STIS
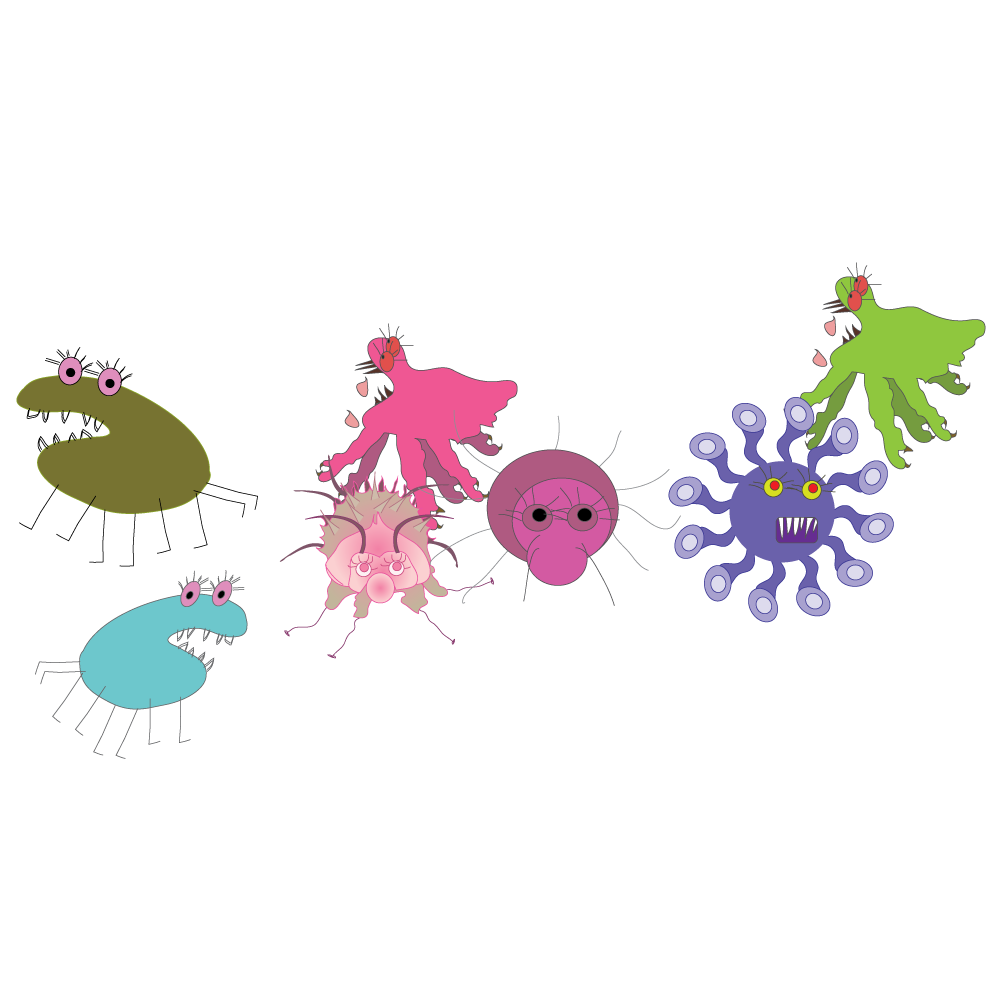
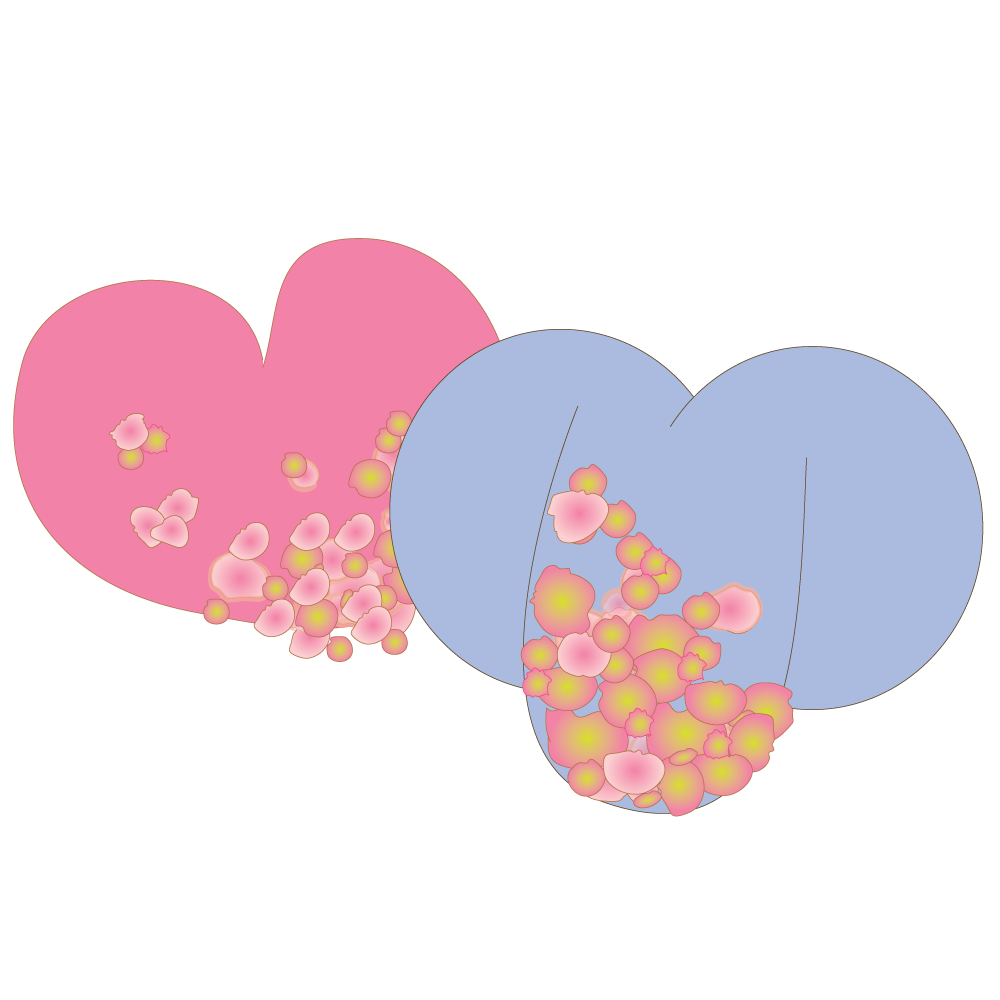
STIs are infections (diseases) that are spread through sexual contact. Most are spread through unprotected penetrative sex, but some can be spread through oral sex and mutual masturbation.

They used to be called venereal diseases or sexually transmitted diseases.
Some STIs like herpes, thrush, lice and chlamydia can be spread through oral sex and mutual masturbation.

Most STI’s can be cured if you get treatment in time.

Sexual partners (both/all) need to be treated or reinfection will take place during unprotected sex (the STI will come back).
Make sure your partner gets treatment too.

Sexually transmitted infections (diseases) spread from person-to-person by various types of sexual behaviour.

Many STIs are spread by secretions (saliva, urine, sexual fluids) and/or blood contact.
Some STIs like herpes, lice, thrush and chlamydia are spread by close physical contact.
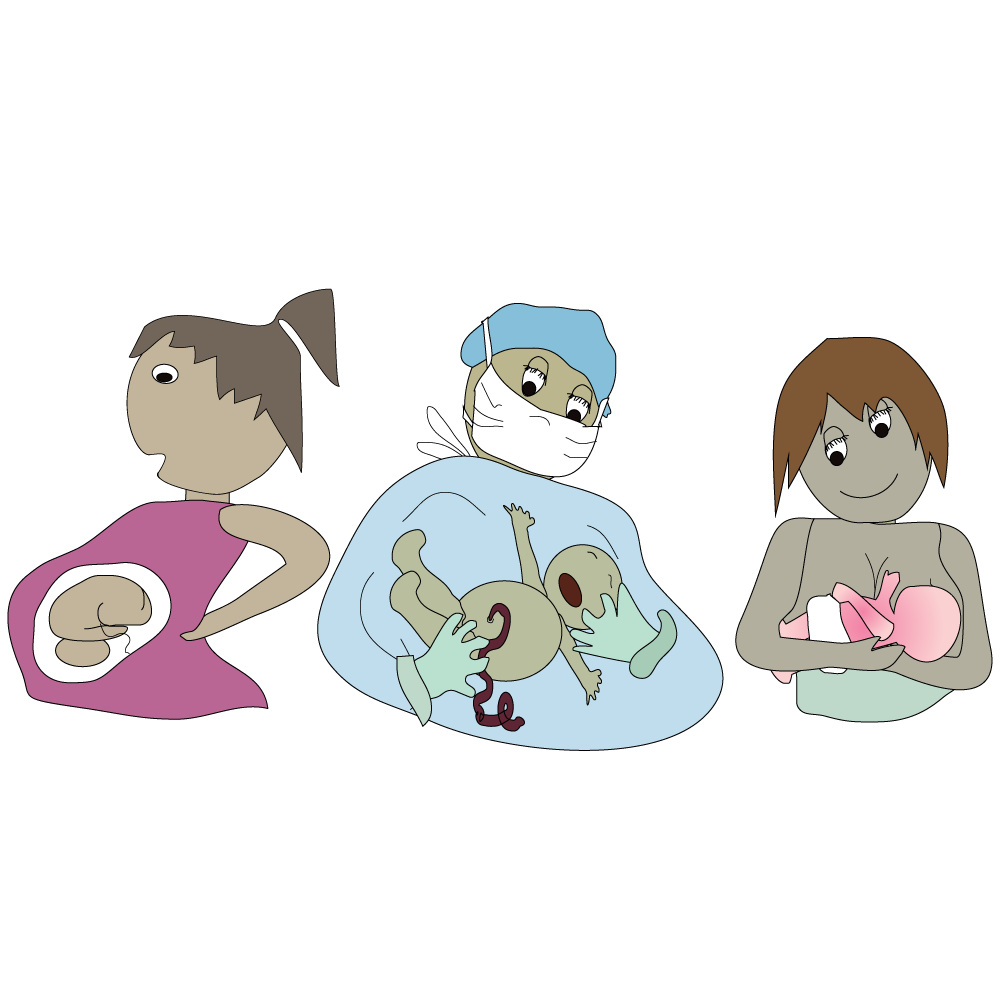
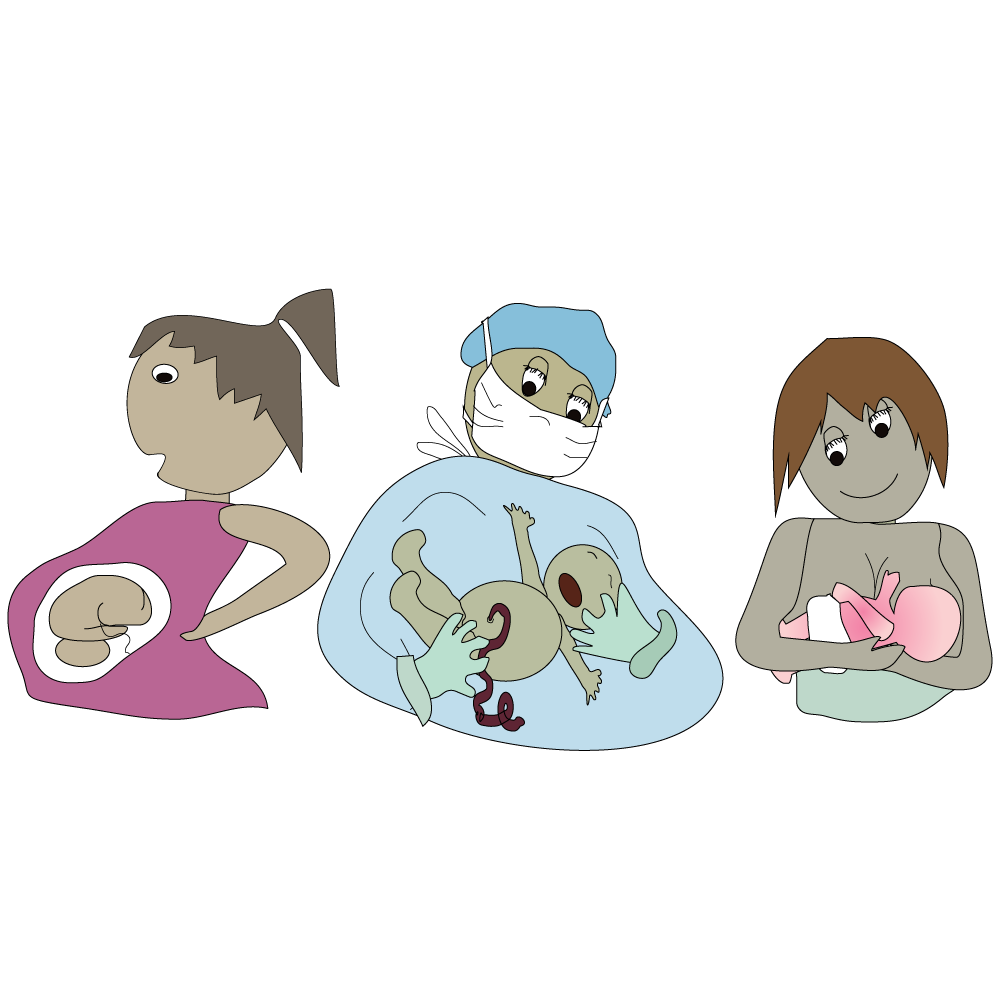
Some STIs can be spread from mother to baby during pregnancy, breastfeeding or birth.

