To support mental health education and awareness for young people
Most young people with mental health problems are not receiving the help they need. At least 90% of young people aged 15-24 who commit suicide have a diagnosable mental illness. Half of all mental health conditions (such as schizophrenia, bipolar disorder, depression, and anxiety disorders) start by 14 years of age, but most cases are undetected and untreated (WHO {2020} Adolescent Mental Health).
We hope that by delivering factual simple information the messages around mental illness become more about seeking help as a sensible and supportive action, rather than a sign of weakness.
Tell Me About Mental Health is for information purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. If you think you have a mental health problem, seek help as soon as possible.
Although Tell Me About Mental Health has been written by psychologists and the content reviewed by an expert panel, reliance on any information is solely at your own risk.
We all have times when we feel lots of different emotions. Some of them might be happiness and contentment, sadness, anger or anxiousness.

When we feel happy, we want to do happy things.

When we feel sad, we usually don’t want to do much.
We all experience different emotions at different times – but that doesn’t mean we have a mental illness.
Most of us will have times during our lives when we feel contented and times when we don’t.
We call these the different mental health STATES.
We use these symbols (or icons) to learn about the different mental states as we continue.
Our MENTAL HEALTH symbol shows a sunny face wearing a big smile.
Mental health is when we are coping well with the normal stresses in our lives – like writing exams, a school race, a competition.


We feel balanced and good, think clearly, physically healthy, and able to deal with daily challenges. This is also called well-being.

Well-being could be described as how we feel about ourselves and our life.
- It’s a mixture of our emotions
- Our physical health
- Our life satisfaction
- Our relationships with others
Everyone, old and young, can experience good or poor mental wellbeing.
Every aspect of your life influences your state of wellbeing.
Happiness researchers found the following factors enhance a person's wellbeing:
- happy homelife, happy relationships with family
- close friends
- enjoyable community life
- regular exercise
- nutritional diet
- enough sleep
- spiritual or religious beliefs
- fun things to do in spare time
- healthy self-esteem
- optimistic outlook
- realistic and achievable goals
- a sense of belonging, purpose and meaning
- the ability to adapt to change
- living in a safe community
The first step towards keeping mentally healthy is to understand that what is going on in our heads can affect us in our bodies.
A good example:

That funny feeling like butterflies in our tummy when we are worried or nervous.
That is our brain telling us that there is something we should be worried or nervous about. We get butterflies in our tummy when we have these thoughts.
So, the “butterflies” show us that what we are thinking (in our minds) can make us feel something (physical) in our bodies.
Our mental health is linked to our physical health!
Think of how miserable we can feel when we are physically sick.
If we start off by learning to recognise and understand that what we think and feel (our emotions) can affect us physically (our bodies),.
Then we can begin to understand that there are things we can do to that can often help us stay mentally healthy.
We sometimes believe that we need to happy all the time.

This is not possible.
So, let’s talk more about emotions.
We all have thoughts and feelings. These are called emotions.
Everyone has emotions no matter how old or young.
And sometimes those feelings can be really big.

Like anger or sadness. These big feelings are completely normal.
Our feelings are clever, and they often tell us something.
Like if we are sad, it can be our body’s way of telling us that we need to attend to our sadness:
- to talk to someone
- to breathe
- to ask somebody for some comfort or a hug.
So, it’s good idea to learn to listen to our feelings. We need to stop and ask ourselves –
1. What am I feeling?

2. Learn to identify the feeling
Knowing it’s normal to feel hurt (or angry, scared, sad etc)

“I’m feeling so angry!”
3. Try to find ways to understand where that feeling comes from
and then we can think of ways that might make us feel better.
Knowing our emotions and where they come from helps us work out how to respond or behave in different places and situations.
For example:

“My cheeks are hot - I’m feeling angry because my brother took my juice…”
4. Then we get used listening to our feelings and emotions

So instead of getting angry and yelling…

You can think: “No point in getting cross - maybe he was thirsty – I will just get more juice.”
And when learn to work with these feelings and emotions - we can achieve (get) better well-being.

Being kind is a good way to start!
The Second Mental State
Sometimes things can get us down. This is EVERYDAY DISTRESS.
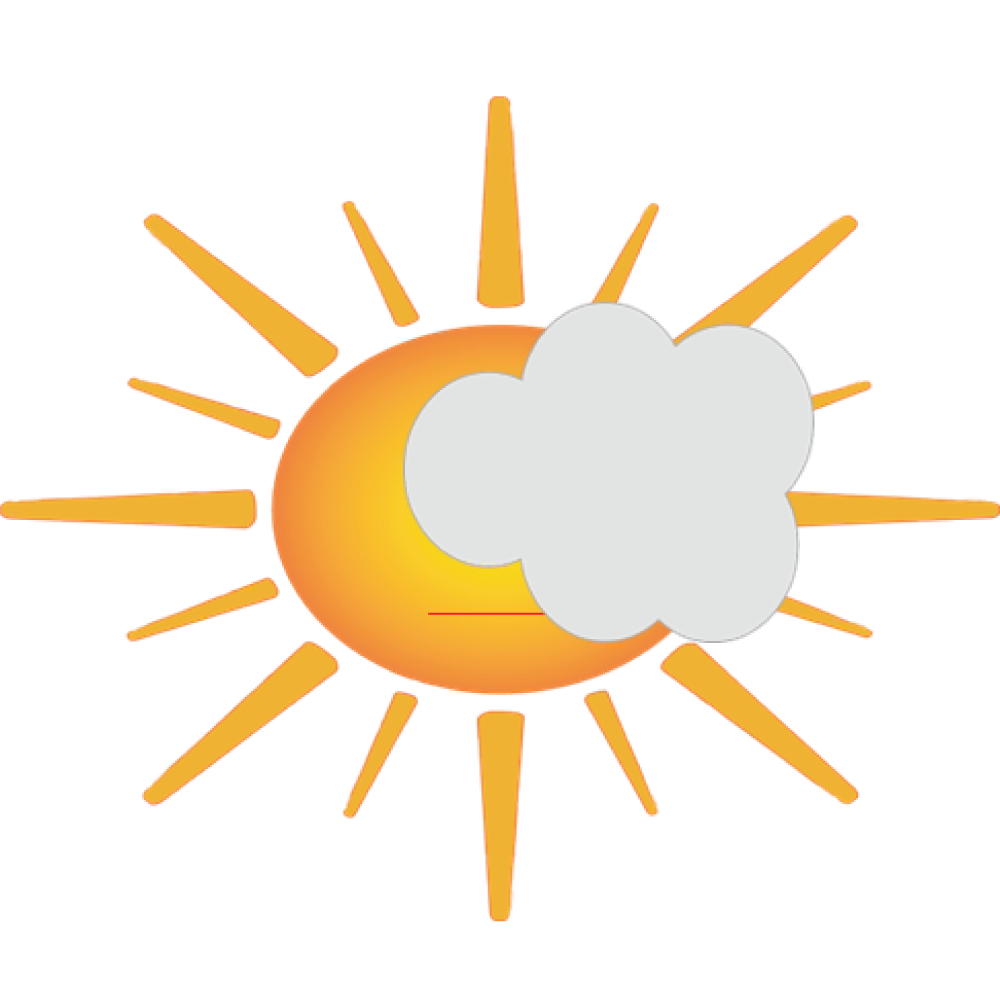
We can see from our EVERYDAY DISTRESS symbol that there’s a small cloud over the sun.
Everyday distress is when your mental health is upset or unbalanced.
We all can have Everyday Distress now and then; mental health goes up and down at different times.

Some causes might be problems with a relationship, or exam anxiety.

We feel upset or stressed.

We look at everyday distress as a feeling of discomfort and tension that comes from stressors (things that stress us).
This feeling of discomfort is a signal to you, from your brain, telling you that you need to adapt to what is happening around you (and it is the basis for adaptation and resilience).
Everyday distress is normal - you don’t need counselling or medicine.