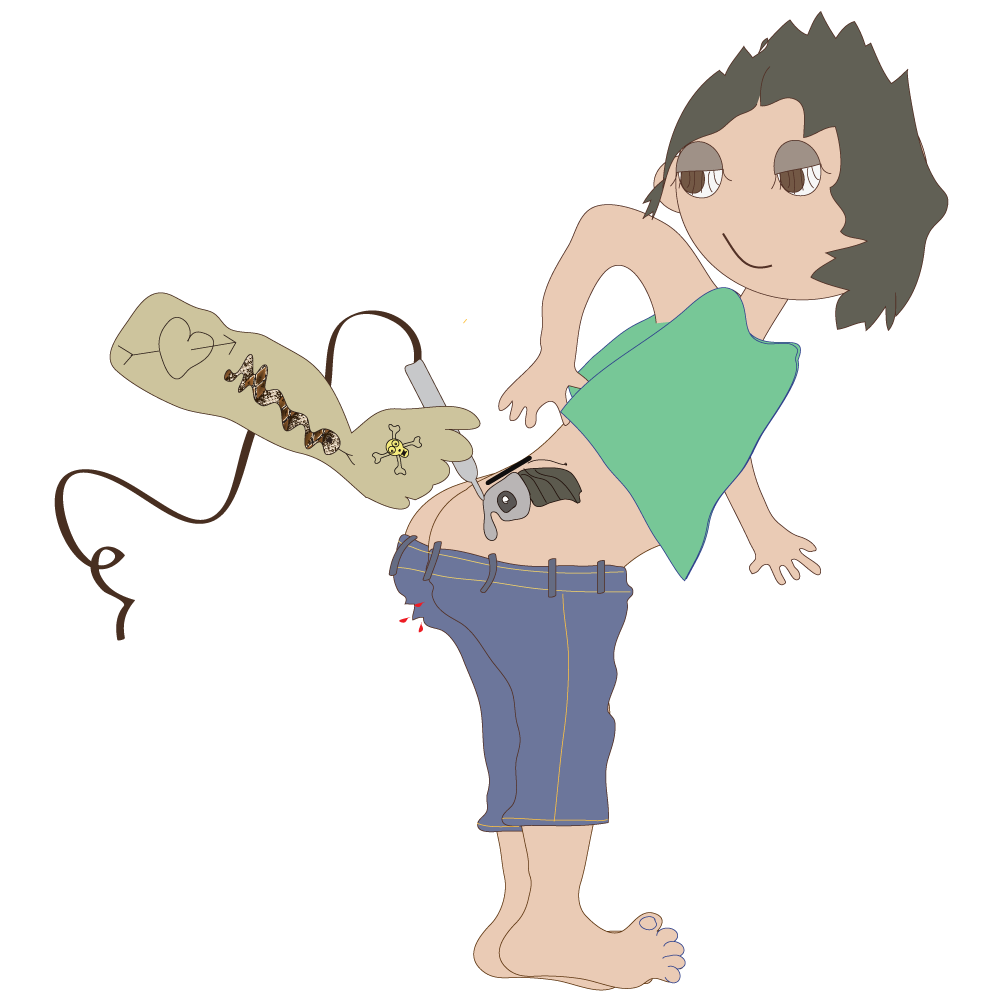
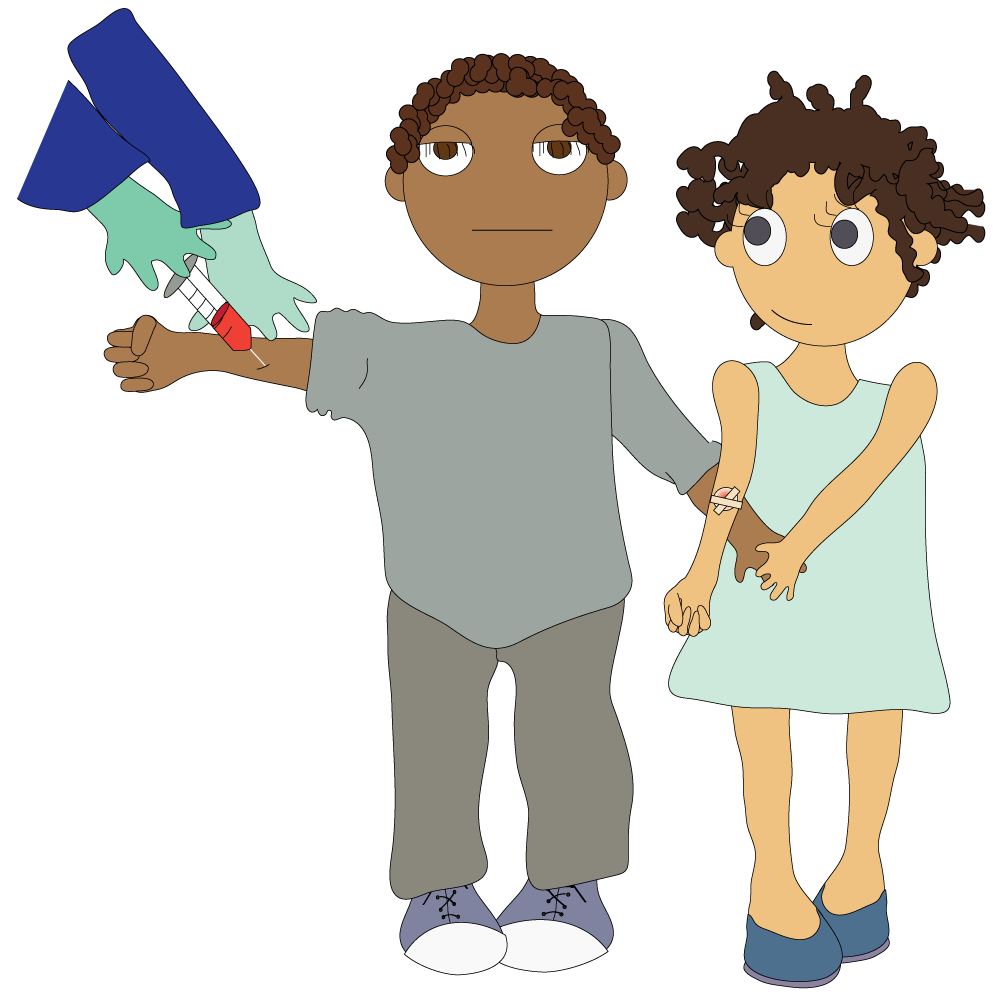
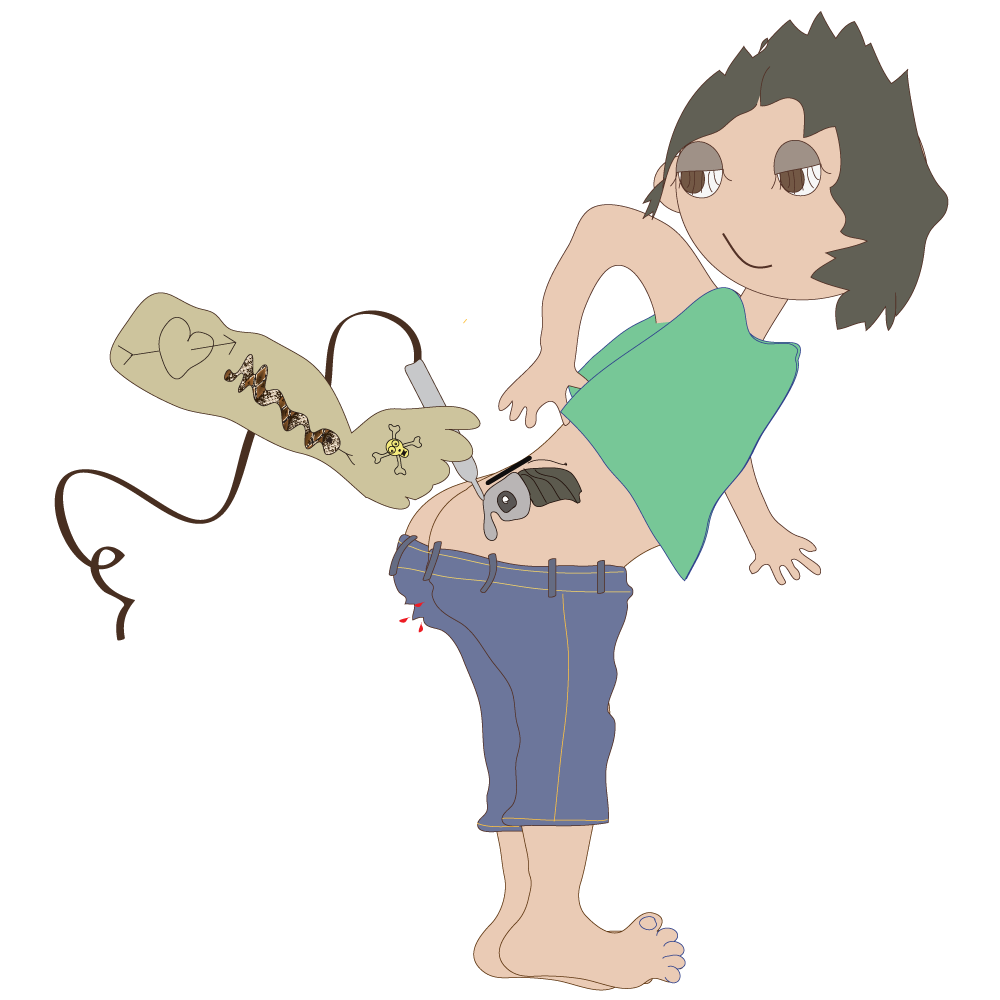
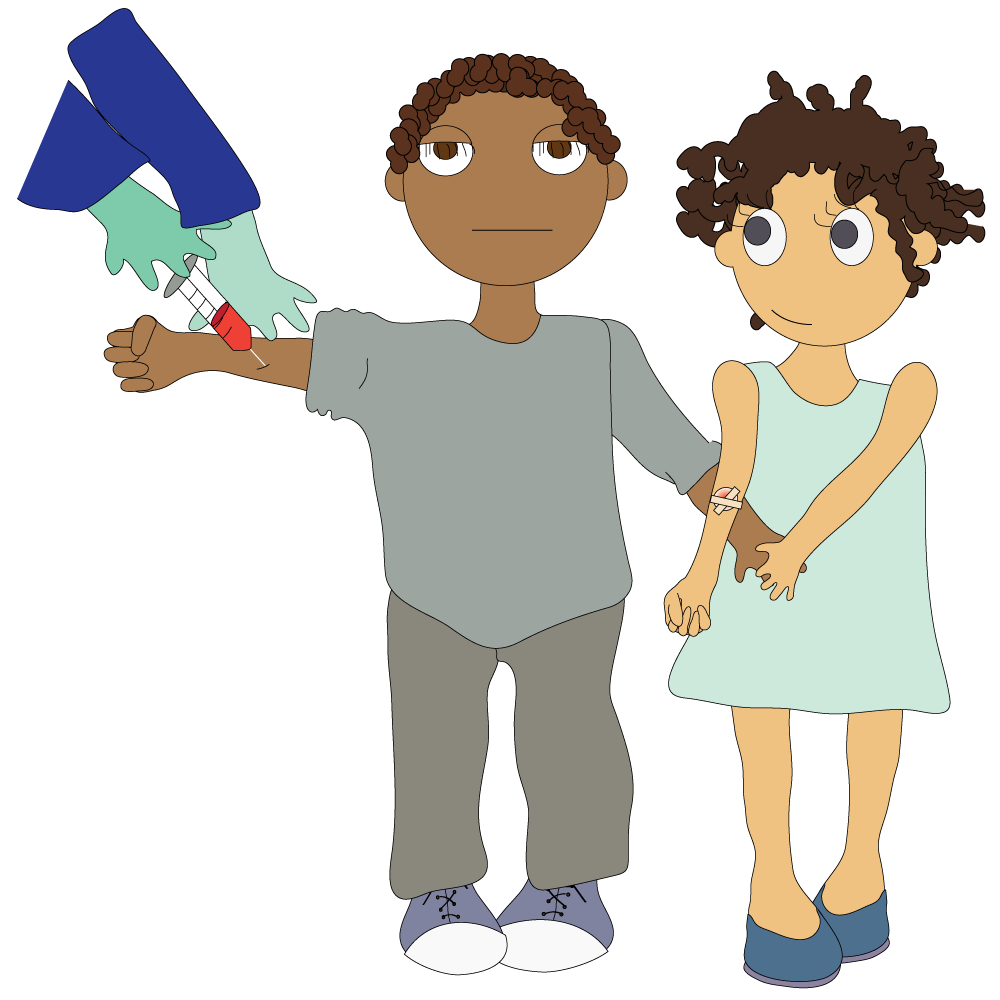
STIs can also be transmitted through unsafe blood practices like sharing needles, during intravenous drug use, scarification rituals or tattooing.