- Use the stress signal - listen to your brain
- Develop new response skills
- Get support from friends, family or a trusted adult
- Exercise
- Get enough sleep
- Stay away from drugs and alcohol
- Learn from your wrong choices to make right ones
1. Learn to Understand your thoughts when something happens.
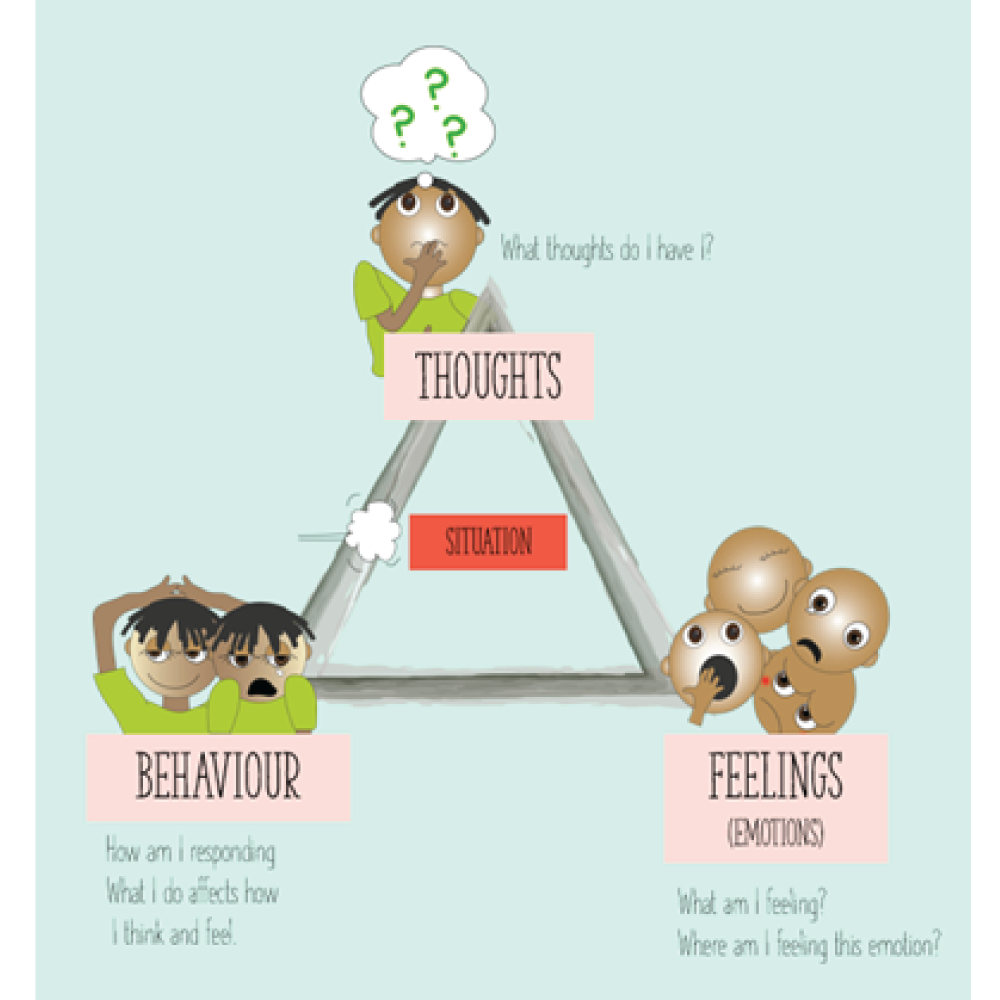
The cognitive triangle illustrates how thoughts, emotions, and behaviours affect one another. This idea forms the basis of Cognitive Behaviour Therapy (CBT).
2. If we do not control our thoughts, they can lead to feelings of distress
3. How do we control our thoughts?
Make a list:
- Write down all the stressful thoughts
- Create thoughts that replace the stressful thoughts
- Read your list often
- Notice when the stressful thoughts pop up
- Replace them with your happy thoughts
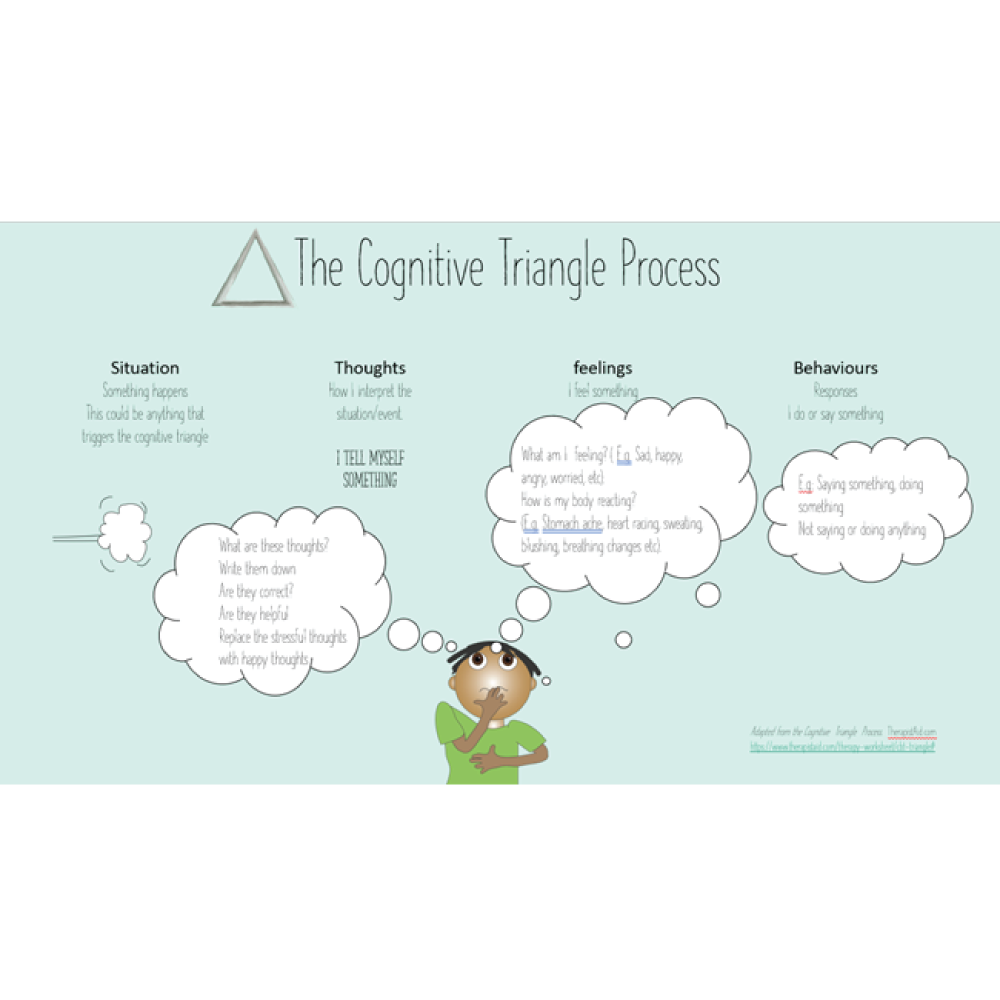
Adapted from the Cognitive Triangle Process. TherapistAid.com
https://www.therapistaid.com/therapy-worksheet/cbt-triangle#
Young people experiencing everyday distress do not require counselling – you are not sick and you do not need treatment. You can learn how to manage the stress response and how to use the stress signal to develop new skills.
You learn these skills naturally by trial-and-error by obtaining advice from friends, parents, teachers, and trusted adults and from other sources (such as the media). You can also use techniques that are part of general health management, such as: exercise, having enough sleep, being with friends and family, eating properly and staying away from drugs and alcohol.
Use the CBT triangle* to learn to understand your thoughts and change them from negative to positive, to help change how you respond to stressors.
Sometimes what you try does not work (for example: instead of studying for an exam you go out and party with friends, instead of getting a good night’s sleep before an exam you try to stay up all night and study) and as a result your stress may increase. But making wrong choices is part of learning how to make good choices. This is a normal part of growing up.
For parents/caregivers:
Remember that everyday distress is normal – your child doesn’t need medical help or counselling.
Reassure your child that everyday distress is a very normal part of life and that without it, nothing would get done.

Encourage your child to:
- Develop new response skills
- Get some exercise
- Get enough sleep
- Stay away from drugs and alcohol
- Learn from their wrong choices to make right ones
The Third Mental Health State
Our symbol has a sad mouth with quite a few dark clouds over the sun.
Mental distress happens when the level of stress is higher, and reactions are stronger and more intense.
Some examples might be:
- someone close to you is very sick
- community violence
- a family divorce
- the illness or death of someone you love

You might sometimes show noticeable difficulties in everyday functioning - at school and outside of school.

When you are (more seriously) mentally distressed - the stressors (things that are stressing you) are much stronger than everyday stressors.
Ask for help. Professional support or help can be very helpful at these times.
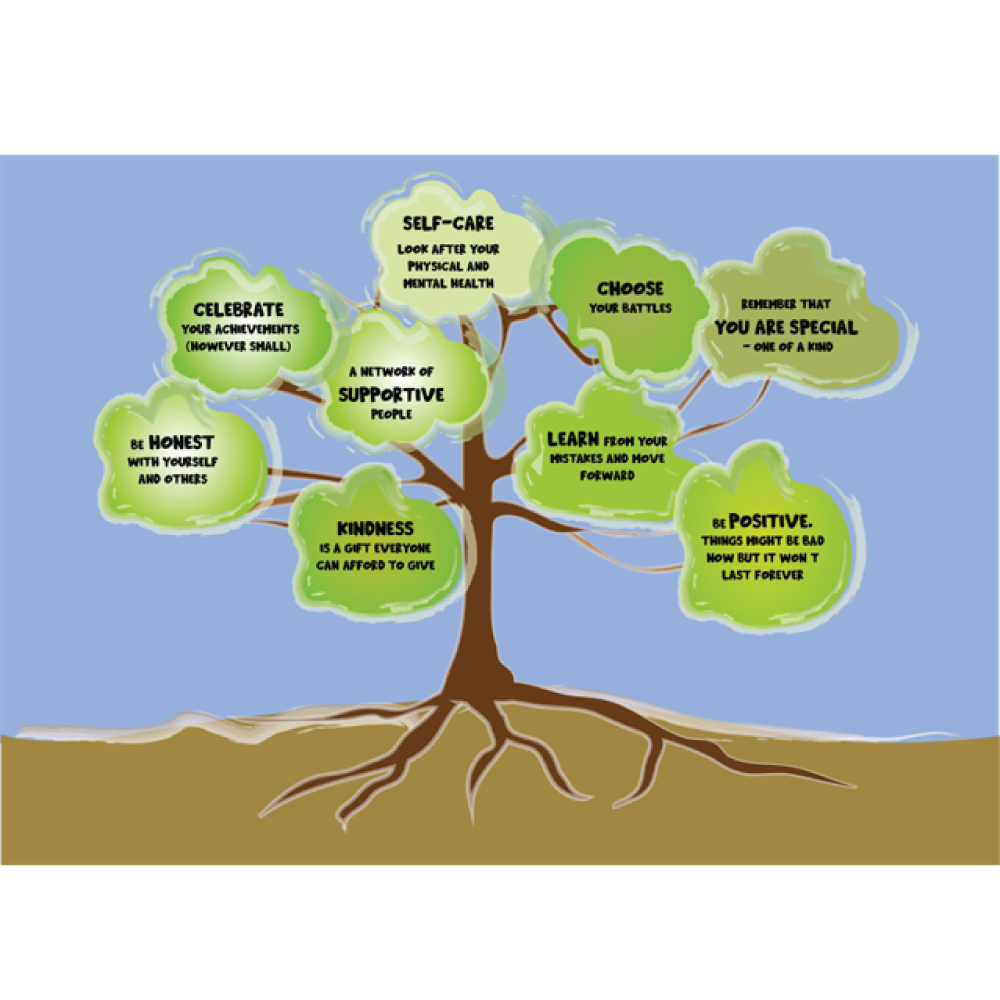
Build your resilience! (Resilience is becoming strong, healthy or successful again after something bad happens)
Sources of Resilience:
YOU can also find out about:
- Support groups
- Counselling

- Group counselling
- CBT (Cognitive Behavioural Therapy)
- DBT

- Friendship bench
There are many different approaches to improving mental health. The most common are:

CBT believes that mental health problems have to do with the way that we think about things. It aims to replace harmful negative thoughts with more positive ones.
Helps with obsessive compulsive disorder, anxiety, depression, building self-esteem, phobias.
The best-known cognitive behavioural therapies are:
- Mindfulness based cognitive therapy (MBCT)
Helps you to pay attention to your thoughts and feelings without judgement. It uses meditation, yoga, and other approaches. Helps with anxiety, depression, and bipolar disorder. - Dialectical Behaviour Therapy (DBT)
Helps you to develop problem-solving skills to cope better with stress. Helps with Borderline personality disorder, bipolar disorder, substance use disorders, attention deficit hyperactivity disorder, eating disorders and post-traumatic stress disorder. - Acceptance and Commitment Therapy
Helps you to think about deeper feelings so that you can start to make the changes needed to improve wellbeing. Helps with depression, social anxiety, stress, obsessive compulsive disorder, and substance use disorders. - Rational Emotional Behaviour Therapy
Helps you to recognise negative and irrational thoughts and replace them with healthier thoughts and beliefs. Helps with anxiety, guilt, depression, anger, eating disorders, aggressive behaviour.

These approaches help you get to know yourself better by exploring the connections between what you are feeling now and past experiences.
Helps with depression and anxiety.
Some of the better-known psychoanalytical approaches include:
- Ego-state Therapy
Helps to create harmony between different parts of the self to create a balance. Helps with trauma, depression, phobias, and anxiety. - Humanistic Therapy
Is about helping people to become what they are capable of being. One well-known approach is client-centred therapy where the therapist guides the journey of self-discovery and gives support in the search for answers. Another is existential therapy, which helps a person to find meaning and purpose in life by building self-awareness and self-respect. Helps with depression, post-traumatic stress disorder and substance use disorders. - Integrative or Holistic Therapy
This approach looks at the relationship between mind, body and spirit and helps a person to understand how difficulty in one area can affect other areas. Helps with trauma, anxiety, and depression.
- Eye Movement Desensitisation and Reprocessing (EMDR)
where a therapist guides you to remember a traumatic event whilst directing you to move your eyes in a certain way. Helps with post-traumatic stress disorder, and trauma related distress.
- Art Therapy
Weaves psychotherapy and creativity into an approach that allows people to explore their emotions and thoughts through expressive therapies like art, dance, and music therapy. Helps with anxiety, depression, autism, and other developmental conditions, eating disorders, high stress levels, traumatic brain injury, post-traumatic stress disorder.

- Support Groups
Support groups bring together people who are going through or have gone through similar experiences. For example, this common ground might be mental health challenges, chronic medical conditions, addiction, bereavement or caregiving. A support group provides an opportunity for people to share personal experiences and feelings, coping strategies, or first-hand information about diseases or treatments.
For many people, a health-related support group may fill a gap between medical treatment and the need for emotional support. A person's relationship with their doctor or other medical personnel may not provide emotional support, and a person's family and friends may not understand the impact of a disease, disorder or treatment. A support group among people with shared experiences may function as a bridge between medical and emotional needs.
- Friendship Bench approach
Provides sustainable community-based psychological interventions that are evidence based, accessible and scalable. Their mission is to get people out of ‘kufungisisa’ - depression & anxiety - by creating safe spaces and a sense of belonging in communities to improve mental wellbeing and enhance quality of life.

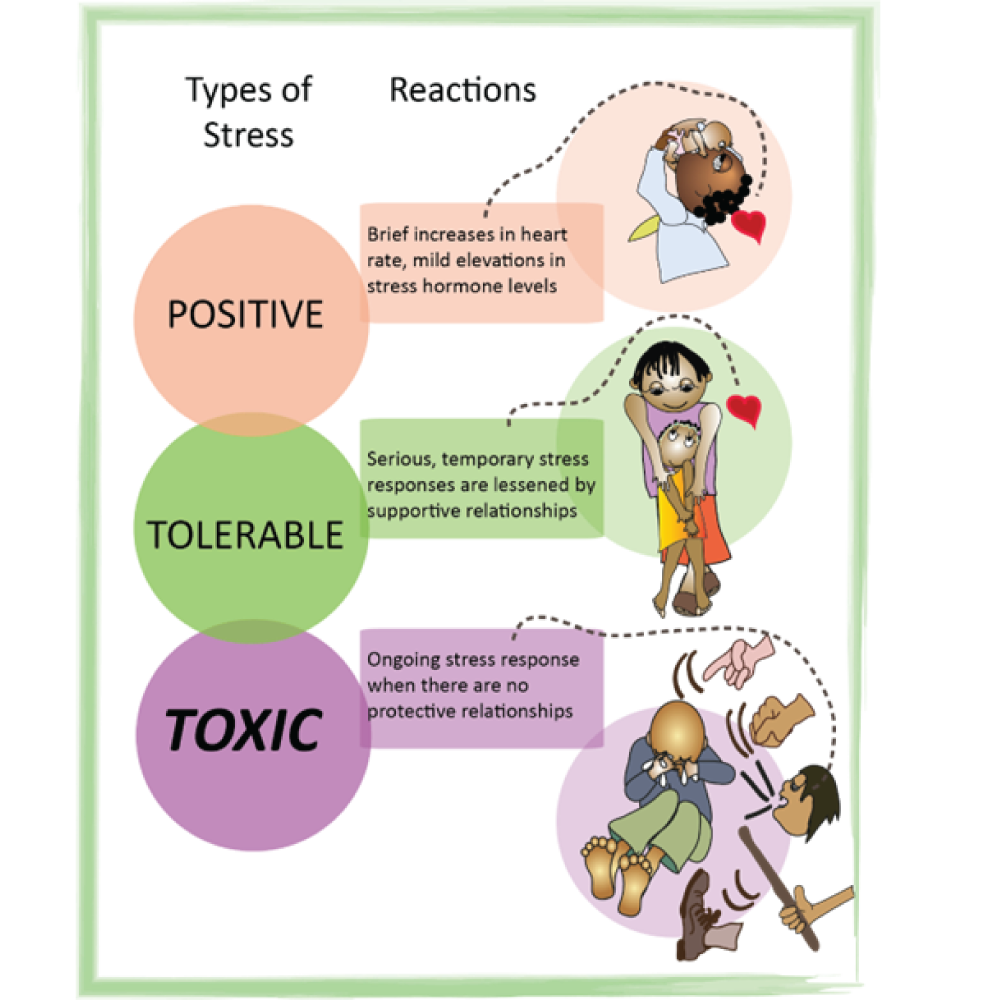
The word STRESS is the FEELING of being overwhelmed or unable to cope with mental or emotional pressure.

Stressor
Stress is not a sickness or a diagnosis. It’s a process that happens over time and the level of stress we feel often depends on our attitude to that stressor (The thing that is stressing us). There is a big difference between stressors and stress

Stress
An important aspect of stress is its effect over time (duration).
Stress that continues for very long periods (chronic) can lead to damaging changes in the body.
Chronic stress eventually affects the immune system (the body’s defence against infection) making it more vulnerable to disease.
Stress is a natural physical (body) and mental reaction (emotional) to life experiences.
Everyone experiences stress from time to time. This stress response also happens in not–so-serious circumstances. Everyday things like work, school, exams and family can cause stress. Serious life events such as an illness diagnosis, war, or the death of a loved one can trigger stress too.
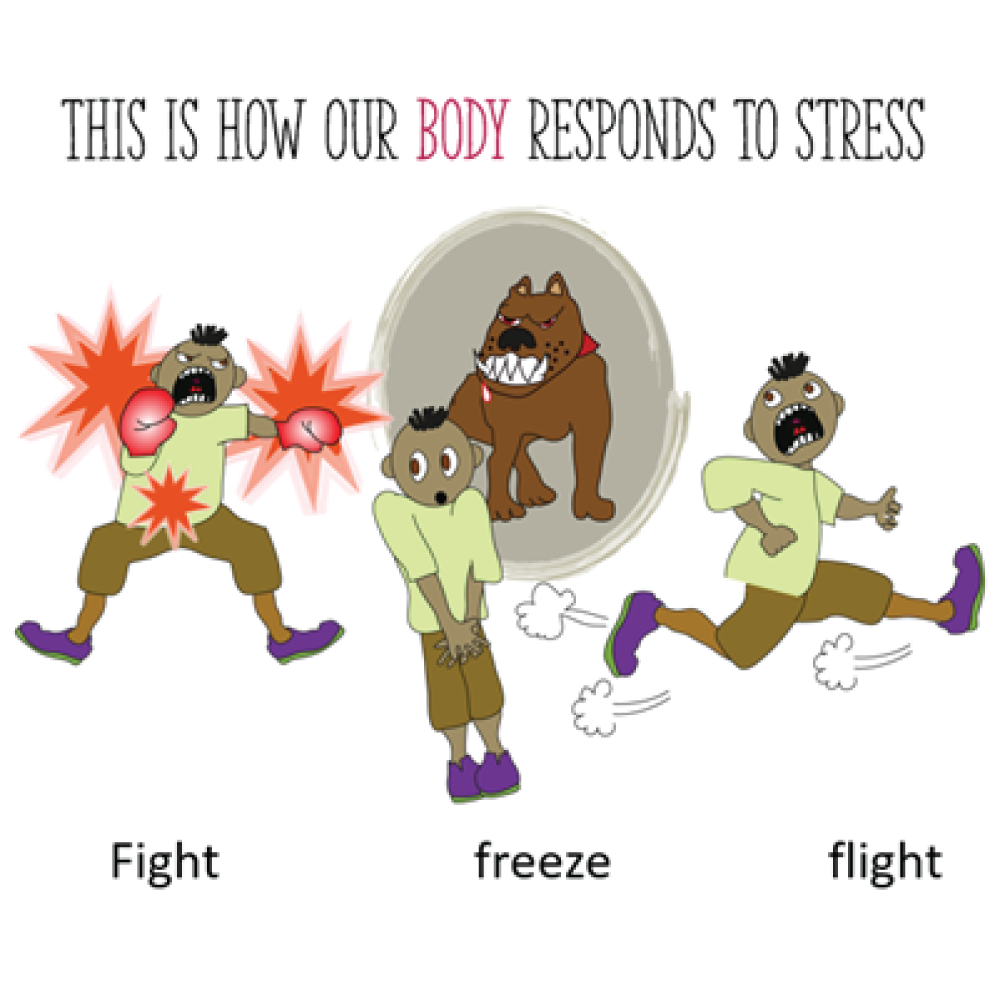
Your body responds to stress by releasing hormones that increase your heart and breathing rates and gets your muscles ready to respond. This is a survival response, designed by nature to protect your body in an emergency by preparing you to react quickly and get out of danger so you can (fight) the danger, numb out the horror (freeze), or get out of danger as fast as you can (flee).
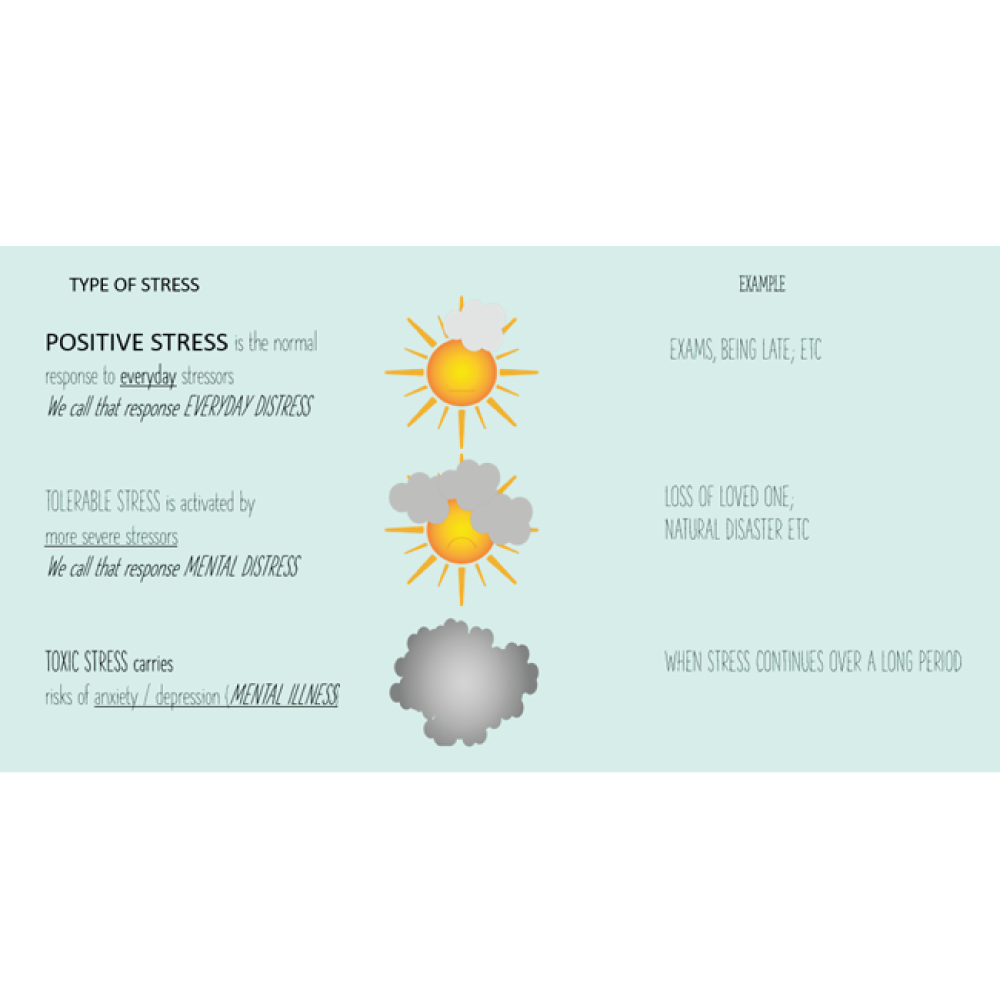
Here we can see some reactions to different types of stress:
How does our brain responds to stress?
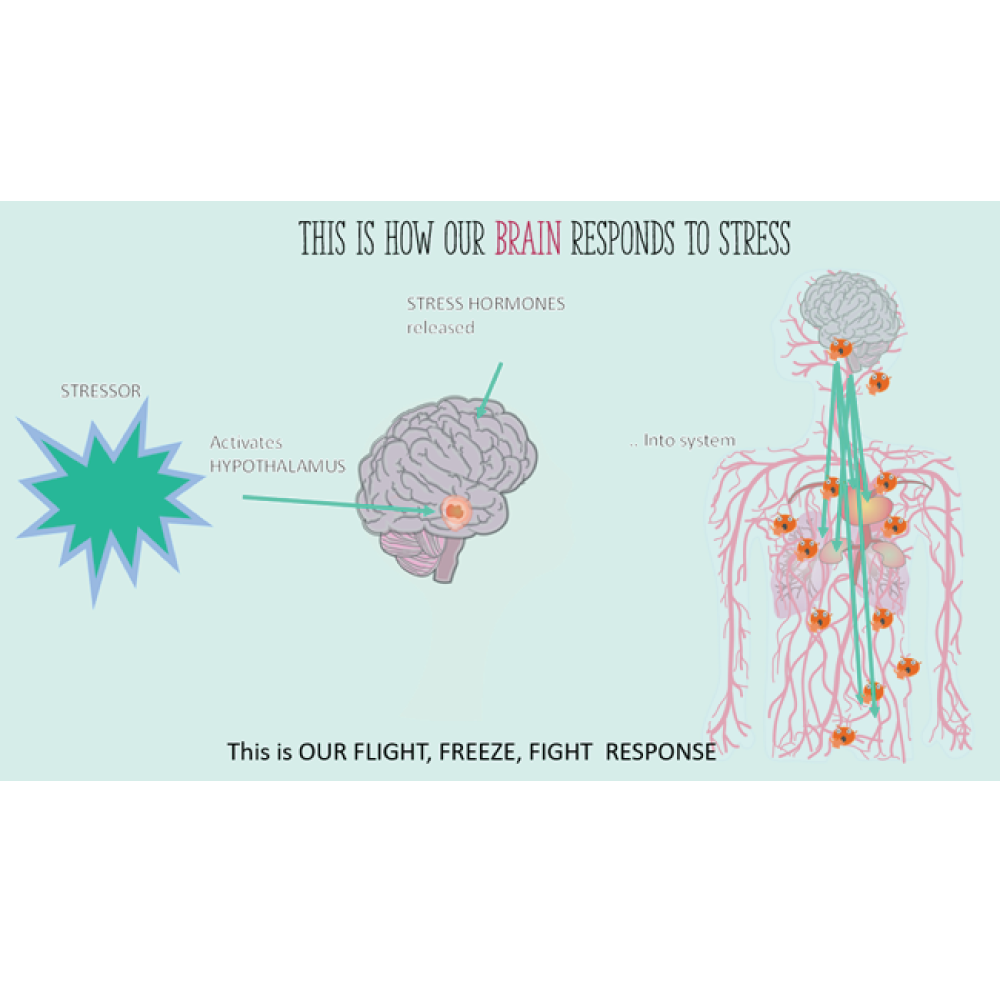
How does our body respond to stress?
In the case of a stressful event, your body responds to stress by releasing hormones. These hormones (or chemical messengers):
- increase your heart and breathing rates
- get your muscles ready to respond
This is a survival response, designed by nature to protect your body in an emergency by preparing you to react quickly and get out of danger so you can (fight) the danger, numb out the horror (freeze), or get out of danger as fast as you can (flight).
BUT these responses are not meant to be working all the time without switching OFF
The responses are supposed to stop once the stressor (threat or harmful event) is over.
We should go back to our normal way of functioning that is not on guard or over alert.