Needlestick injury can also result in transmission of STIs.
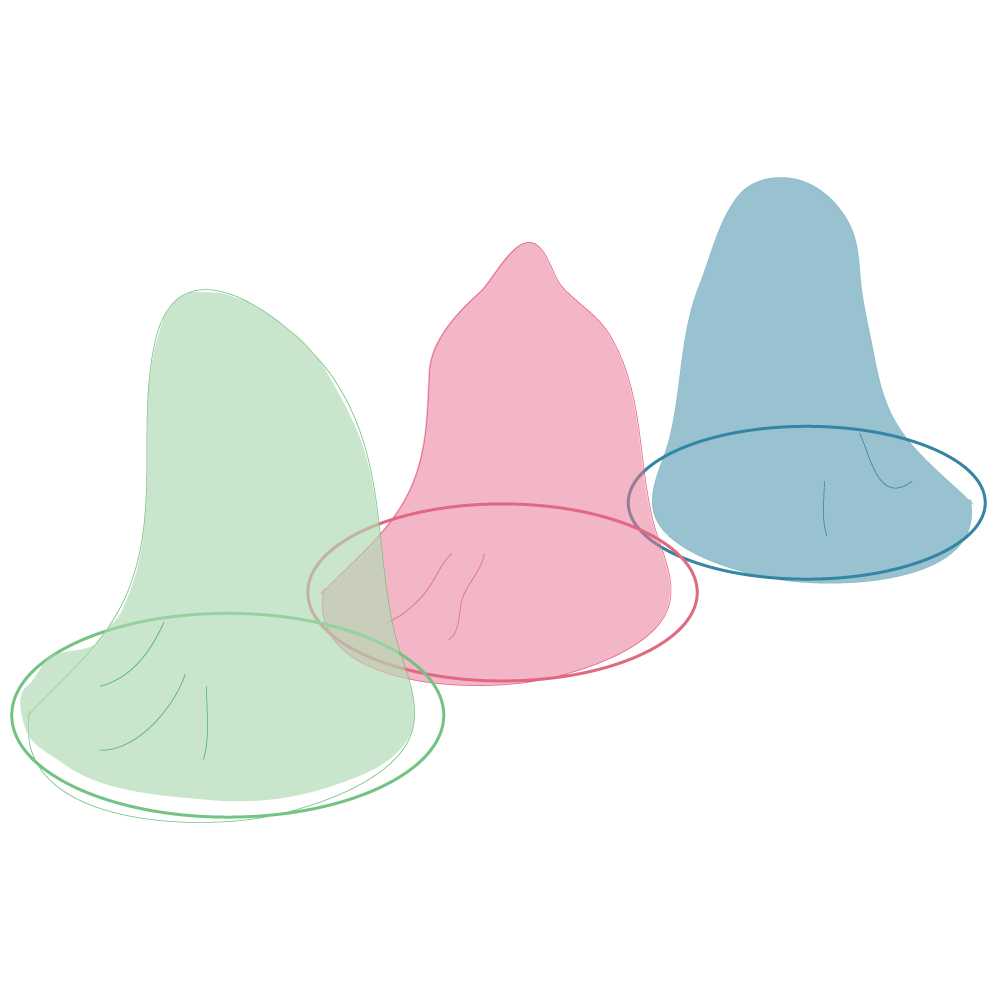
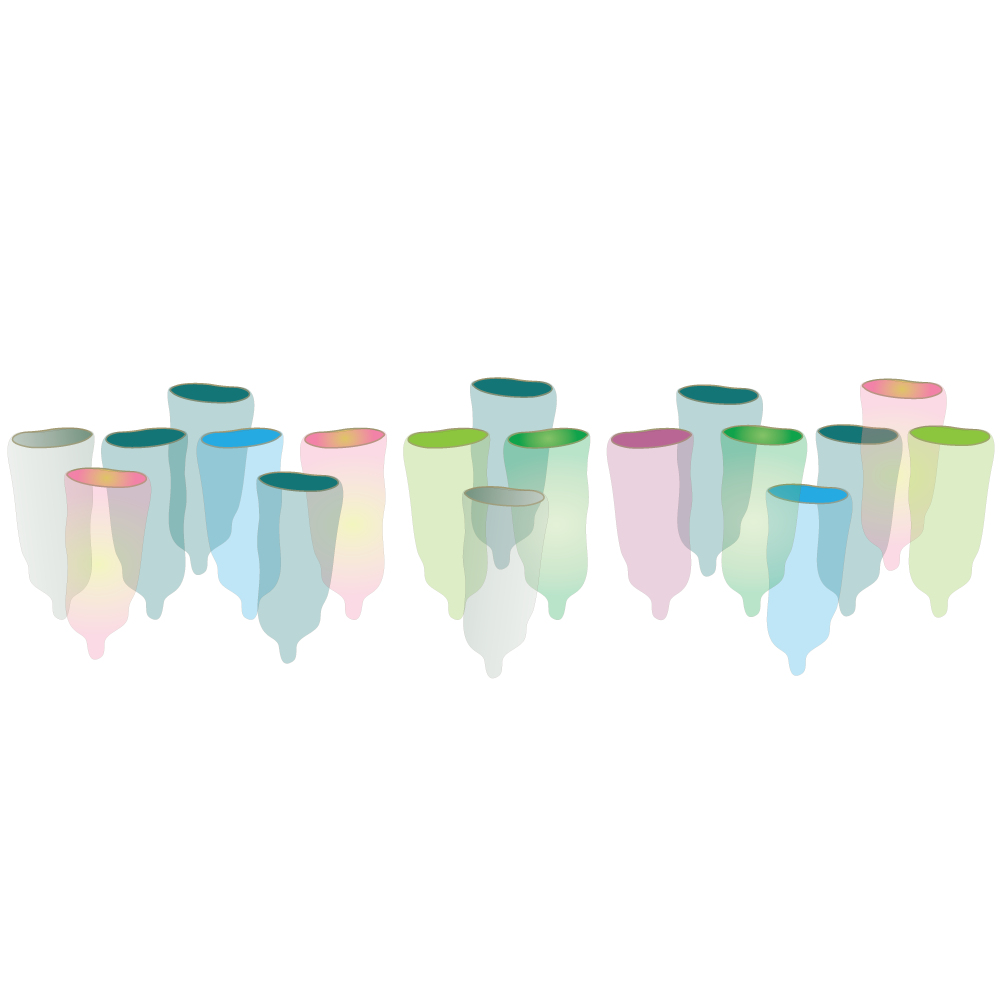
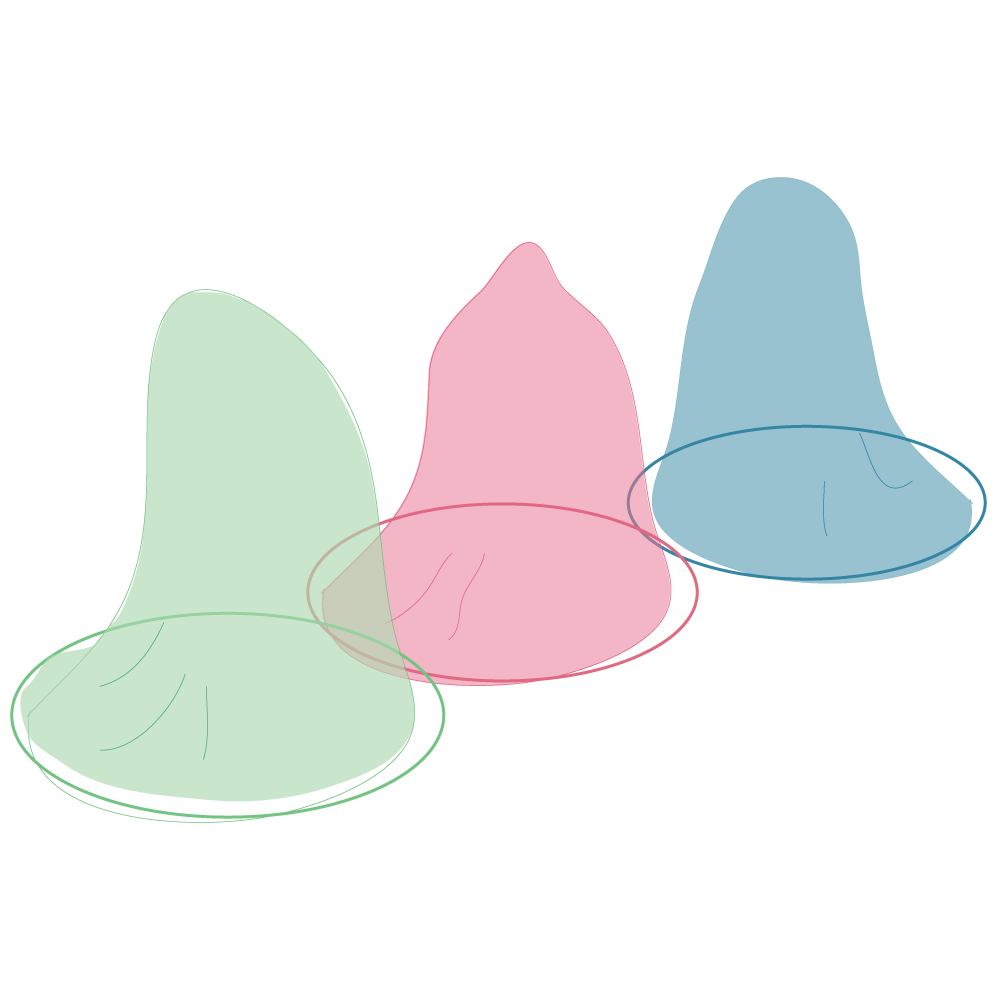
Unprotected sex (anal, vaginal and oral). Not using condoms consistently and correctly.
Lots of sexual partners.

Sharing underwear/sex toys.

Mother-to-child transmission.

Unclean needles /needlestick injury.
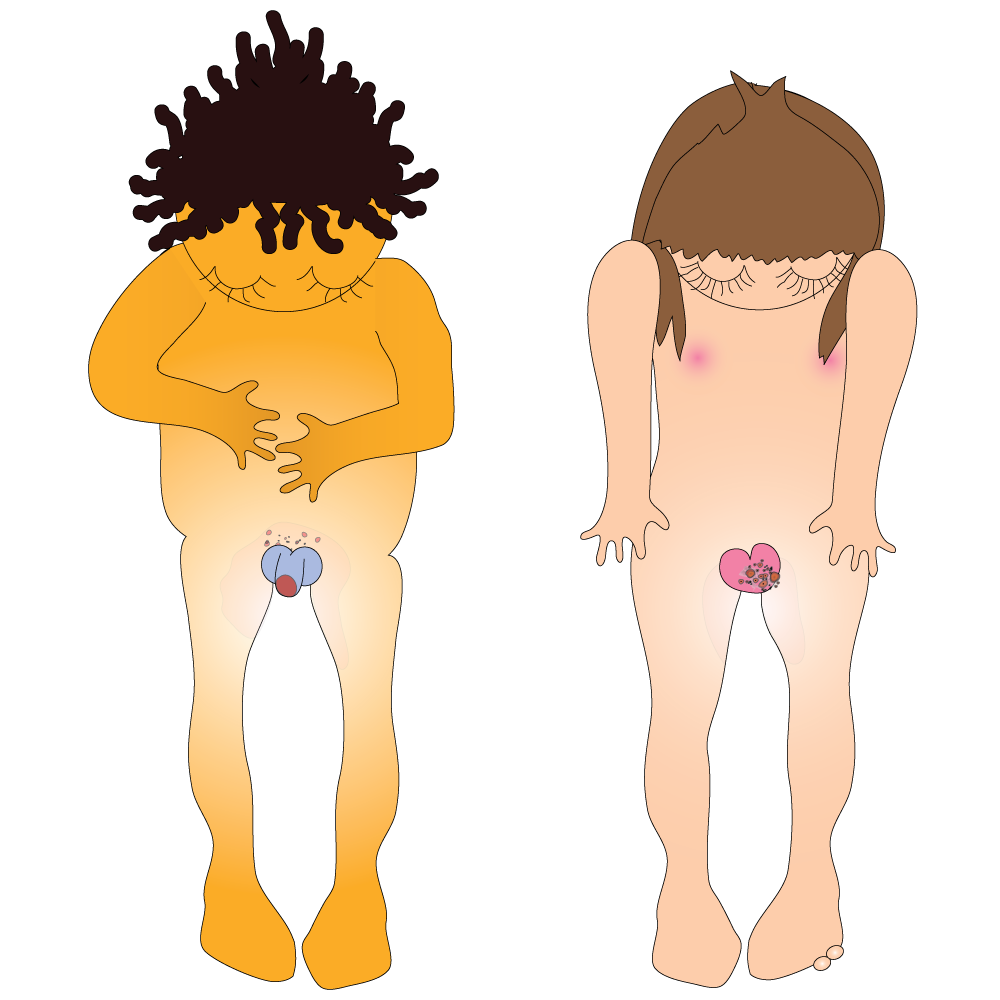
STIs are often silent (asymptomatic). They can’t be seen.

That is why it is important to get screened.
If you don’t, you won’t know you’re infected, so you won’t get treatment and you will pass your STI on to your sexual partner/s.
* Symptom means a sign or indication of the existence of something else, a sign or indication of a disorder /disease, especially when it’s a change from normal function, sensation or appearance.
Sometimes there are no symptoms or symptoms take a while to appear.

Some STIs (Chlamydia and Gonorrhoea) have no symptoms, or no early symptoms (Silent STIs).
Having unprotected sex with a person who has an STI in its silent phase means that you can become infected without seeing any signs on the person.
This means you can pass on your STI without even knowing you have an STI yourself. So STIs can spread further and result in complications such as PID (Pelvic inflammatory diseases) and infertility.
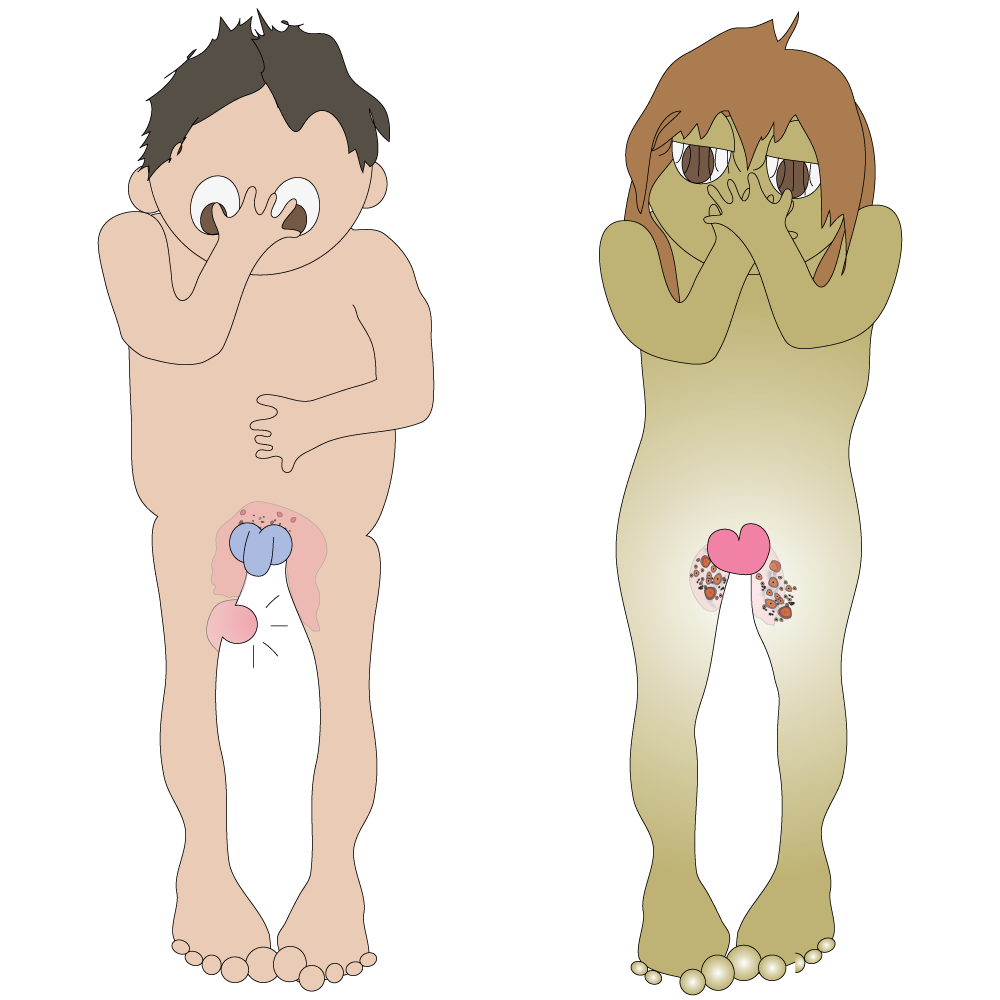
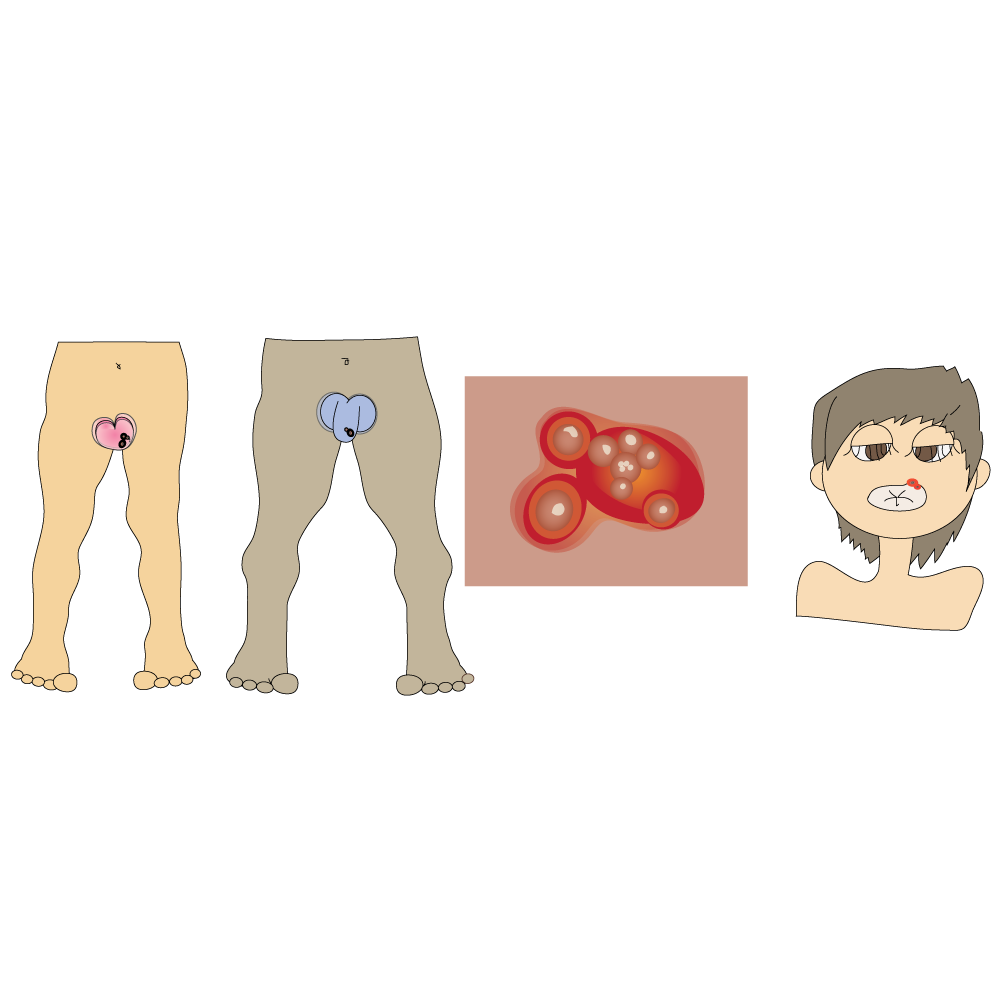
Sores /ulcers on the genitals.
Rashes /swelling /lumps in the groin.
Discharge from penis/ vagina.
Warts on, in and around penis /vagina /anus.