All the parts of our body (digestive, immune, hormonal, muscular, heart, blood vessels, brain, etc.) do not want to live in a constant state of fight, flight, or freeze.

It is like keeping the motor running when the car should be switched off.

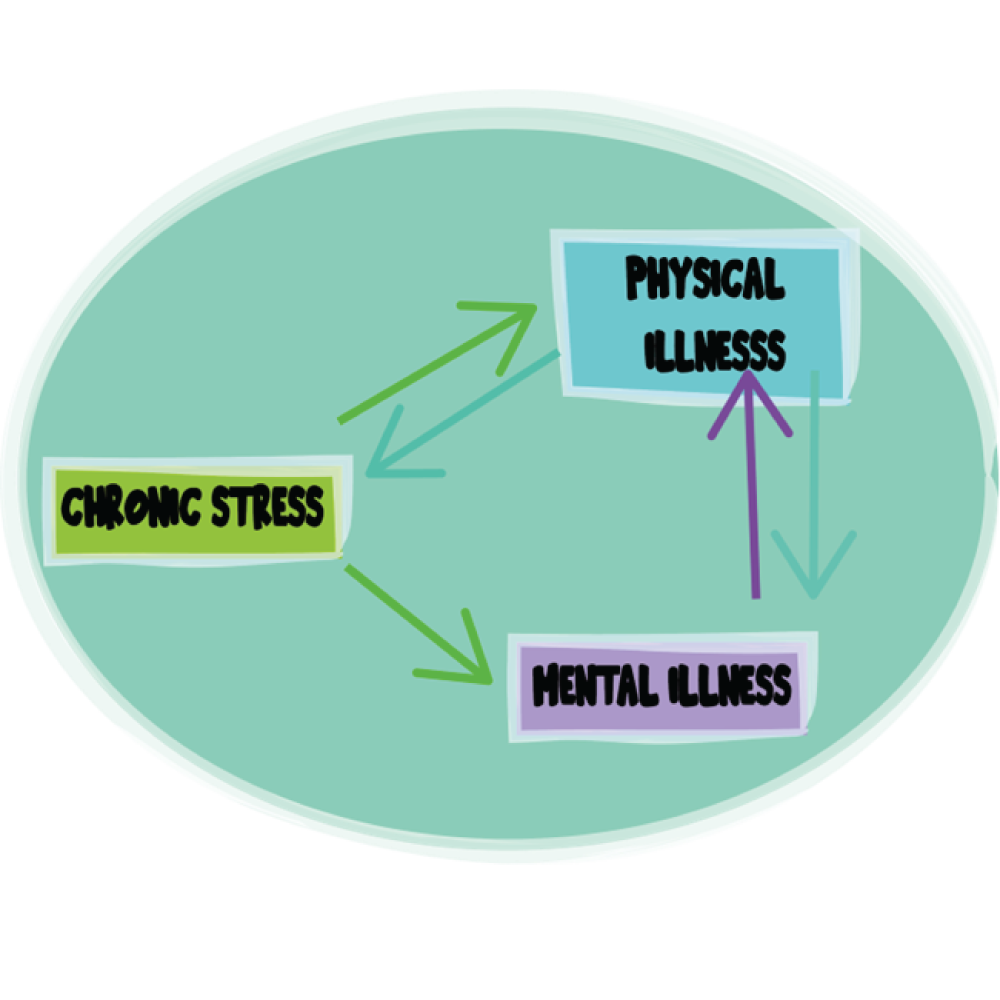
Stress, (especially the kind that doesn’t get switched off) can cause many kinds of illnesses.
These can be mental and/or physical illnesses (of the mind and/or of the body).

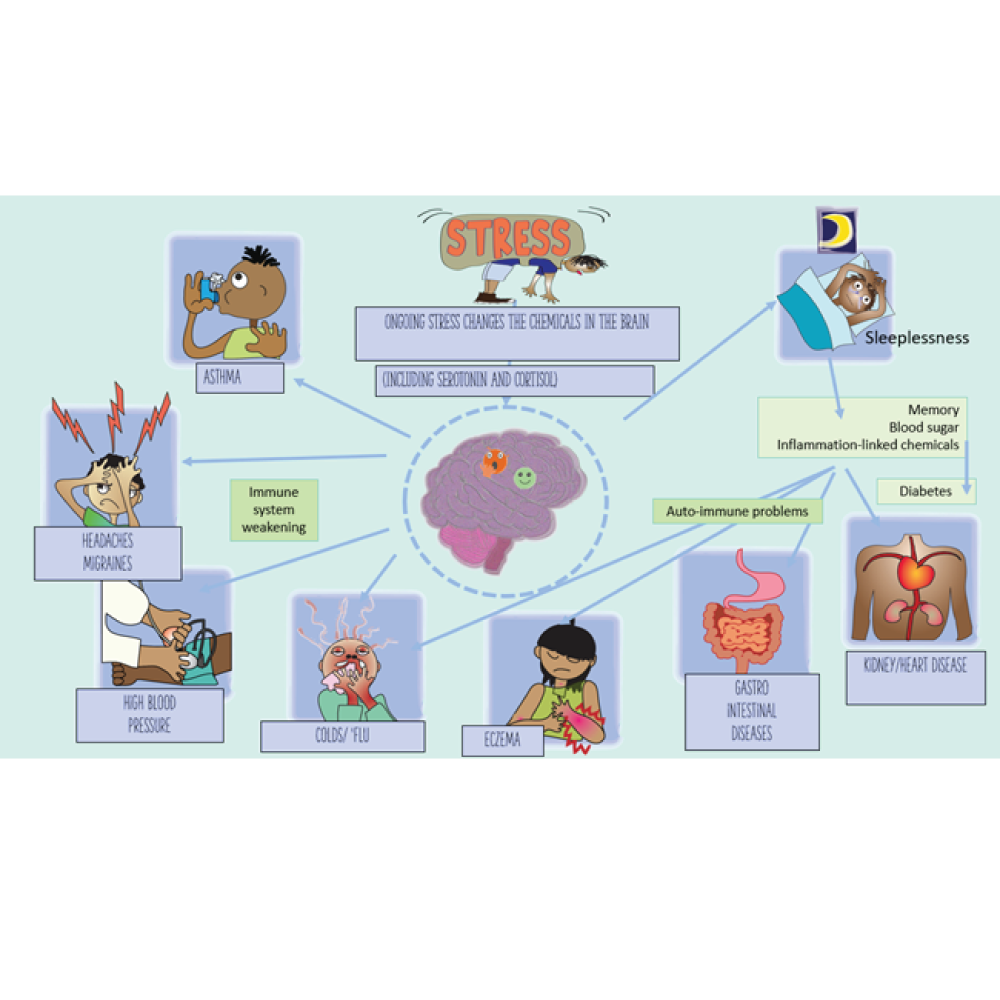
Stress can cause physical and mental illness, but illness can cause stress too.
We will not be able to recognise mental illness, but knowing the basic mental health states helps us to use the correct language for everyday and mental distress which is different from the language used in mental illness.
For example:
Sad, unhappy, and disappointed, are not the same as DEPRESSION
Worrying feeling nervous and apprehensive are not the same as ANXIETY
Feeling upset, inconvenienced and angry is not TRAUMA (Physical abuses, neglect, violence and living in a war zone, are!)
Having a bad day is not the same as Depression
Being organised is not the same thing as OCD
Being hyperactive is not the same as ADHD
Feeling upset is not the same as PTSD
Exam stress is not the same as Anxiety Disorder
A ‘split personality’ is not Schizophrenia
Feeling afraid is not the same as Panic Disorder
Being moody is not the same as Bipolar Disorder
Using the word Depression when we mean upset is confusing and unhelpful in advancing understanding and communication.
Language must be clear and convey what it is intended to mean.
Young people need to understand the differences. They need to be clear about the language they use to tell others how they are feeling. We need to use language in the same way.

Description of depression -
SADNESS

Actual feelings of people with depression -
WORTHLESS, ALONE, EXHAUSTED, ISOLATED, OVERWHELMED
The Fourth Mental State
Our symbol is a big dark cloud covering everything.
A mental disorder (or mental illness) is very different from everyday distress or the more serious mental distress.
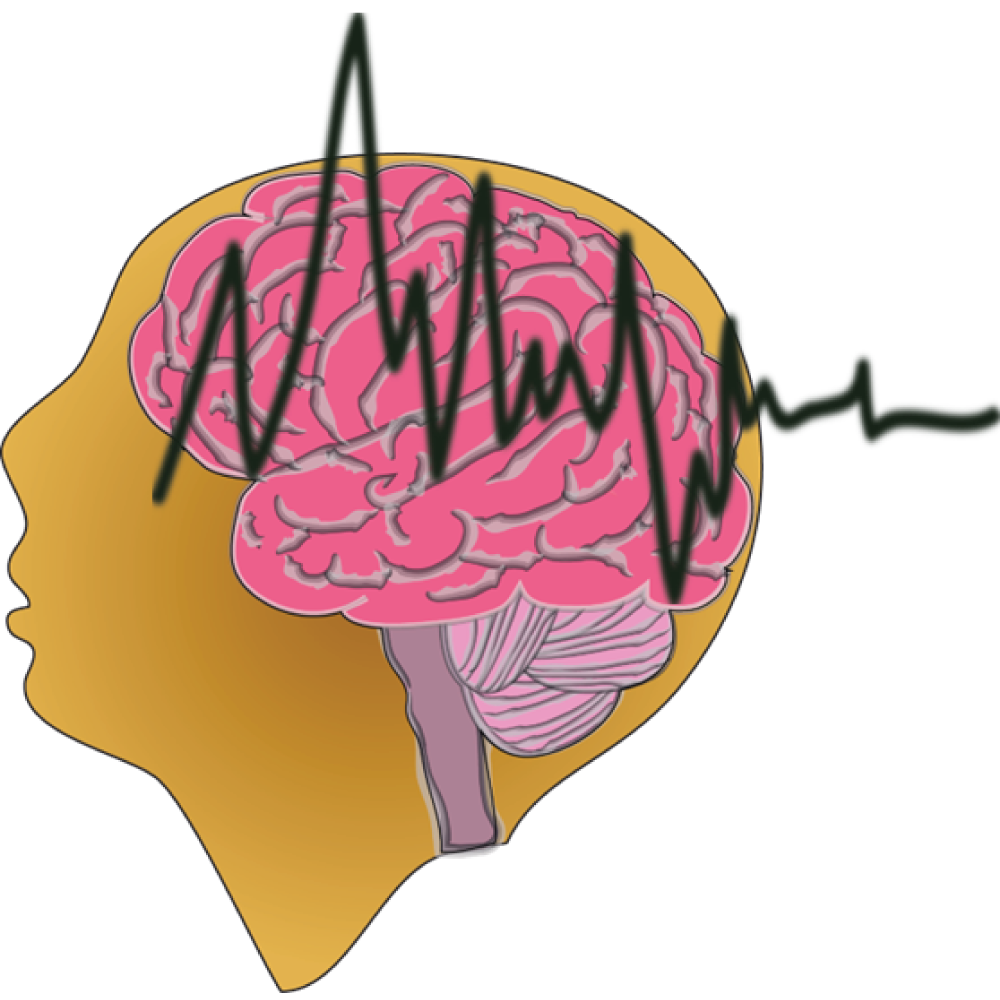
Mental illness is when changes happen in the brain.
Mental illnesses are MEDICAL illnesses, in the same way that diabetes is a disturbance in the pancreas, mental illnesses are disturbances of usual brain function.
Whenever you feel unsure - ask for help
Our brain is like our own onboard computer that controls the body's functions.
Our nervous system is like a network of electrical circuits that relays messages to parts of our body.
When you touch something hot, you quickly move your hand away - your brain sending a message before you burn yourself.

This is one example of how our brains are connected to our bodies.
We all have times when our mood is happy, sad, or irritable.
We need a mental health professional to find out if a person is experiencing is more than a mood swing.

For a start:
- you will be asked about your thoughts, feelings, and behaviour and how long these have been causing you distress.
- there might be a blood test needed to check if there could be a physical condition that is causing the problem.
- Doctors use a special manual that is made up of a list of symptoms that are common to various disorders.
- If your symptoms closely match those on the official list, they will make a diagnosis.
So, quite a few things need to happen before a mental health disorder is diagnosed (by a health care professional)
Because these disorders affect a how you function at home, at school and in relationships, each step is important for the right diagnosis and treatment.
- Mood changes - Rapid or dramatic shifts in emotions or depressed feelings
- Sleep or appetite changes - Dramatic sleep and appetite changes or decline in personal care
- Withdrawal - Recent social withdrawal and loss of interest in activities previously enjoyed
- Drop in functioning - An unusual drop in functioning, at school, work or social activities, such as quitting sports, failing in school or difficulty performing familiar tasks
- Problems thinking - Problems with concentration, memory or logical thought and speech that are hard to explain
- Increased sensitivity - Heightened sensitivity to sights, sounds, smells or touch; avoidance of over-stimulating situations
- Apathy - Loss of initiative or desire to participate in any activity
- Feeling disconnected - A vague feeling of being disconnected from oneself or one’s surroundings, a sense of unreality
- Illogical thinking - Unusual or exaggerated beliefs about personal powers to understand meanings or influence events; illogical or “magical” thinking, typical of childhood in an adult
- Nervousness - Fear or suspiciousness of others or a strong nervous feeling
- Unusual behaviour - odd, uncharacteristic, peculiar behaviour
- Changes in appearance - sudden weight loss, brown teeth, etc
Whenever you feel unsure - ask for help.
Mental illnesses (or disorders) are not a choice.
They are medical conditions that affect the brain and come from a complicated mix of:
- a person’s genes (inherited from their family),
- their environment,
- and their personality.
Like diabetes, cancer and heart disease, mental disorders are caused by a combination of factors.
Mental illnesses can be managed – much like physical illnesses.

A young person with depression is likely to feel sad and empty.
They might lose interest in things that they enjoyed doing before. They may feel irritable and have angry outbursts or become withdrawn.
There are different types of depression.
Major depression is the term that is used to describe the most common type of depression. Symptoms can range from mild, to moderate and severe.
Depression is caused by a chemical imbalance in the brain.
This imbalance is caused by:
- environmental (what is around us)
- psychological (our feelings)
- biological (genetic factors)
Name: DEPRESSION (Mood disorder)
Possible Signs:
- Feelings of sadness, tearfulness, emptiness, or hopelessness
- Anxiety, agitation or restlessness
- Angry outbursts, even over small matters
- Feeling misunderstood and extremely sensitive
- Loss of interest or pleasure in most or all normal activities
- Social withdrawal
- Inability to return calls, messages, emails
- Staying in bedroom/isolating
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy
- Poor self-care
- Failure to do chores/participate in housekeeping tasks
- Not doing homework
- Missing class
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Unexplained physical problems, such as back pain or headaches
- Slowed thinking, speaking, or body movements
- Feelings of worthlessness or guilt
- Fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering things
Ask for help – the sooner you get treatment, the better.
Cause:
A chemical imbalance in the brain.
Caused by:
- environmental (what is around us)
- psychological (our feelings)
- biological
- genetic factors Family history (genetic)
- psychosocial stressors
Treatment:
Medication
Psychotherapy
CBT, DBT or combination treatment
TIPS:
Be kind to yourself
Take small steps
Try something new
Challenge negative thoughts
Practice mindfulness
Connect with others
Suicide Crisis Help line
0800 567 567
MOST people respond well to treatment. The sooner you get treatment – the better.

Mental health challenges are experienced by pregnant teenagers as a consequence of adolescent pregnancy itself, as well as other factors such as poverty, intimate partner violence, family rejection, social isolation, stigma, and in some cases chronic illnesses.
These stressors lower resilience and make depression more likely.
NAME: POST-PARTUM DEPRESSION (PPD)
or Post-Natal Depression (PND)
PPD is more common among adolescent mothers than adult mothers.
Possible signs:
- Feelings of sadness, tearfulness, emptiness, or hopelessness
- Anxiety, agitation, or restlessness
Additional symptoms of postpartum depression include:
- difficulty bonding with your baby
- overwhelming fatigue
- feeling worthless
- anxiety
- panic attacks
- thinking of harming yourself or your baby
- difficulty enjoying activities you once did
Causes/risks:
When pregnancy happens at a time when the adolescent brain is rapidly changing, the additional physical, emotional, and mental demands that pregnancy brings can be overwhelming.
Poverty, abandonment by the partner, family isolation, and gender-based violence all contribute to possible depression after the baby is born (and before).
Adolescents face higher risk of complications of pregnancy and childbirth including pre-eclampsia/eclampsia and obstructed labour.
Treatment:
Medication
Psychotherapy
CBT, DBT or combination treatment.
Support from community, family and friends
There is a big difference between baby blues and post-partum depression
The sooner you get treatment – the better.
SADAG Mental Health Helpline
0800 456 789
SMS 31393
Up to 80% of new mothers get what’s called the “baby blues”. These are short-term dips in mood caused by all of the changes that come with a new baby. You’re likely to feel better by the time your baby is 1 or 2 weeks’ old.
Treatment is usually lifelong and often involves a combination of medications and psychotherapy. Treatment can help, but this condition can't be cured. Chronic: can last for years or be lifelong. Requires a medical diagnosis.
With Bipolar Disorder, a person’s mood and energy levels will swing between being very happy or ‘up’ with more energy than usual (manic episode) and very sad or ‘down’ with little energy (depressive episode). There is no single cause of bipolar disorder.