Burning when passing urine.

Pain in testicles (boys).
Pain in the lower belly (girls).
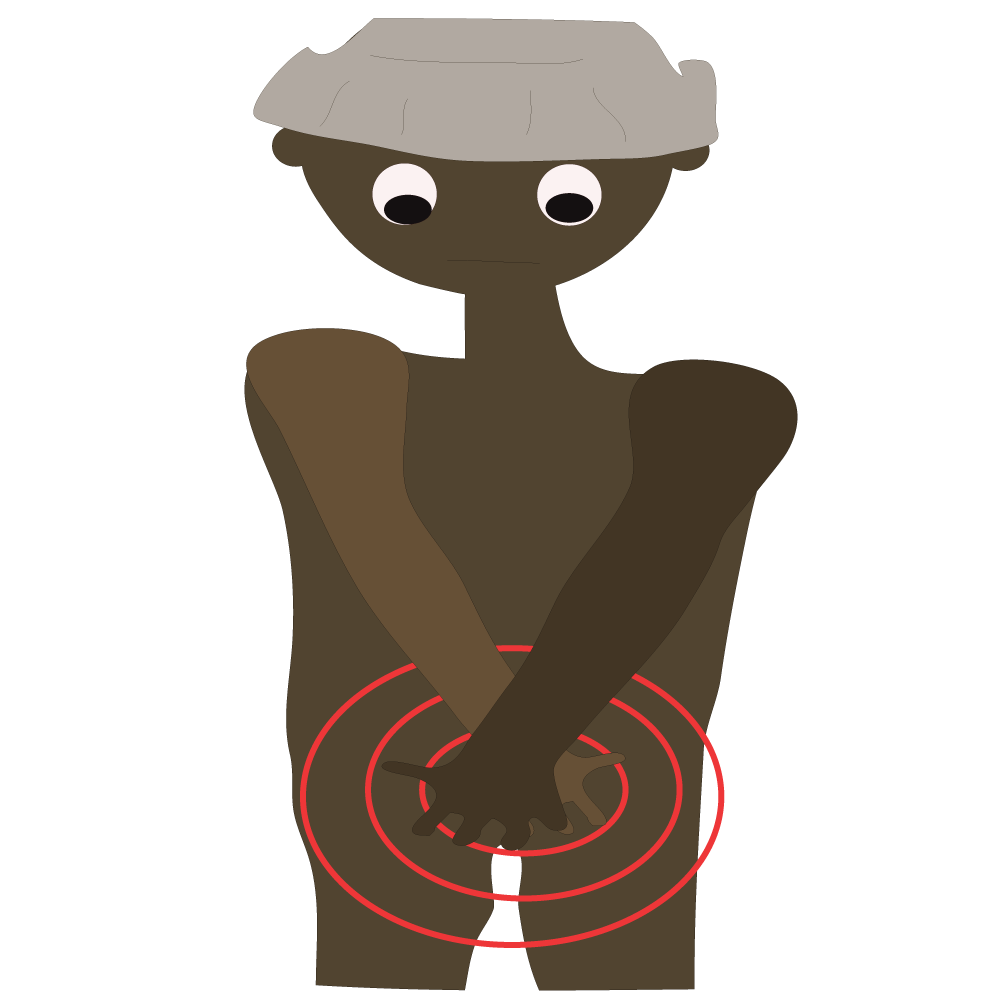
Itching pubic area (mainly at night).

Rashes /lesions /lumps /sores, aches and pains on the body, swollen glands, and a high temperature, plus other assorted symptoms.

You can have more than one STI at a time.
If you think you might have an STI, get treatment as soon as possible. Most, but not all STIs are easily treated.
You should have an STI screening if:
- you are sexually active and have not had a check-up before
- you have had unprotected oral, vaginal or anal sex with one or more partners
- your sex partner has had unprotected sex with someone other than you
You have any unusual symptoms including:
- unusual discharge from your penis or vagina
- pain when passing urine
- unusual sores or blisters in the genital or rectal (anus) area
- itching or irritation in the genital area
- pain during sex
If you are sexually active and you or your partner might be having sex with someone else, you should plan to have a check-up every 6 -12 months.
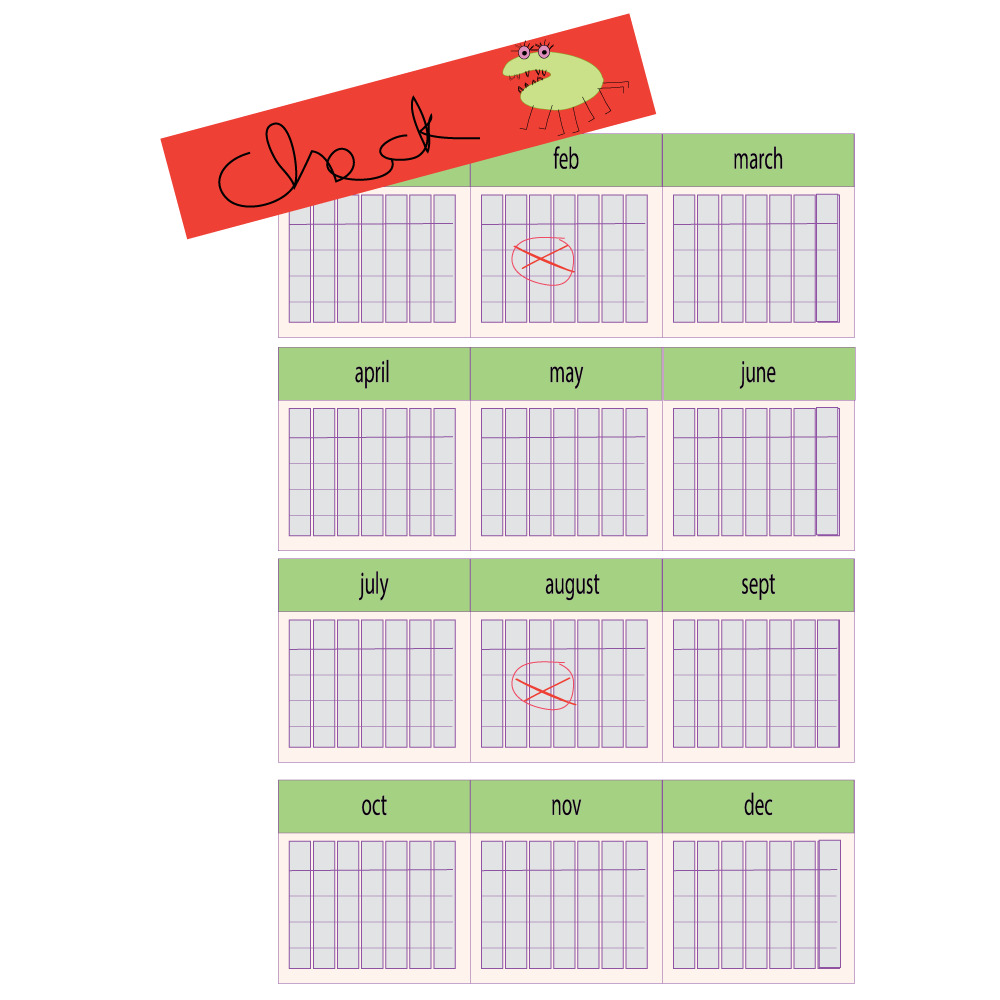
STI screening means you are being tested for all the sexually transmitted infections at the same time.
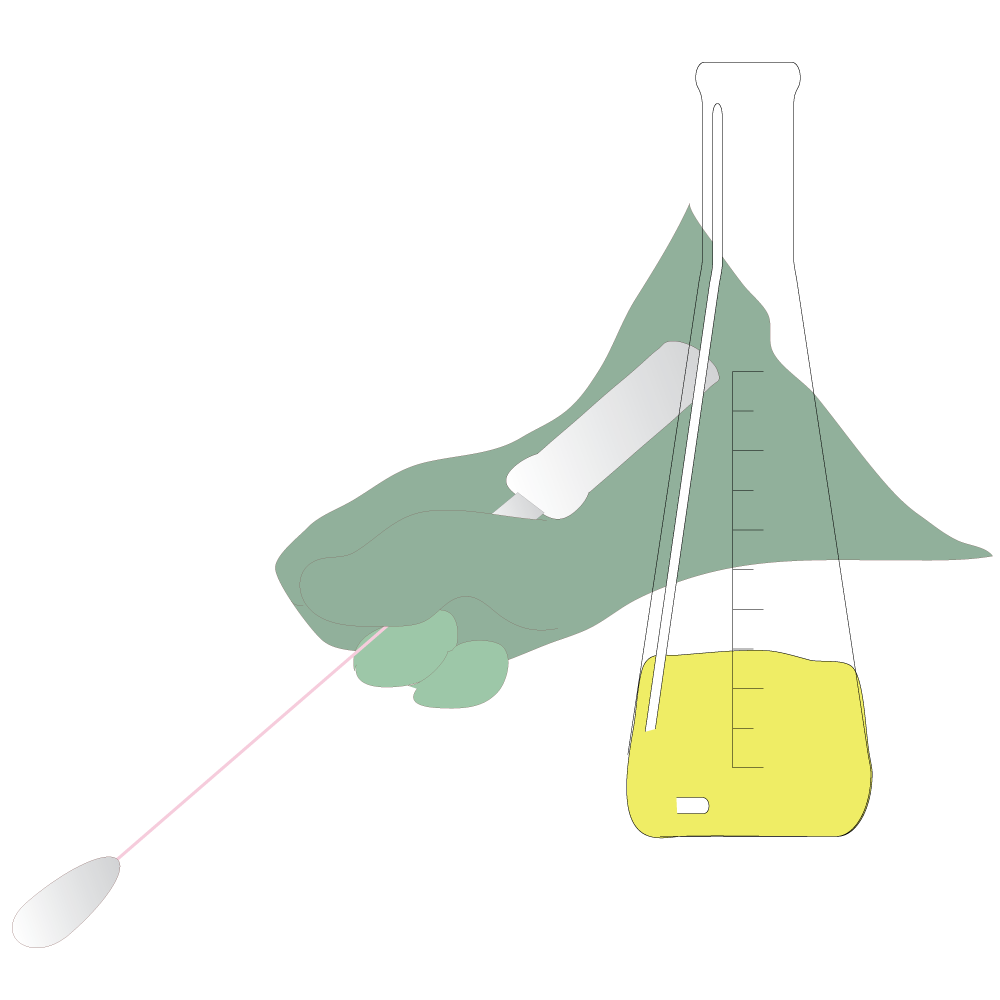
A screening usually includes:
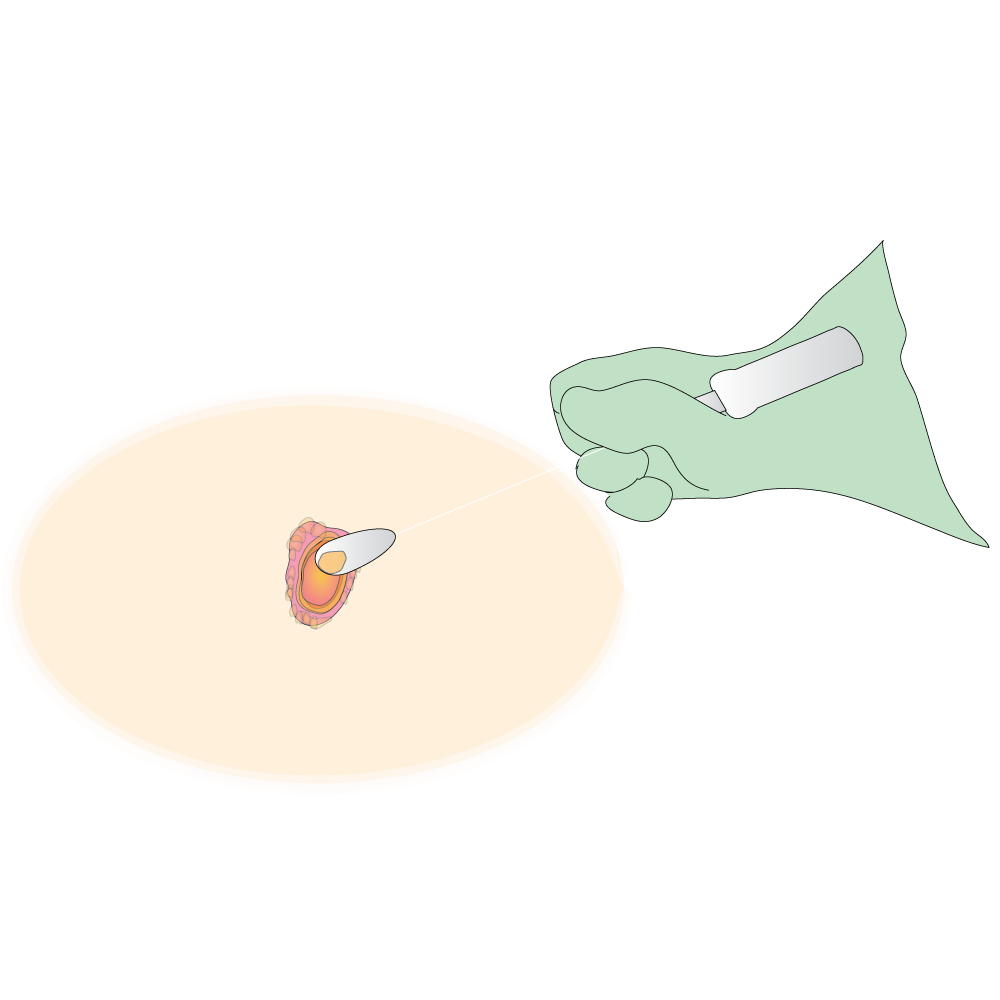
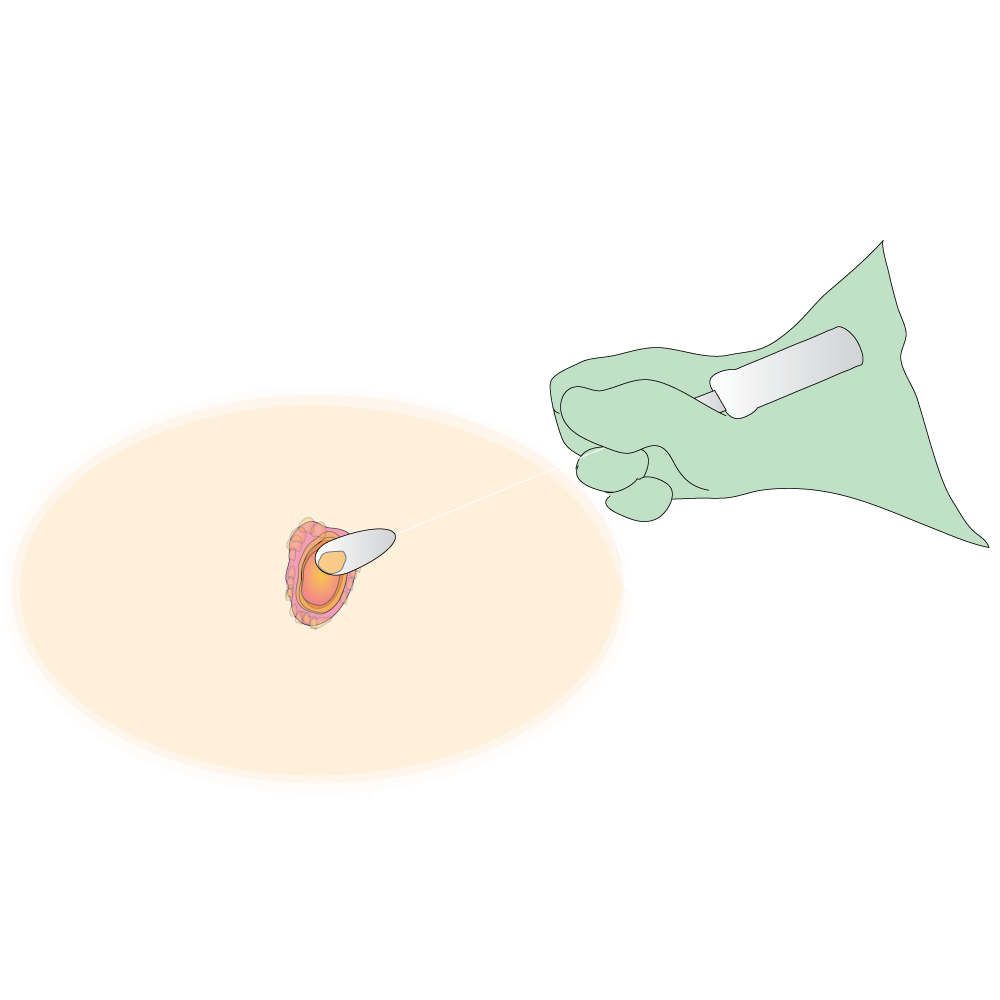
- Swabs (sample of mucous /tissue /blood scooped onto a small piece of absorbent material attached to a soft stick and sent to laboratory for analysis)
- Blood tests
STI screening is free at state clinics. You will need to make an appointment for most clinics, unless they provide a drop-in service.
When you get STI treatment make sure all your sexual partners get treated. If not, you can get the STI again when next you have sex with the untreated person.