The exact cause of bipolar disorder isn’t known, but a combination of genetics, environment and altered brain structure and chemistry may play a role.
Manic episodes may include symptoms such as high energy, reduced need for sleep and loss of touch with reality.
Depressive episodes may include symptoms such as low energy, low motivation and loss of interest in daily activities.
Mood episodes last days to months at a time and may also be associated with suicidal thoughts.
Treatment is usually lifelong and often involves a combination of medications and psychotherapy. Treatment can help, but this condition can't be cured – it is Chronic: can last for years or be lifelong.
Requires a medical diagnosis.
Name: BIPOLAR DISORDER (MOOD DISORDER)
Signs/symptoms:
Elevated mood:
- The person feels extremely high, happy and full of energy. The experience is often described as feeling on top of the world and being invincible.
- Increased energy and over-activity.
- Reduced need for sleep.
- Irritability – The person may easily and frequently get angry and irritable with people who disagree or dismiss their sometimes-unrealistic plans or ideas.
- Rapid thinking and speech – thoughts are more rapid than usual. This can lead to the young person speaking quickly and jumping from subject to subject.
- Lack of inhibitions – This can be the result of the person’s reduced ability to foresee the consequences of their actions. For example, spending large amounts of money buying things they don’t really need.
- Grandiose plans and beliefs – It is common for people experiencing Mania to believe that they are unusually talented or gifted or are kings, movie stars or political leaders.
- It is common for religious beliefs to intensify or for young people with this illness to believe they are an important religious figure.
- Lack of insight – A person experiencing Mania may understand that other people see their ideas and actions as inappropriate, reckless or irrational. However, they are unlikely to recognise the behaviour as inappropriate themselves.
- Psychosis – Some people with mania or depression experience psychotic symptoms such as hallucinations and delusions.
Depression:
Common symptoms include varying degrees of the following:
- Lowered mood – Many people with Bipolar Mood Disorder experience depressive episodes. These are similar in nature to those experienced by people who have depression.
- Withdrawal – The person loses interest and pleasure in activities they previously enjoyed. They may withdraw and stop seeing friends, avoid social activities and cease simple tasks such as shopping and bathing.
- Loss of appetite or weight – They may become overwhelmed by depression, lose their appetite, lose weight, become unable to concentrate, and may experience feelings of guilt.
- Feelings of hopelessness – Some attempt suicide because they believe life has become meaningless or they feel too guilty to go on.
- Delusions – Others develop false beliefs (delusions) of persecution or guilt or think that they are evil.
Cause:
No single cause
Genetic factors
Family history
Treatment:
Medication
Psychotherapy or combination treatment
Mental illnesses are not always accepted in communities and sometimes people with mental health conditions are hidden away because the family is ashamed.
Plea to the community!
Take people with mental health issues to a health facility, support them and encourage them to take their medication.
With access to appropriate treatment and support, most young people with Bipolar disorder lead full and productive lives.
Treatment is usually lifelong and often involves a combination of medications and psychotherapy. Treatment can help, but this condition can't be cured. It is Chronic: can last for years or be lifelong. Requires a medical diagnosis.
It is not unusual to feel anxious about exams or going on a date. But an anxiety disorder is much more than just a passing fear or worry.

People with an anxiety disorder feel anxious all the time. Instead of going away, their anxiety just gets worse until it begins to interfere with everyday life.
There are different types of anxiety disorders:
- social anxiety disorder,
- generalised anxiety disorder
- panic disorder.
A person who has panic attacks will not necessarily develop a panic disorder. Even though they are not life-threatening, panic attacks often come out-of-the-blue and can be very scary. There are many different signs of a panic attack, but these usually go away after a few minutes.

Name: ANXIETY DISORDERS

Generalised Anxiety Disorder:
Excessive, unrealistic worry with no reason
Panic Disorder:
Feelings of intense discomfort and fear
Associated with physical symptoms such as:
- sweating
- shaking
- chest pain
- chills or feeling hot
Social Anxiety Disorder:
Self-conscious about everyday situations; fears humiliation, embarrassment or judgement.
Anxiety can make you feel:
- tense or nervous
- a sense of dread
- like you can't stop worrying or bad things will happen
- worried that people are angry or upset with you
- like the world is speeding up or slowing down
- low mood
Anxiety can cause you to ruminate - think a lot about bad experiences or go over and over a situation in your mind.
Panic Attacks are a type of fear response, and they can be very scary.
You might feel:
- your heart racing
- faint or dizzy
- nauseous (feeling sick)
- very hot or very cold
- pain in your chest or stomach
- you can’t breathe
- like your legs are shaky, like jelly
- like you’re losing control
Caused by:
No single cause
Genetic factors
Family history
Treatment:
Medication
Psychotherapy, or combination treatment
People with anxiety disorders respond well to a combination of interventions
TIPS:
Go for a quick-paced walk
Clean and organise the house/ room
Do something in nature (grow veggies, gardening, birding)
Get involved in a hobby
Remember that recovery is a journey, and it won't always be uncomplicated.
Eg: you might find it more helpful to focus on learning more about yourself and developing different ways to cope, rather than trying to get rid of all your symptoms.
The sooner you get treatment, the better.
Try the 54321 Trick if you’re feeling anxious.
Find:
- five things you can see
- four things you can touch
- three things you can hear
- two things you can smell
- one thing you can taste
Hopefully sitting quietly and breathing deeply will help you feel a bit calmer.
Some signs are obsessive unwanted thoughts and urges (obsessions) that won’t go away.
To get rid of these distressing thoughts certain behaviours are repeated over and over (compulsions).
A person is diagnosed with OCD when the obsessive-compulsive cycle gets in the way of day-to-day functioning.
Name: OBSESSIVE COMPULSIVE DISORDER (OCD)
Symptoms:
OCD often centres on themes such as a fear of germs or the need to arrange objects in a specific manner.
Obsessive thoughts and worries about:
- Health issues (germs, poisons, body fluids etc.)
- Losing control or acting on impulses
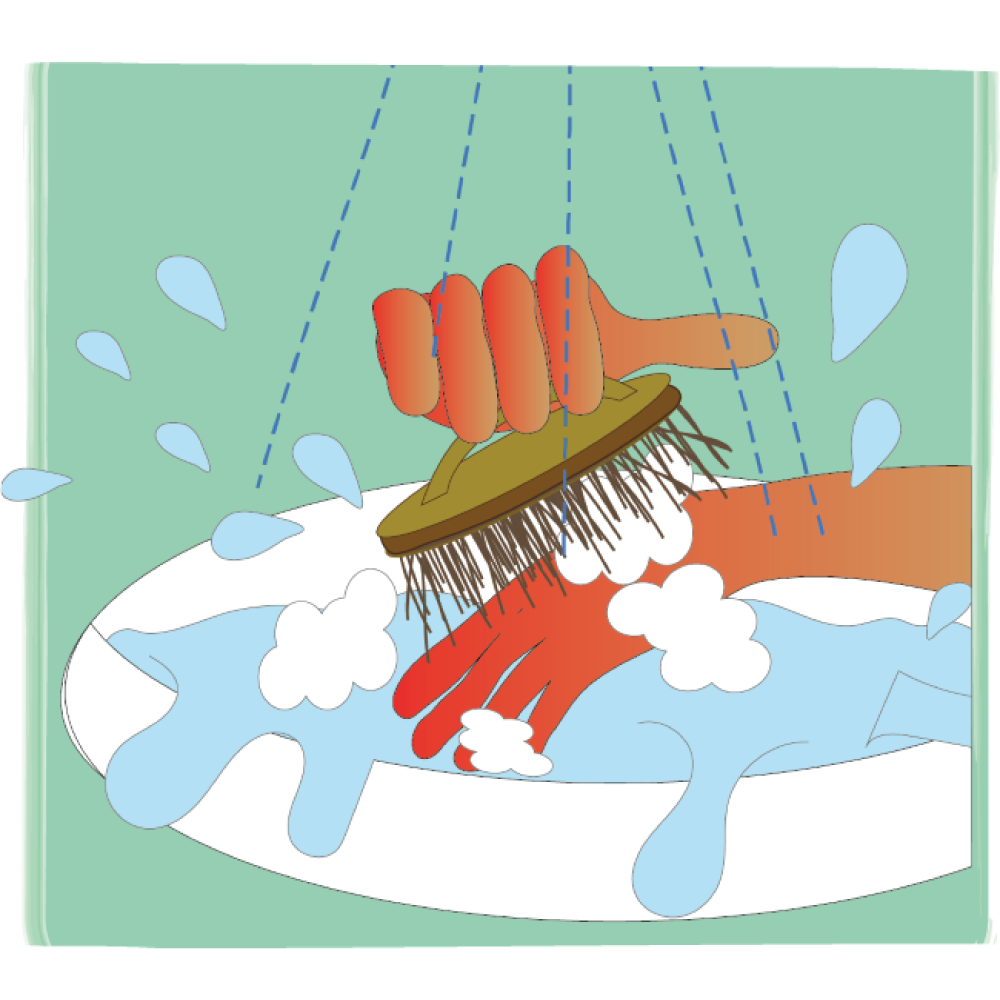
Compulsions – repeating rituals like:
- Counting
- Washing
- Cleaning rooms or items multiples times
- Washing body parts over and over
Caused by:
No single cause
Genetic and environmental factors
Treatment:
Medication
Cognitive Behavioural Therapy
Exercise and activities that require intensive concentration may also help.
Obsessions and compulsions can take over your life and leave you feeling helpless. There are things you can try to help manage your OCD and improve your wellbeing. Remember that different things work for different people at different times.
This disorder usually starts in childhood and can continue into adulthood.
A person with ADHD is on the go all the time and can act without thinking (impulsive) or finds it very hard to pay attention.

SYMPTOMS:
On-the-go all the time
Difficulty paying attention
Restlessness
Daydreaming
Slow to complete tasks
Impulsivity
Inattention
Forgetfulness
Poor time management
Poor organisational skills
Poor listening skills
Lack of focus
Low frustration tolerance
Poor social skills

Anxiety and adhd have some common symptoms.
Average age diagnosed: 7 years
Symptoms shown from 3 years
Risk Factors:
Mainly genetic but there may be other risks such as traumatic birth process, toxins, or brain injuries.
Girls may be more likely to display inattentive symptoms, like daydreaming or losing things, whilst boys may display more hyperactive-impulsive behaviours, such as fiddling or disturbing others.
Treatment:
Medication and therapy (CBT)
Support groups, social skills training are other useful interventions
A young person with Conduct Disorder will have problems following rules and can behave in a way that causes harm to themselves and others. They may lie, steal, or become aggressive. Conduct disorders usually begin between the ages of 10-19 years and have different causes.

Name: CONDUCT DISORDERS
Behaviour and emotional problems
Possible signs:
Won’t follow rules
Disregard for others
Aggressive behaviour
Destructive behaviour
Deceitfulness
Physically violent behaviour
More common in boys
Usually starts in late childhood or early teens
Causes/risk factors:
Environment (abuse, traumatic experience, substance abuse, inconsistent parenting)
Brain defects or injuries
Inherited
Psychological
Social
Treatment:
Therapy - and medication for symptoms
Nurturing, supportive, and consistent home environment with a balance of love and structure may help reduce symptoms and prevent episodes of disturbing behaviour.
A dangerous, very scary, or shocking event can result in Post-Traumatic Stress Disorder (PTSD). With this disorder a person will re-live a traumatic experience and feel stressed and frightened even if there is no longer any danger. PTSD can develop at any age and can be caused by serious events like witnessing or experiencing physical or sexual assault, abuse or an accident.

Name: POST-TRAUMATIC STRESS DISORDER
Not recovering after experiencing or seeing a terrifying event

Possible signs:
Nightmares
Flashbacks (reliving the event mentally)
Anxiety
Depressed mood
Heightened reactivity to stimuli
Avoiding places or situations that bring back the trauma
Pain
Sweating
Nausea
Trembling
Causes/risk factors:
Witnessing or experiencing a traumatic event
Accident
Violence
Childhood physical violence
Assault
Threatened with a weapon
Threatened death
Sexual violation
Treatment:
Different types of Psychotherapy
Medications to manage symptoms
Condition may last months or years.
Triggers can bring back intense, vivid, memories of the trauma.
Not everyone will experience PTSD after trauma
Symptoms don’t start straight away
Symptoms don’t start straight away
Caregivers can develop symptoms too
EATING DISORDERS
These include:
ANOREXIA NERVOSA and BULIMIA NERVOSA
A young person with an eating disorder will be obsessed with food, their weight, and their body. They might starve themselves, over-eat (binge) and then vomit, or over-exercise to avoid weight gain. Eating disorders can be serious and may be life-threatening.