Understand the following points before you start treatment:
- Why you need the drug
- How and when to take the drug and/or where and how to apply the cream or lotion
- How to store the drug
- What might happen if you don't take the drug as prescribed
- How long to take the drug for
Ask your health care worker to explain everything carefully and to write down the medication instructions

It is very important to follow your health care worker’s instructions.
- Never use your medication for any symptom of illness other than the one for which it was prescribed.
- Never take someone else's medication or give your medication to someone else.
- Never take more or less of a medication, unless directed by your health care professional.
How well will my medication work?
Read the following statements. Tick the block if any apply to you.
- I sometimes forget /put off having my medication refilled.
- I sometimes forget to take my medication.
- I sometimes take my medication at the wrong times.
- I take many different medications and sometimes it's hard to know one from the other.
- I sometimes stop taking medication once I feel better
- I sometimes take more or less of my medication than my doctor prescribed.
- I sometimes stop taking my medication because I think it is not working.
- I don't understand when I am supposed to take my medication.
- I don't ask my health care worker questions about my medication because I am shy or embarrassed.
If you have ticked any one of the blocks, you may not be getting the full benefit of your medications.
Talk to your health care worker about taking your medications correctly - it will really help with your treatment outcomes.

Condoms protect against most but not all STIs. The only way to stay 100% protected from STIs is to abstain from sex altogether. Some STIs show no visible symptoms, so you won’t always know if you need a check-up.
The only sure way to prevent sexually transmitted infections is to avoid having sex entirely, or to be in a long-term mutually monogamous (100% faithful to each other) relationship with a trusted partner who has been tested and is known to be uninfected.
Condoms do not always protect. Contact with a sore outside the condom-covered area can still cause infection.
Another approach is to talk about these kinds of infections before you have sex with a new partner, so that you can make informed choices about the level of risk you are comfortable taking with your sex life.

- Abstain from having sex if you can
- Delay having sex for as long as you can
- Always use a condom if you can’t delay
- Avoid having sex during menstruation
- Do not share needles/blades etc
- Do not share sex toys or underwear
- Get screened even if you have no symptoms
- Get early treatment of any STI
- Make sure your partner/s get treatment as well
- Finish taking your treatment
- Get regular check-ups
- Change your sexual behaviour
- Practice safer sex - use condoms every time
- Vaccinations (in some cases)
- Understand your treatment.
- How and when to take it

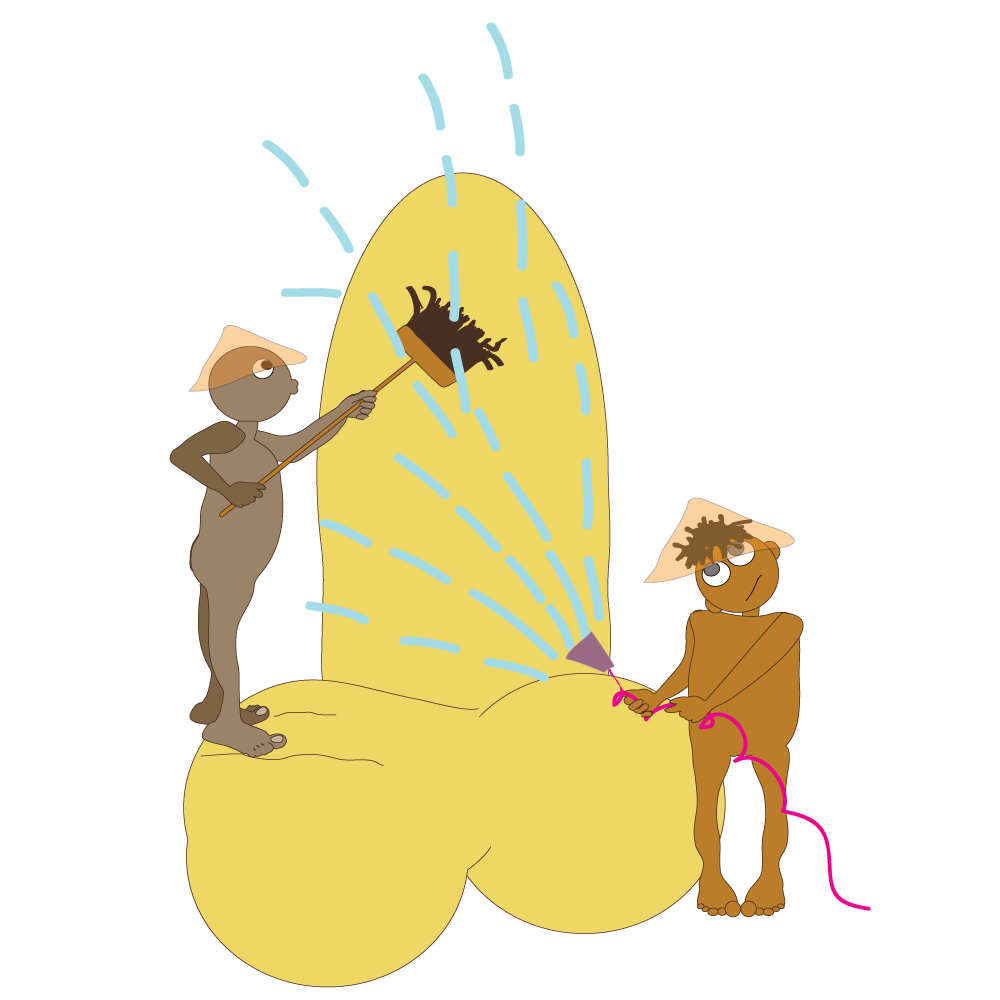
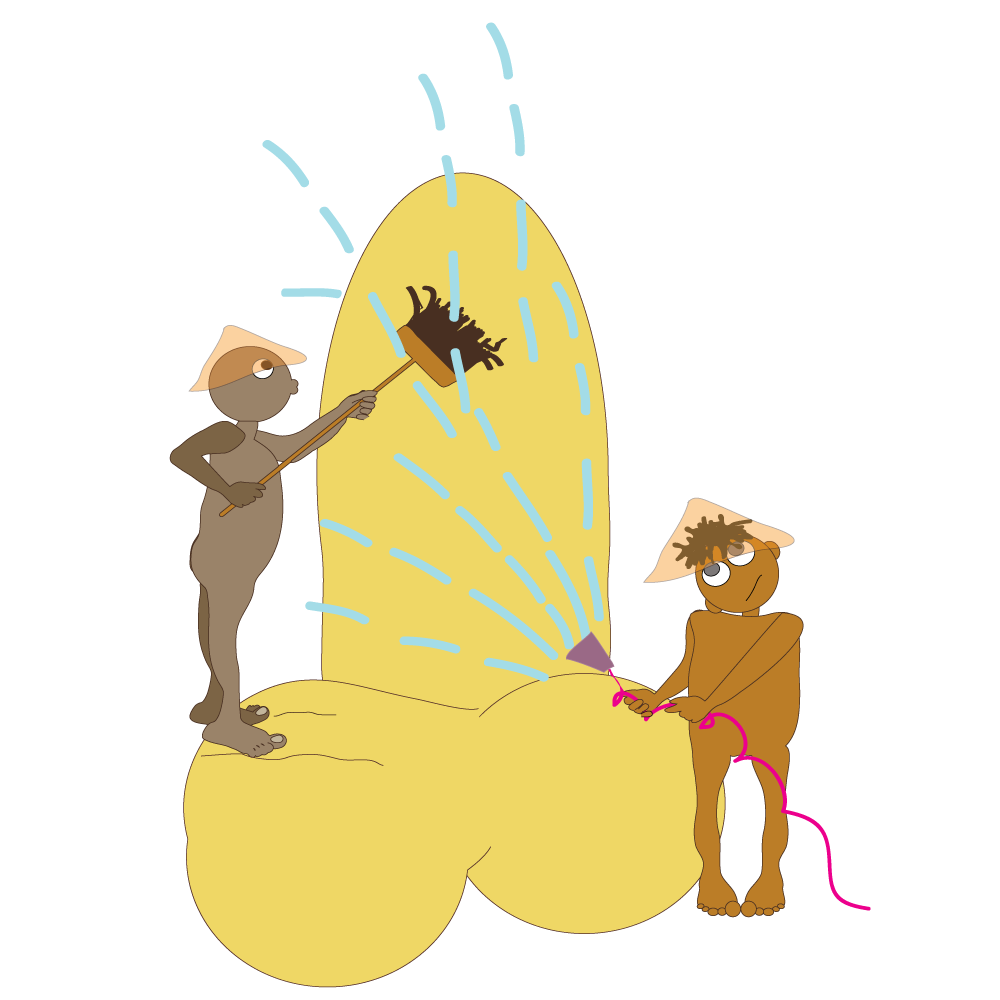
Personal hygiene - making sure your body is clean.
People have different ideas about personal hygiene. Some people wash their body at least every day and use deodorant to stop armpit smells. Bodies can smell bad if they’re not washed often.
Body smells are caused partly by:
- Chemicals that the body makes (such as the pheromones or ‘sexual’ chemicals that attract – or repel – others)
- Things the body is trying to get rid of by breathing them out (such as garlic and alcohol)
- The actions of bacteria on the skin and clothes. There are always bacteria (germs) on the skin, which ‘feed’ on dead skin cells and sweat. Some of these bacteria make chemicals that smell unpleasant.
Washing and using deodorant can get rid of many of these smelly chemicals for a while, but they build up again every day. That is why regular bathing helps to keep germs and smells away.
Keeping the genital area clean is a very important part of daily hygiene.