Name: ANNOREXIA NERVOSA
People with Anorexia Nervosa have a distorted body image, with an unnecessary fear of being overweight.
Symptoms include trying to maintain a below-normal weight through starvation or too much exercise.

Medical treatment may be required to restore normal weight. Talk therapy can help with self-esteem and behavioural changes.

Physical signs/ symptoms of anorexia may include:
Extreme weight loss
Not making expected developmental weight gains
Thin appearance
Abnormal blood counts
Fatigue
Insomnia
Dizziness or fainting
Bluish discoloration of the fingers
Hair that thins, breaks or falls out
Soft, downy hair covering the body
Absence of menstruation
Constipation and abdominal pain
Dry or yellowish skin
Intolerance of cold
Irregular heart rhythms
Low blood pressure
Dehydration
Swelling of arms or legs
Eroded teeth
Causes/risk factors:
As with many diseases, anorexia is a combination of biological, psychological and environmental factors. Western cultures emphasise thinness. This may be reinforced through peer pressure.
Treatment:
Treatment usually requires a team approach, which includes doctors, mental health professionals and dietitians, all with experience in eating disorders.
Ongoing therapy and nutrition education are highly important to continued recovery.
Anorexia can last for years or be lifelong. Dieting can lead to anorexia.
Recovery is possible!
Reach out – the sooner you get treatment, the better.
Name: BULIMIA NERVOSA
A serious, potentially life-threatening eating disorder marked by excessive overeating, followed by methods to avoid weight gain which include vomiting, excessive exercise, chewing and spitting food, or fasting.
Treatments include counselling, medication and nutrition education.

Physical signs/ symptoms of bulimia may include:
Preoccupation with body shape and weight
Repeated episodes of eating huge amounts of food in one sitting

Loss of control overeating
Forced vomiting or exercising after bingeing

Use of laxatives, diuretics or enemas
Fasting, restricting calories or avoiding certain foods between binges
Using products excessively for weight loss

Causes/risk factors:
The exact cause is unknown. Many factors could play a role in the development of eating disorders, including genetics, biology, emotional health, societal expectations and other issues.
Treatment:
Combining psychotherapy with antidepressants may be the most effective for overcoming the disorder.
Treatment generally involves a team approach that includes family, the primary care provider, a mental health professional and a dietitian.
Here's a look at bulimia treatment options and considerations:
Different types of psychotherapy include:
- Cognitive behavioural therapy: Helps normalise eating patterns and identify unhealthy, negative beliefs and behaviours and replace them with healthy, positive ones.
- Family-based treatment helps parents intervene to stop their teenager's unhealthy eating behaviours.
- Interpersonal psychotherapy, addresses difficulties in close relationships, helping to improve communication and problem-solving skills.
Effective treatment can help you feel better about yourself, adopt healthier eating patterns and reverse serious complications.
This is a mental health condition where a young person believes that their body is flawed or that there is something wrong with their body.

Name: BODY DISMORPHIC DISORDER
Intense focus on appearance and body image.
Repeatedly checking the mirror.
Grooming or seeking reassurance, sometimes for many hours each day impacting ability to function in daily life.
Seeking out numerous cosmetic procedures to try to and fix the flaw.
Anxiety often returns and search resumes.

Obsessive and repetitive behaviours are a central part of BDD.
They are not self-obsessed even though they focus on appearance.
Suffers from a lot of shame.
Causes/risk factors:
Body dysmorphic disorder may result from a combination of issues, such as a family history of the disorder, negative evaluations or experiences about body or self-image, and abnormal brain function or abnormal levels of the brain chemical called serotonin. Societal pressure/expectations of beauty contribute greatly.
Treatment:
Treatment may include Cognitive Behavioural Therapy and medication
Identifying the disorder early and starting treatment may be of some benefit.
TOURETTE’S SYNDROME (TS) (not a mental disorder)
It’s a condition of the nervous system that causes sudden and repeated twitches, movements, or sounds and occur with:
Attention Deficit Hyperactivity Disorder (ADHD)
Obsessive Compulsive Disorder or Behaviours (OCD/OCB)
Anxiety
Learning disabilities
Behavioural or conduct issues
Name: TOURETTE’S SYNDROME (TS)
A condition of the nervous system
Possible signs:
TS causes people to have “tics” that happen when your brain makes your body move or say something that you might not want to. Tics are sudden twitches, movements or sounds that people do repeatedly. People who have tics cannot stop their body from doing these things.
Tics usually start at 5 - 10 years old. The first tics are usually motor tics, but everyone’s tics are different. They’re usually worse during times of stress or excitement. They tend to improve when a person is calm and focused on an activity. People can’t stop their tics. They can sometimes hold them in (suppression), but eventually have to release them, very much like a sneeze.
Causes/risk factors:
Risk factors for and causes of TS are unknown.
Research shows that genes play an important role where multiple genes interacting with other factors in the environment.
Common co-occurring conditions include:
Attention Deficit Hyperactivity Disorder (ADHD)
Obsessive Compulsive Disorder or Behaviours (OCD/OCB)
Anxiety
Learning disabilities
Behavioural or conduct issues
Tourette Syndrome affects more boys than girls.
Less than 10% of people swear (coprolalia).
Treatment:
Tics are often mild and don't need to be treated.
Medication is used in some cases.
Counselling, behaviour and talk therapy can also be helpful.
Most people with TS experience their worst tic symptoms in their early teens, but tics typically lessen and become controlled by the late teens to early 20s.
TS can be a chronic condition with symptoms that last into adulthood for some, and tics may worsen in adulthood.
Billie Eilish and Lewis Capaldi both have Tourette’s. “How I’m Feeling Now” is Capaldi’s documentary on Netflix and is bringing attention to the disorder.
Tips:
There are some simple things you can do that may help to improve tics:
- Try to avoid stress, anxiety and boredom – try to find a relaxing and enjoyable activity to do (such as sport or a hobby.
- Try to ignore a child's tic and not talk about it too much – drawing attention to it may make it worse.
- Do not tell a person off when their tic occurs, reassure them that everything’s okay and there's no reason to feel embarrassed.
- People you're in regular contact with should know about tics, so they're aware of them and know not to react when they occur.
If a child is finding school difficult, talk to their teacher about ways of dealing with it, like letting them leave the classroom if their tics are particularly bad.
Suicide is the act of taking one’s own life. There are many reasons why a young person might want to die, often it is because they feel overwhelmed by difficult emotions and situations and suicide seems the only way out. Many people who commit suicide have depression. They don’t recognise that it is the depression and not the situation that is driving them to end their lives.

Suicidal Gesture
A suicidal gesture is when a person does not want to die but they want to alert others to their emotional pain they are going through.
Suicidal Ideation
The term suicidal ideation is used to describe a person who has thoughts about suicide.
Name: SUICIDE
When people harm themselves with the goal of ending their life, and they die as a result.
Possible signs:
Warning signs that someone may be at immediate risk:
Talking about wanting to die or wanting to kill themselves
Talking about feeling empty or hopeless or having no reason to live
Talking about feeling trapped or feeling that there are no solutions
Feeling unbearable emotional or physical pain
Talking about being a burden to others
Withdrawing from family and friends
Giving away important possessions
Saying goodbye to friends and family
Putting affairs in order, such as making a will
Taking great risks that could lead to death, such as driving extremely fast
Talking or thinking about death often
Other serious warning signs:
Displaying extreme mood swings,
Making a plan or looking for ways to kill themselves (searching for lethal methods online,
stockpiling pills, or buying a gun)
Talking about feeling great guilt or shame
Using alcohol or drugs more often
Acting anxious or agitated
Changing eating or sleeping habits
Showing rage or talking about seeking revenge
Causes/risk factors:
A history of suicide attempts
Depression, other mental disorders, or substance use disorder
Chronic pain
Family history of a mental disorder or substance use
Family history of suicide
Exposure to family violence, including physical or sexual abuse
Presence of guns or other firearms in the home
Having recently been released from prison or jail
Exposure, either directly or indirectly, to others’ suicidal behaviour, such as that of family members, peers or celebrities
Treatment:
Effective, evidence-based interventions are available to help people who are at risk for suicide:
Cognitive Behavioural Therapy (CBT)
Dialectical Behaviour Therapy (DBT)
Brief Intervention Strategies
Collaborative Care
If you notice warning signs of suicide—especially a change in behaviour or new, concerning behaviour – get help as soon as possible.
Family and friends are often the first to recognise the warning signs of suicide, and they can take the first step toward helping a loved one find mental health treatment.
Do not leave them alone.
Do not promise that you will keep their suicidal thoughts a secret - tell a trusted friend, family member or other trusted adult.
Call 10111 if there is an immediate life-threatening situation.
SADAG: 0800 567 567
AKESO Crisis Helpline: 0861 435 787
Love Life: 0800 121 900
Childline: 116
Deliberately harming your own body by cutting, burning or hitting yourself is known as self-injury. Self-injury is not usually meant as a suicide attempt. Rather it is a way to try and cope with, and (temporarily) release emotional pain, sadness, or anger.

Name: SELF-HARM/ SELF-INJURY/ CUTTING
Examples of self-harm include:
- Cutting, scratching or stabbing with a sharp object
- Burning with lit matches, cigarettes or heated, sharp objects such as knives
- Carving words or symbols on the skin
- Self-hitting, punching, biting or head banging
- Piercing the skin with sharp objects
- Inserting objects under the skin

Possible signs:
Symptoms of self-injury may include:
- Scars, often in patterns.
- Fresh cuts, scratches, bruises, bite marks or other wounds.
- Excessive rubbing of an area to create a burn.
- Keeping sharp objects or other items used for self-injury on hand.
- Wearing long sleeves or long pants to hide self-injury, even in hot weather.
- Frequent reports of accidental injury.
- Difficulties in relationships with others.
- Behaviours and emotions that change quickly and are impulsive, intense and unexpected.
- Talk of helplessness, hopelessness or worthlessness.
The arms, legs, chest and belly are mostly the targets of self-injury. But any area of the body may be a target, sometimes using more than one method.
Causes/risk factors:
There's no one single or simple cause. In general, self-injury may result from:
- Poor coping skills - non-suicidal self-injury is usually the result of an inability to cope in healthy ways with stress and emotional pain.
- Difficulty managing emotions - having a hard time controlling, expressing or understanding emotions may lead to self-injury.
Risk factors include:
- Having friends who self-injure
- Life issues (neglect, sexual, physical or emotional abuse, or other traumatic events, growing up and remaining in an unstable family environment, questioning personal or sexual identity and social isolation)
- Mental health issues - borderline personality disorder, depression, anxiety disorders, post-traumatic stress disorder and eating disorders.
- Alcohol or drug use.
Treatment:
Psychotherapy, Talk therapy or psychological counselling
Cognitive behavioural therapy (CBT)
Dialectical behaviour therapy (DBT)
Mindfulness-based therapies
Medicines to treat the underlying condition that's linked with self-injury to self
Inpatient care
If there's a focus on thoughts of suicide, do something to get help right away.
The release that you can feel is temporary, those feelings come back. The only way to feel better is by dealing with the cause of those feelings, using different treatments.
People who experience BPD feel emotions intensely and for extended periods of time. It is difficult for them to return to a ‘stable baseline’ after an emotionally triggering event. This can lead to impulsivity, poor self-image, turbulent relationships and powerful emotional responses to stressors. BPD can result in dangerous and impulsive behaviors.