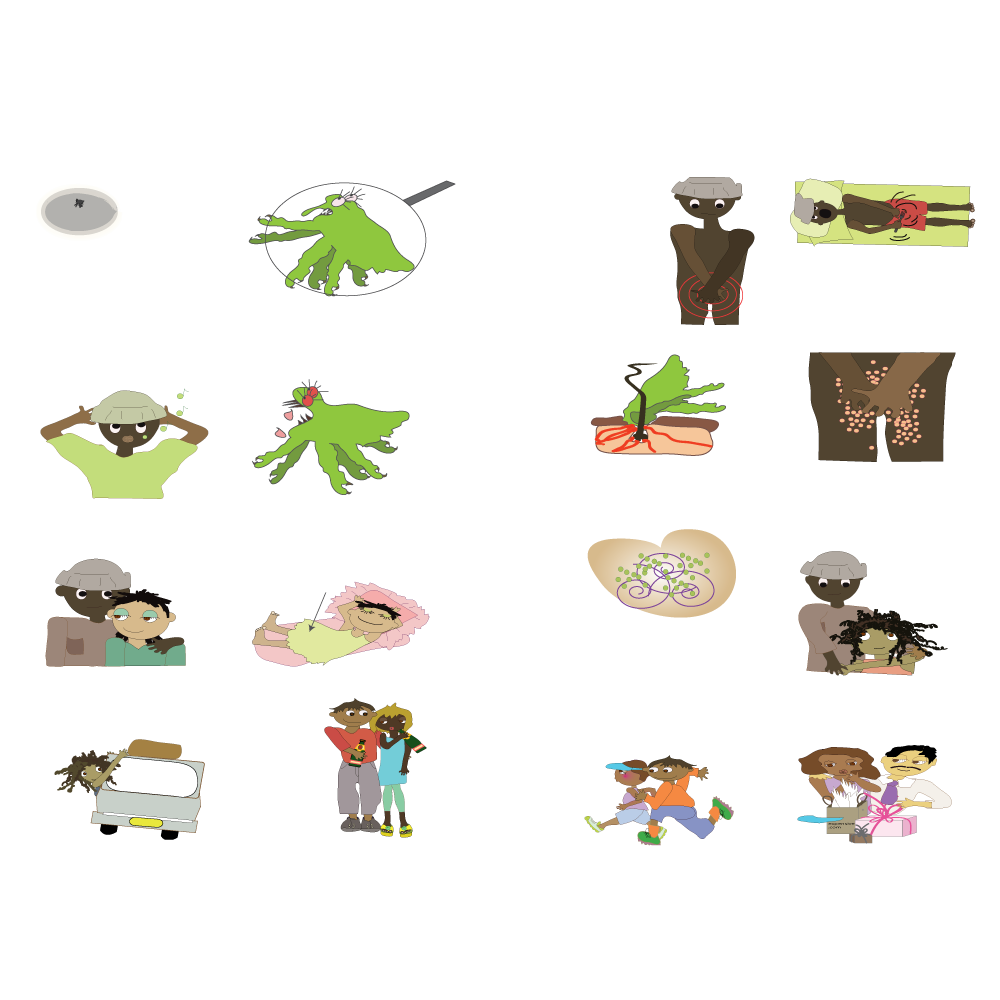
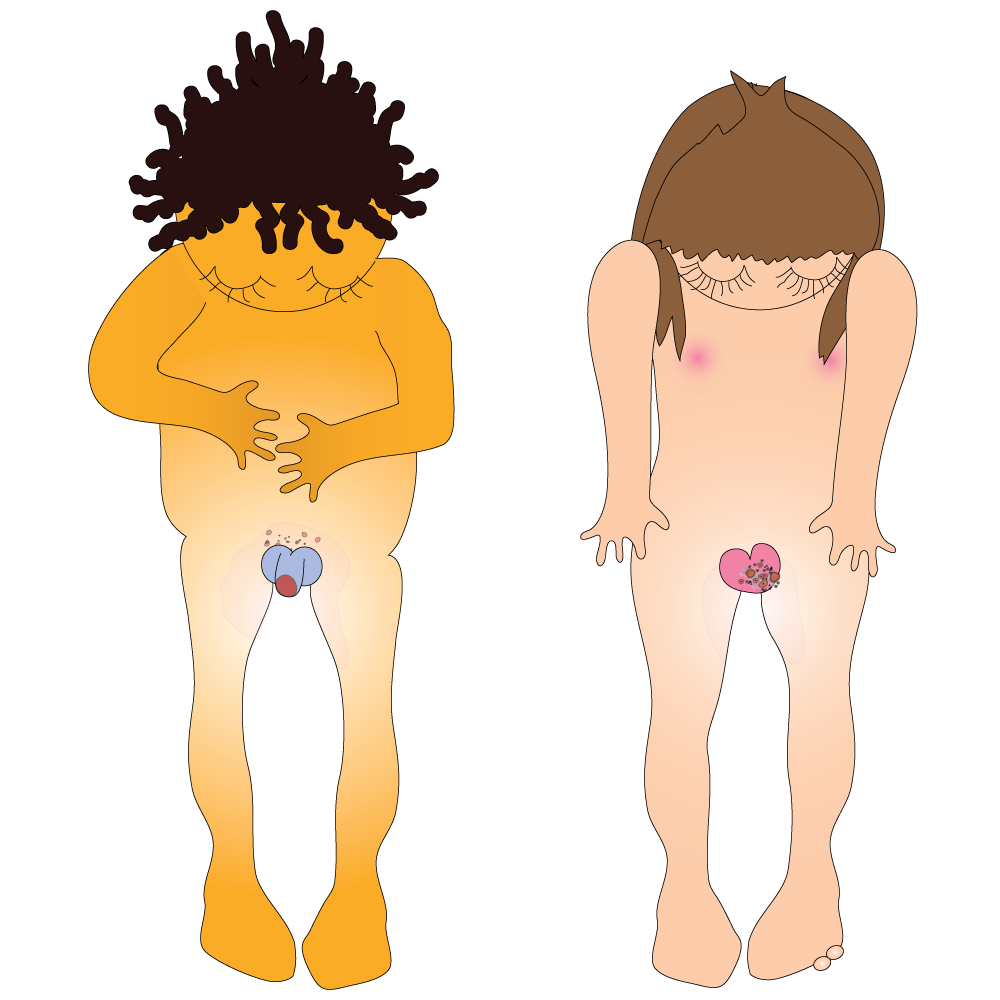
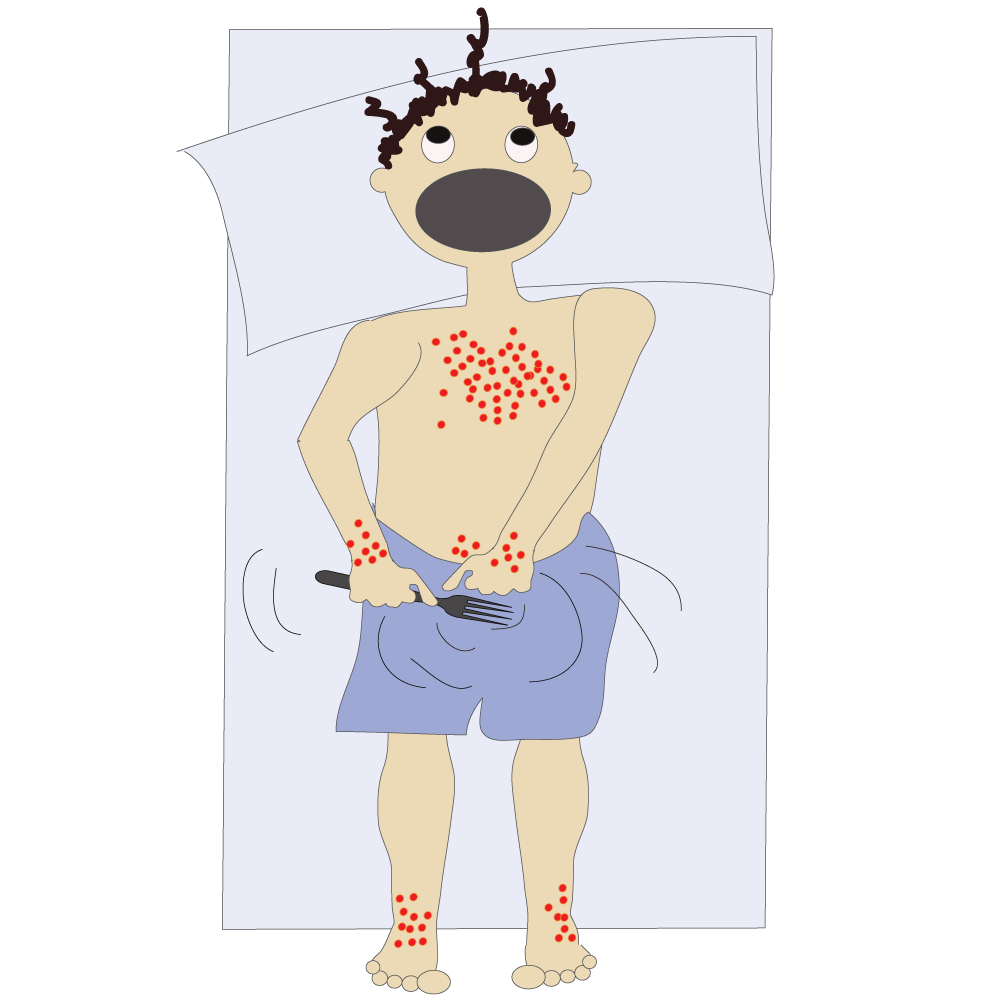
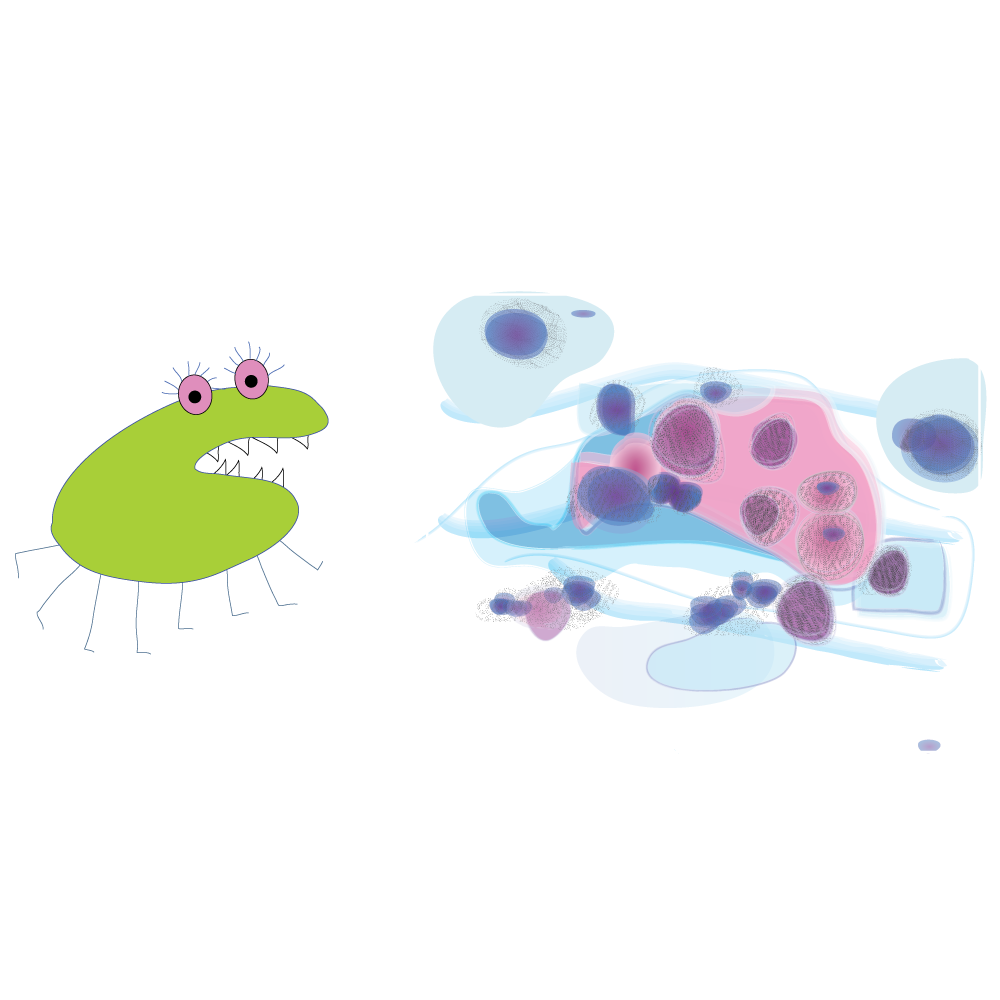
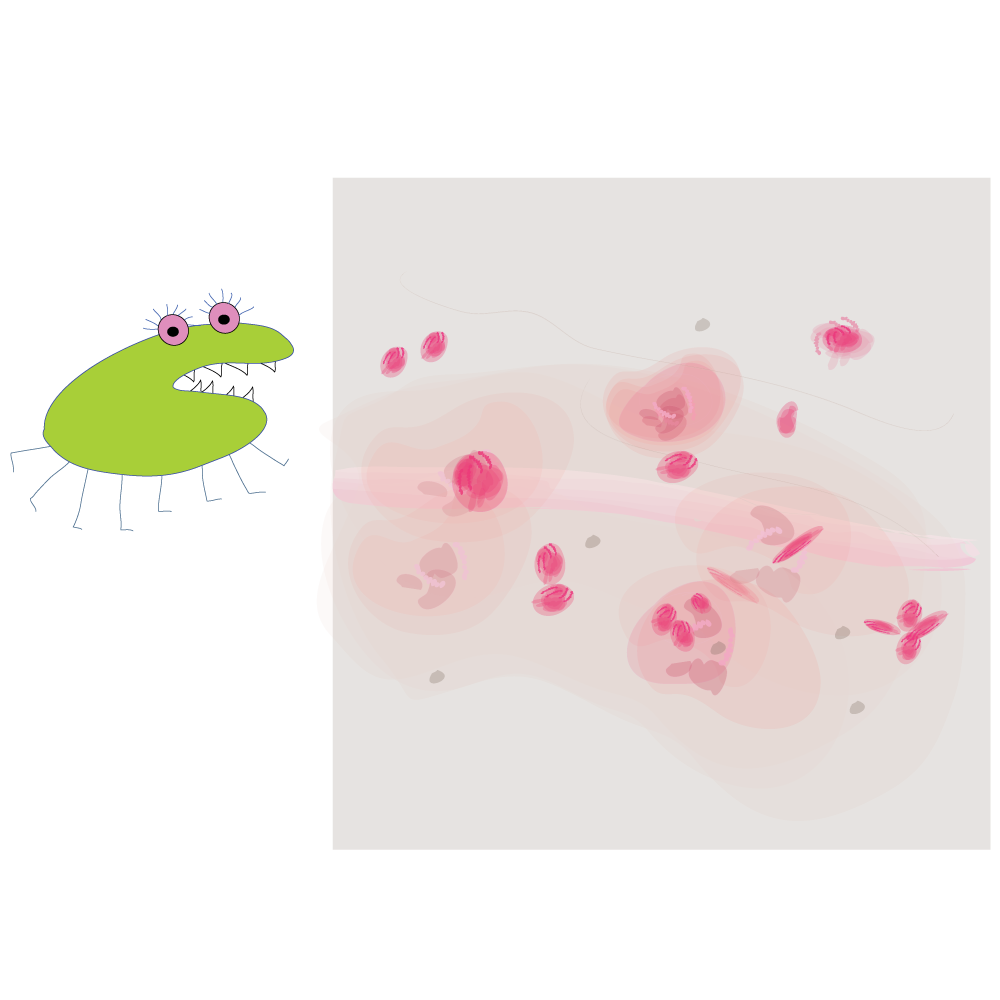
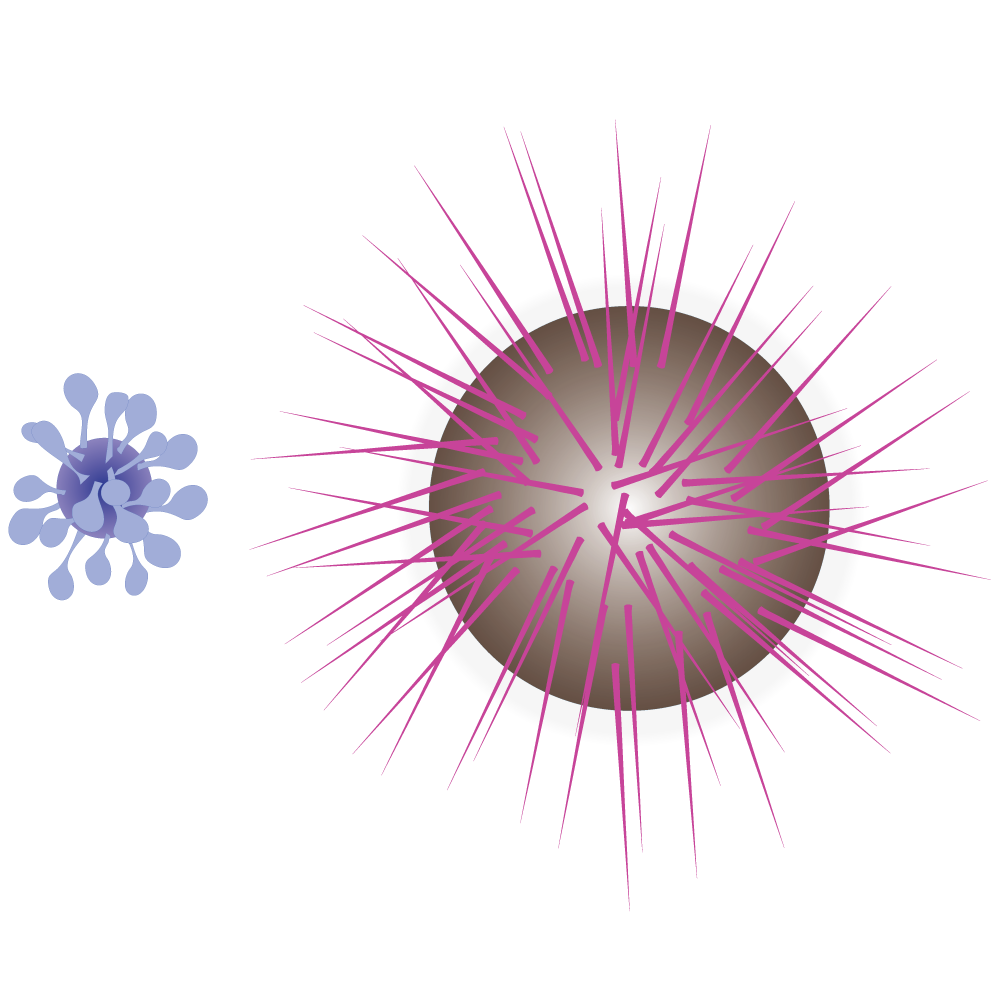
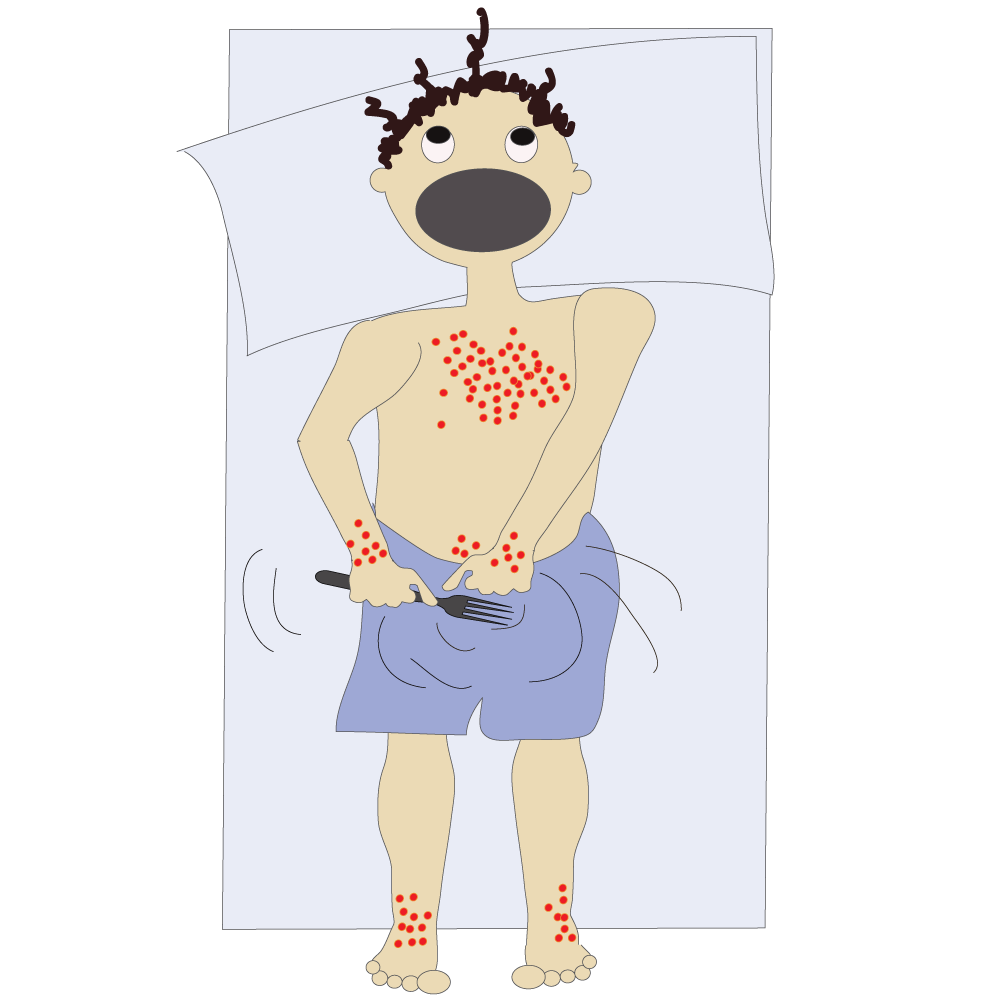
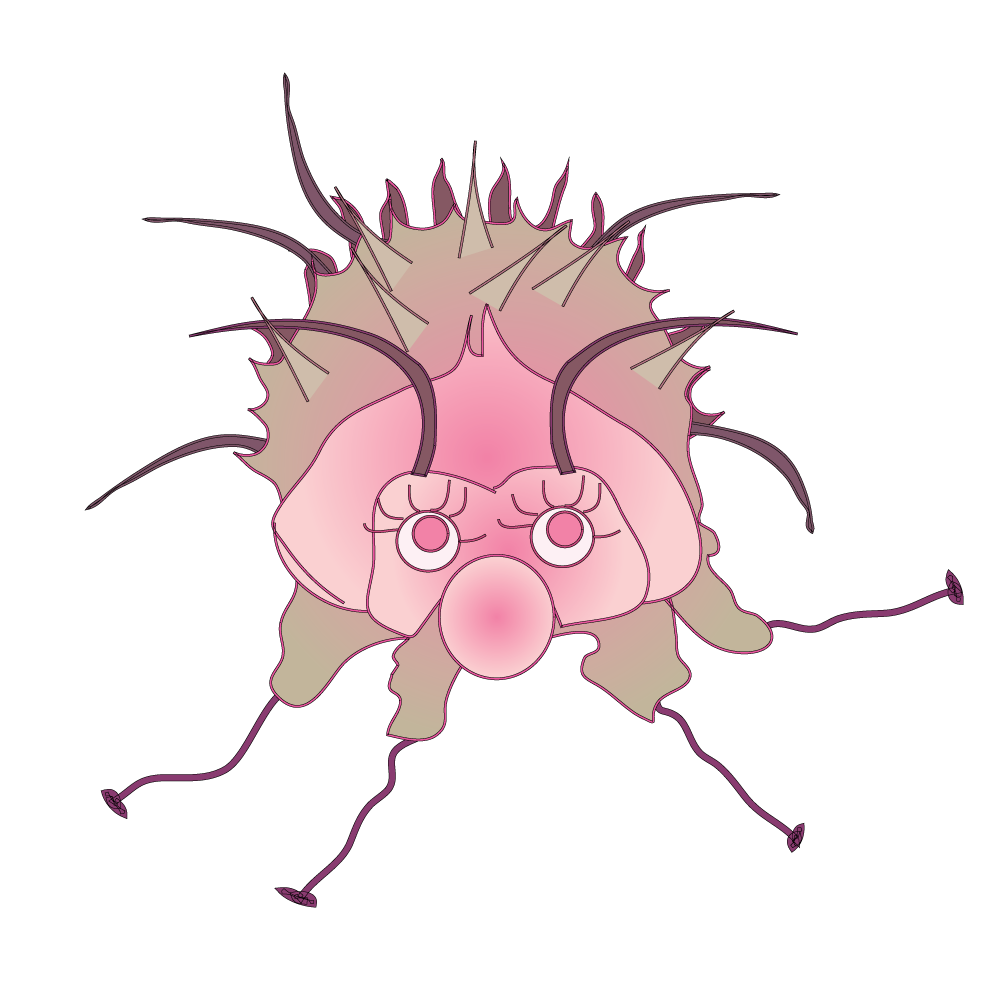
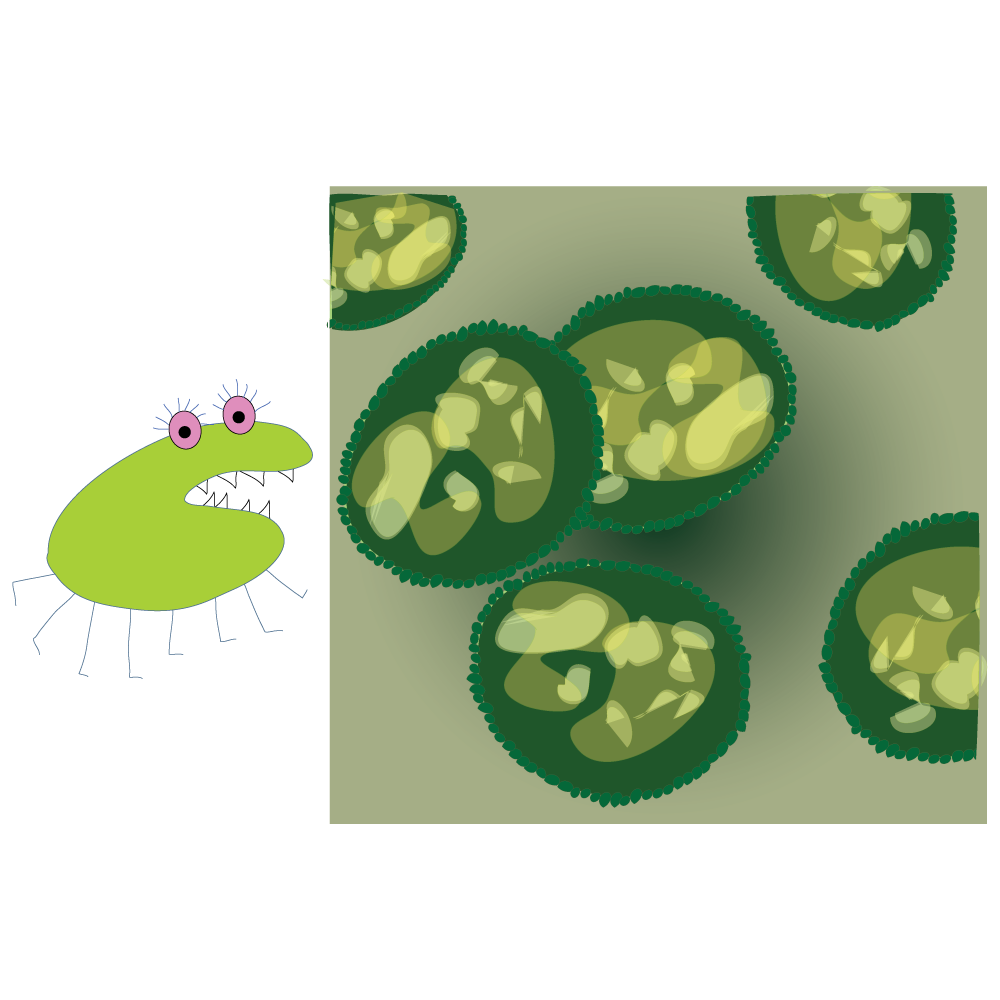
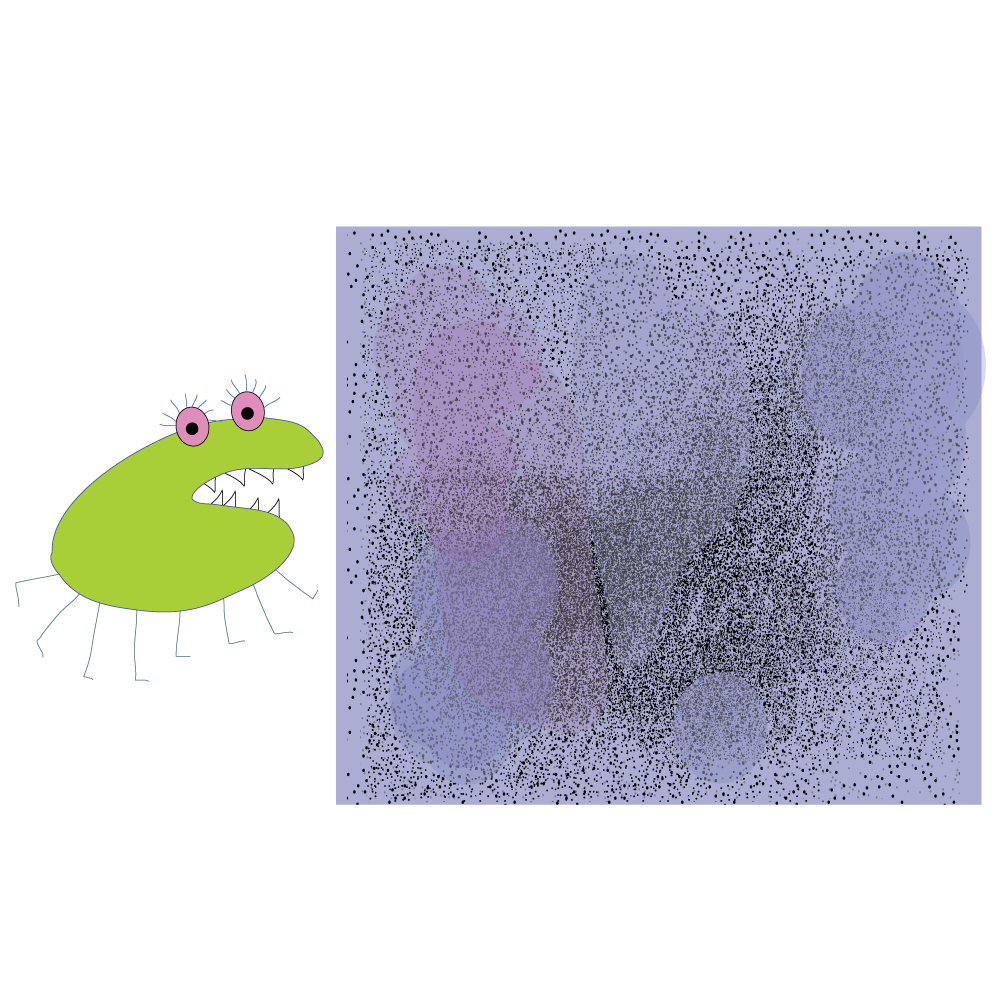
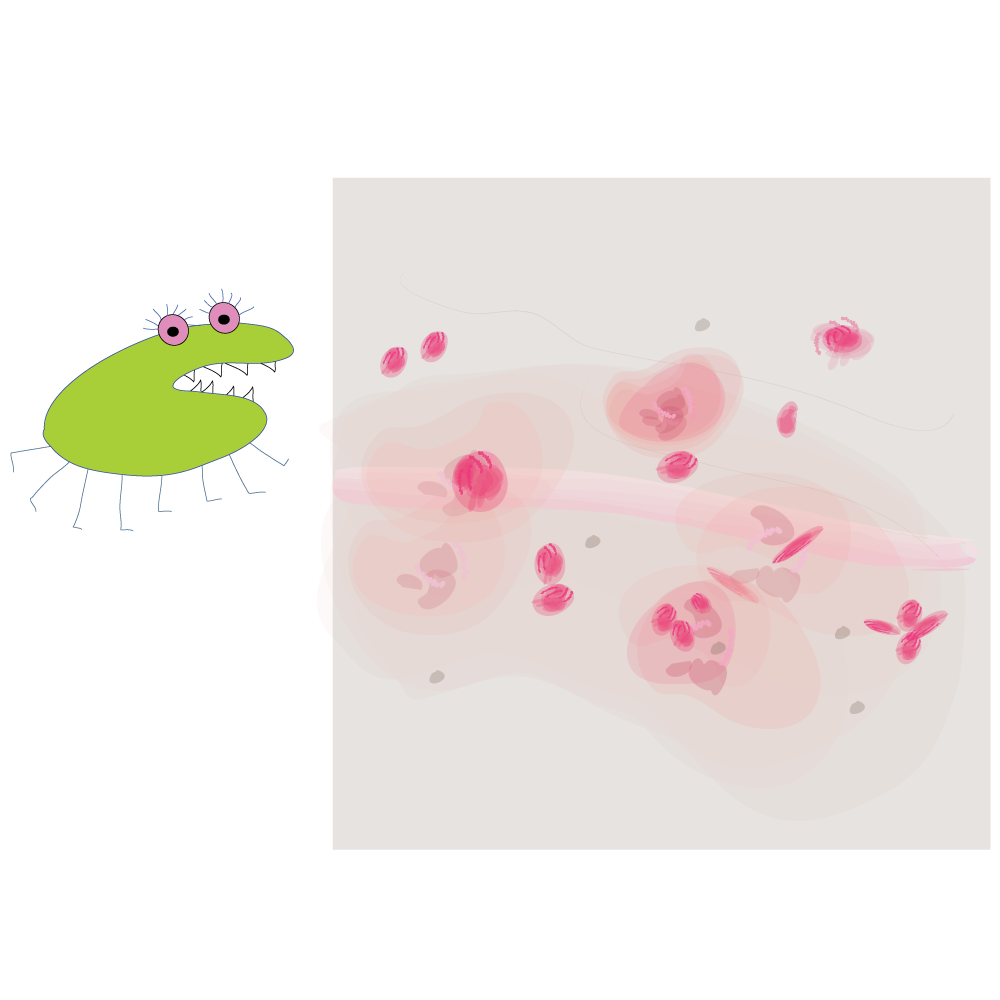
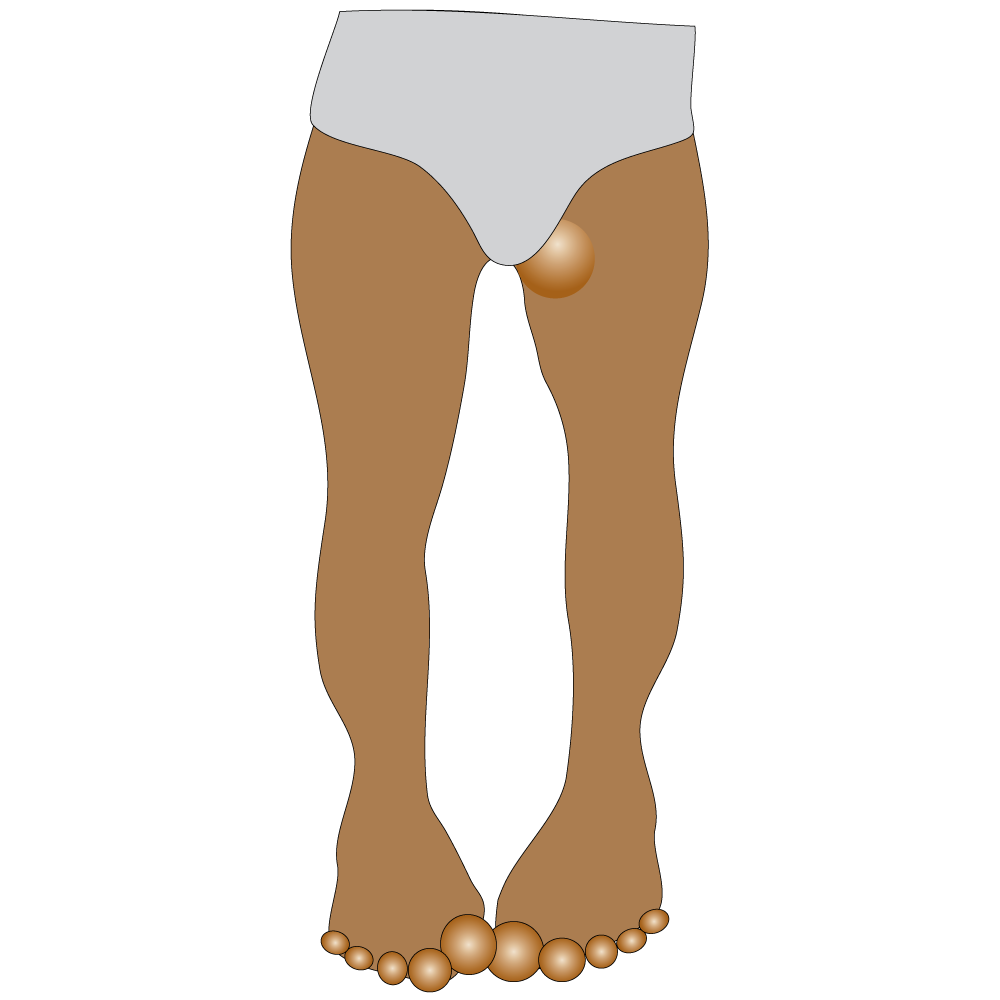
This is Pthirus, a pubic louse. He is very tiny - about the size of a pencil dot.

This is him under a microscope.
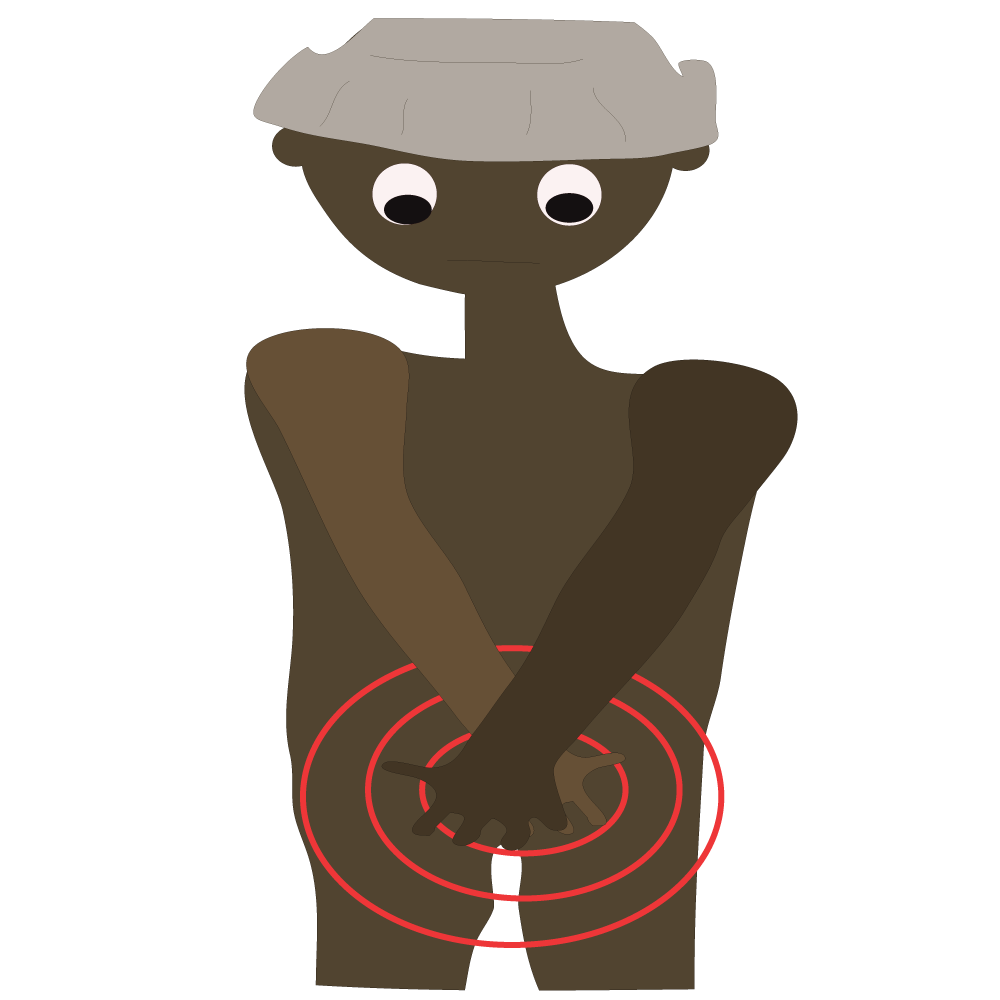
Pthirus is currently living with his family in Prophet’s pubic area. They are laying more eggs every day.
Prophet gets very itchy, mainly at night.