Possible signs:
Uncertainty about identity (interests and values can change quickly)
View things in extremes (eg: either all good or all bad).
Intense and unstable relationships (often from their changing views of the person)
Impulsive and risky behaviour (misuse of alcohol/drugs, binge eating or sexual relationships)
Distorted sense of self
Intense fear of being abandoned or not wanting to be alone
Feelings of emptiness
Frequently and inappropriately angry
Acts of self-harm
Moves from crisis-to-crisis

What appear to be signs and symptoms of borderline personality disorder may go away as children get older and become more mature (their personalities are not developed until later).
Diagnosis of borderline personality disorder is not usually made in children or teenagers.
BPD has been known to lead to:
- Depression
- Substance use
- Problems with relationships at school and home
- Self-harm
- Suicide attempts
Causes:
The causes are unknown but genetic, family and social factors are thought to play roles.
Risk factors for BPD include:
Abandonment in childhood or adolescence
Disrupted family life
Poor communication in the family
Sexual, physical or emotional abuse
BPD affects females more and among hospitalised psychiatric patients.
Treatment:
There is no medication to treat BPD but medication for other symptoms like anxiety or depression.
DBT and MBT therapy can help.
Art and other creative therapies
Over time and with treatment many people with BPD overcome their symptoms and recover. Recovery means different things to different people.
If you’re thinking about suicide or acting on suicidal thoughts, wanting to self-harm, or doing something that could put yourself or other people at risk, PLEASE GET HELP IMMEDIATELY!
SADAG Mental Health Helpline
0800 456 789
SMS 31393
A mental illness that affects about 1% of the population. It interferes with mental functioning and behaviour.

It can present in adolescence or early adulthood as psychosis* with:
- Delusions (thinking things that are not true)
- Hallucinations (seeing or hearing things that aren’t there)
Psychosis may or may not develop into schizophrenia.
Name: SCHIZOPHERENIA
Schizophrenia is a serious mental disorder in which people interpret reality abnormally.
Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behaviour that impairs daily functioning. It can be disabling.

Possible signs:
- Delusions - These are false beliefs that are not based in reality. Delusions occur in most people with schizophrenia.
- Hallucinations - These usually involve seeing or hearing things that don't exist. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganised thinking (speech) - Disorganised thinking is inferred from disorganised speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated.
- Extremely disorganised or abnormal motor behaviour - Childlike silliness to unpredictable agitation.
- Negative symptoms - Inability to function normally, neglecting personal hygiene or appear to lack emotion, may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Causes/risk factors:
Causes of schizophrenia are unknown but researchers believe that a combination of genetics, brain chemistry and environment contribute to development of the disorder.
Treatment:
The treatment team may include a psychiatrist, a psychologist, social worker, psychiatric nurse.
Treatment with medications and psychosocial therapy can help manage the condition.
In some cases, hospitalisation may be needed.
Schizophrenia requires lifelong treatment, even when symptoms have subsided.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Suicidal thoughts and behaviour are common among people with schizophrenia. If your child is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person. Call your local emergency number immediately. Or take the person to the closest emergency room if you think it is safe to do so.
SADAG Mental Health Helpline
0800 456 789
SMS 31393
This is when a person struggles to know what is real and what is not.
They might:
- see or hear things that others do not (hallucinations)
- believe things that are not true (delusions)

This can be very frightening and may cause a person experiencing a psychotic episode to hurt themselves or others.

The causes of psychosis are not always obvious but, in some cases, may be linked to drug and alcohol abuse.
Bereavement is the word used to describe the sadness that a person feels after someone they love has died.

Bereavement is the word used to describe the sadness that a person feels after someone they love has died. Grief is about how a person reacts to their loss.
It can be very painful and may take a long time before they adjust to the emotional and life changes that happen when someone dies.
>br>
However, Complicated Grief is a chronic form of grief that can impair someone’s life.
Don’t forget that Mental Distress happens when the level of stress is higher, and reactions are stronger and more intense. Grief and bereavement are massive stressors for our mental health. Remember that there are ways to get help before your grief becomes debilitating:
- Support groups
- Counselling

- Group counselling
- CBT
- DBT
- Friendship bench

Grief can make you feel many different emotions, and it’s normal to feel anger, deep sadness, despair, afraid, scared and anxious after someone you love passes away. It may take a long time for you to feel consistently a bit better. This does not mean you have a mental illness.
Grieving for a loved one is important, but by seeking help when you’re in Mental Distress and getting the right support, you’ll start to have more days that are a little brighter and sunnier.
Name: COMPLICATED GRIEF
Possible signs:
Complicated grief often dominates a person’s life, interfering with their daily functioning.
Prolonged symptoms may include:
- Intense sadness and emotional pain
- Feelings of emptiness and hopelessness
- Yearning to be reunited with the deceased
- Preoccupation with the deceased or with the circumstances of the death
- Difficulty engaging in happy memories of the lost person
- Avoidance of reminders of the deceased
- A reduced sense of identity
- Detachment and isolation from surviving friends and family
- Lack of desire to pursue personal interests or plans
Causes/risk factors:
The exact causes are unknown, but it is thought to be a combination of genetic, environmental and psychological factors.
Risk factors:
Losing a loved one suddenly or tragically
A history of anxiety or depression
Having a close relationship with the deceased
A lack of social support or community
A history of trauma or abuse
Treatment
Treatment usually involves therapy, medication, or a combination of both.
The experience of grief is something that a person comes to terms with gradually. It’s a slow process out of grief and it’s important to be patient and kind to yourself.
Mental illness comes from a MIXTURE of many things.
For example, if a family member suffered from depression, you might have a greater chance of experiencing depression.
(That is what inherited means).
What kind of lives we live. For example, we may live in poverty, with no support, or we may live in comfort with loving people around us).

We each have a unique way of thinking, feeling, and behaving and that in turn influences how we react to things that happen.
Some people might shrug off a challenge and others might be weighed down by the same challenge.
Everyone has a different personality, and our personalities remain much the same throughout life.
Different personality types can have different ways of coping with stress.
Personality is one the factors that play a part in our mood and our reactions.

Mental health problems can happen at any age at any time, but adolescents are much more likely to be affected because your brains and your bodies are changing very quickly.
Let’s have a look:

Your brain is still under construction.
Right now, it is like a sponge, soaking up new experiences, new situations, and new information.
It’s amazing.
It adapts and responds easily. More easily than an adult brain.
Right now, it is changing, becoming more efficient, being shaped and re-modelled with new roads (neural pathways) every minute of the day.
Your brain cells (neurons) are making connections that will become stronger or weaker, last a lifetime or get pruned away if they are not used.
But you must use it if you don’t want to lose it.
The more you do things, like listening to music, studying, playing sport, or taking on a new hobby, the stronger the connections become and the longer they last.
You might feel more than you think.
So, it’s not so easy to put the brakes on risky behaviour either.
It may seem like a good idea to just do it but the message that it might be risky and dangerous doesn’t get much attention.

One of the ‘happiness’ hormones the brain releases (dopamine) reaches especially high levels in adolescence, encouraging you to do it, even though it’s not a good idea.
That can make it harder to say NO.
The early-adolescent brain is very much like being in a car with a fast accelerator and very weak brakes.

Hormones can make you super-sensitive to stress too. They can affect your mood, emotions, and impulses.

Does all this sound like your brain is in charge?
NO!
You can help your brain to become resilient…
Learning skills like coping, problem solving, and decision making can make a world of difference…

And because your brain is sensitive to repair too, getting help when it’s needed even for more serious problems like anxiety and depression is always a good idea.

DO:
- Eat healthy foods. They contain vitamins and minerals that are important for the nervous system.
- Get a lot of playtime (exercise).
- Get lots of sleep.



DO:
Wear a helmet when you ride your bike or play other sports that require head protection.

Challenge your brain by doing puzzles, reading, playing music, making art, learning dance steps, or anything else that gives your brain a workout!

DON’T drink alcohol, take drugs, or use tobacco.

During adolescence, sleep patterns change because of hormonal changes in the brain. But you still need plenty of sleep for your overall health and development, including your brain development.

Some tips to get the sleep you need:
- Try and find a comfortable, quiet sleep environment.
- Wind down before bed, away from screens including phones.
- Go to bed and wake up at regular times each day.
- Get 8-10 hours of sleep each night.
For people with mental health issues, the social stigma and discrimination they experience can make their problems worse, making it harder to recover. It may also cause the person to avoid getting the help they need because of the fear of being stigmatized.
Stigma is born out of ignorance.
It happens when people judge others who are different from them in some way.
They might have a disability, a different skin colour, a different belief or identity.
People with a mental illness are stigmatised when they are judged and treated badly because of people’s false beliefs about mental illness.

People with a mental illness are stigmatised when it is believed that:
- mental illness is a sign of weakness
- teenagers don’t have mental health problems
- mental health illness is not common
- you can’t help someone with a mental health problem
- all people with mental illnesses are violent
- that mental health problems are caused by witchcraft or evil spirits
These beliefs come from not knowing the facts and they make those with a mental illness feel ashamed.
This stops people from getting the help and support they need.
Mental illness is not something a person chooses to have. Just like any other illness, mental illness is a real health condition. It is nothing to be ashamed of.
PEOPLE WHO STIGMATISE OTHERS make people feel:
- like they can’t talk about a mental health problem
- that mental health problems are not ok
- they must be hidden from others

- Learn about mental illness
- Speak out
- Get help if you need it
- Support others to get help and support
- Stop stigma
Anyone can have a mental health problem - from a child to an adolescent, an adult to a grandparent. There are lots of treatments that work.

By talking openly about mental health
By not using stigmatising language – words have power
By knowing the facts and sharing your knowledge
By speaking out when you see people being stigmatised
By getting help and support for ourselves and those around us
If someone you know is struggling with their mental health, you can:
- encourage them to talk about their experience in a way that feels comfortable to them.
- be patient, remember that the issues are very real to them, even if they seem unrealistic, irrational or extreme to you
- don't judge even though it can be upsetting to hear about mental health challenges. If you act shocked or judge them, they will be less likely to share their thoughts and feelings with you in future.
- love and support them regardless of their
- difficulties at the time.
- find out what you can about their challenges, it will help you understand what they’re going through.
| Akeso psychiatric response unit | +27 (0) 86 143 5787 |
| Alcoholics Anonymous | +27 (0) 86 143 5722 |
| ChildLine | +27 (0) 80 005 5555 |
| Gender Based Violence command centre | +27 (0) 80 042 8428 or *120*7867# |
| Human Trafficking | +27 (0) 800 073 7283 / +27 (0) 82 455 3664 |
| Ithemba Drug Toll-Free number | +27 (0) 80 022 3217 |
| Lifeline crisis line | +27 (0 86 132 2322 / +27 (0) 11 728 1347 |
| Narcotics anonymous SA | +27 (0) 83 900 6962 |
| National Human Trafficking Helpline | +27 (0) 80 022 2777 |
| Rape Crisis Cape Town | +27 (0) 21 447 9762 |
| SA Depression and Anxiety Group suicide line | +27 (0) 80 056 7567 / +27 (0) 11 234 4837 |
| Stop gender violence centre | +27 (0) 86 132 2322 / +27 (0) 80 015 0150 |
| Substance abuse helpline | +27 (0) 80 012 1314 |