Prophet doesn’t know Pthirus is breeding in his pubic area.

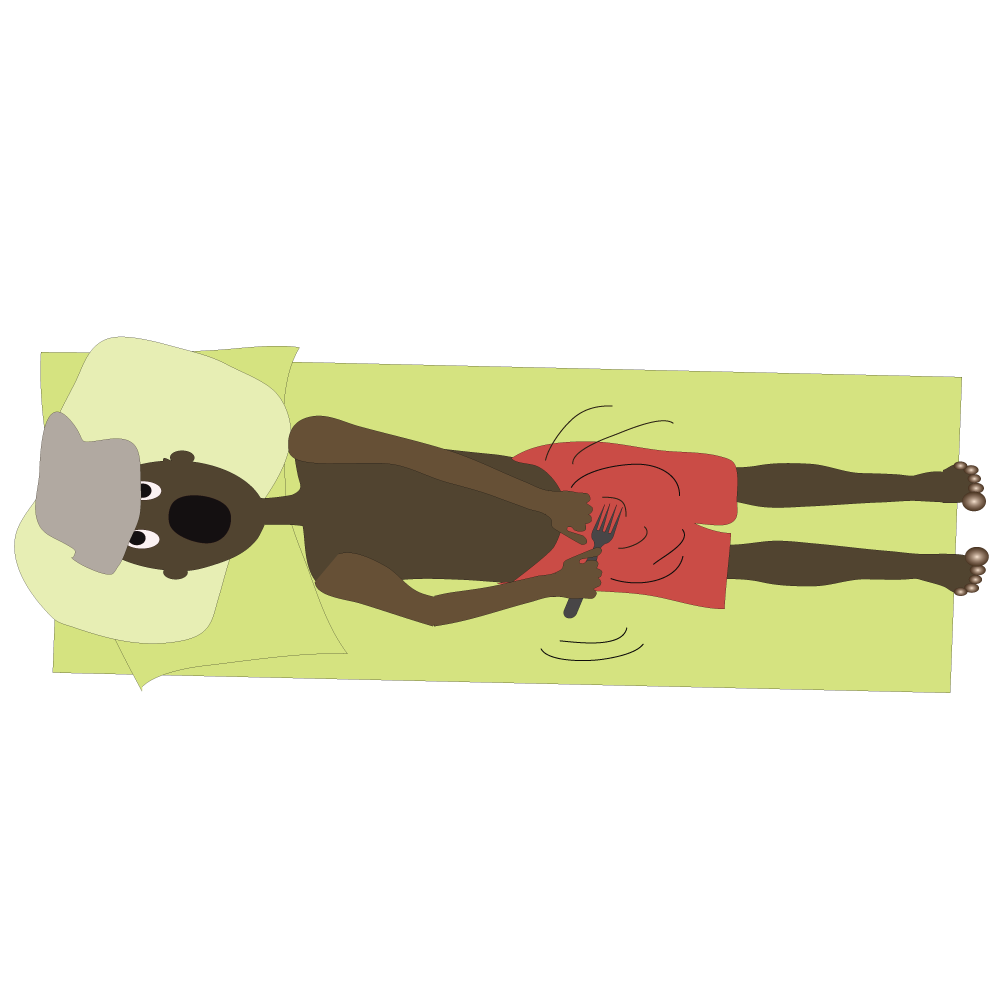
Lice get hungry at night.
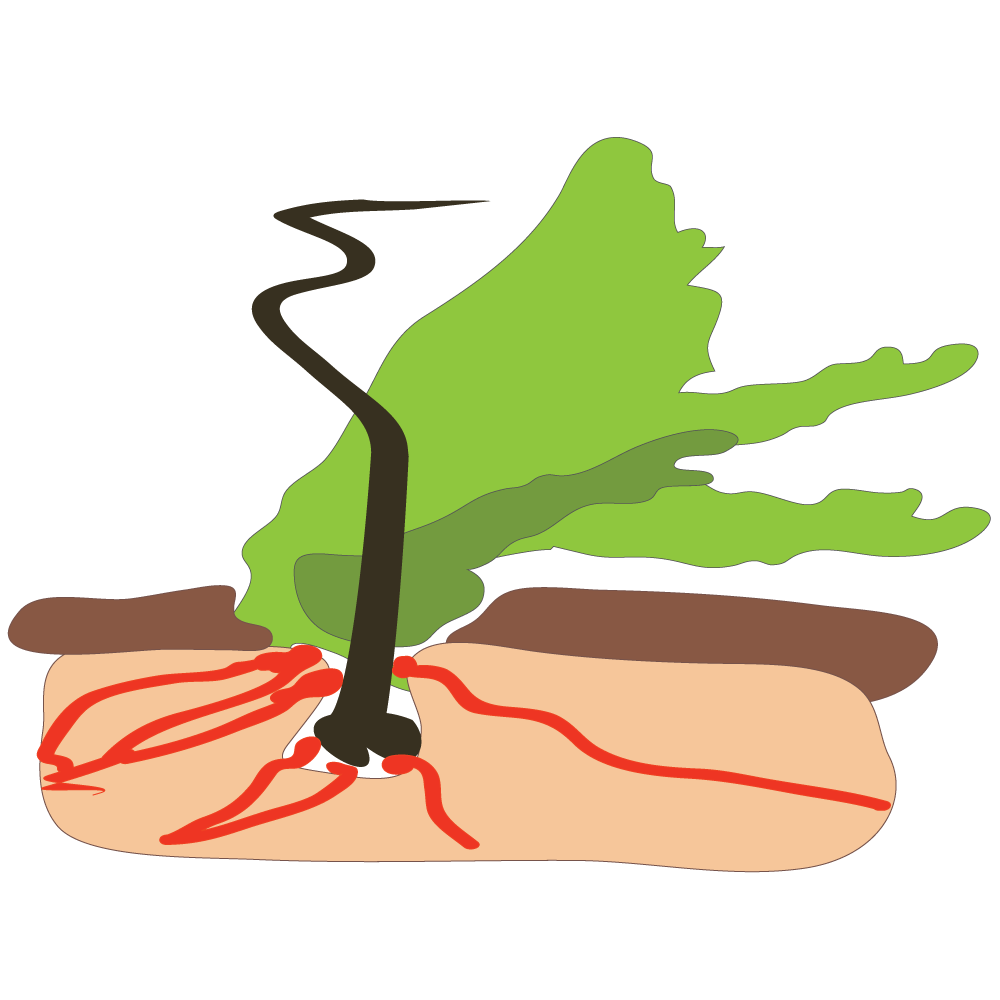
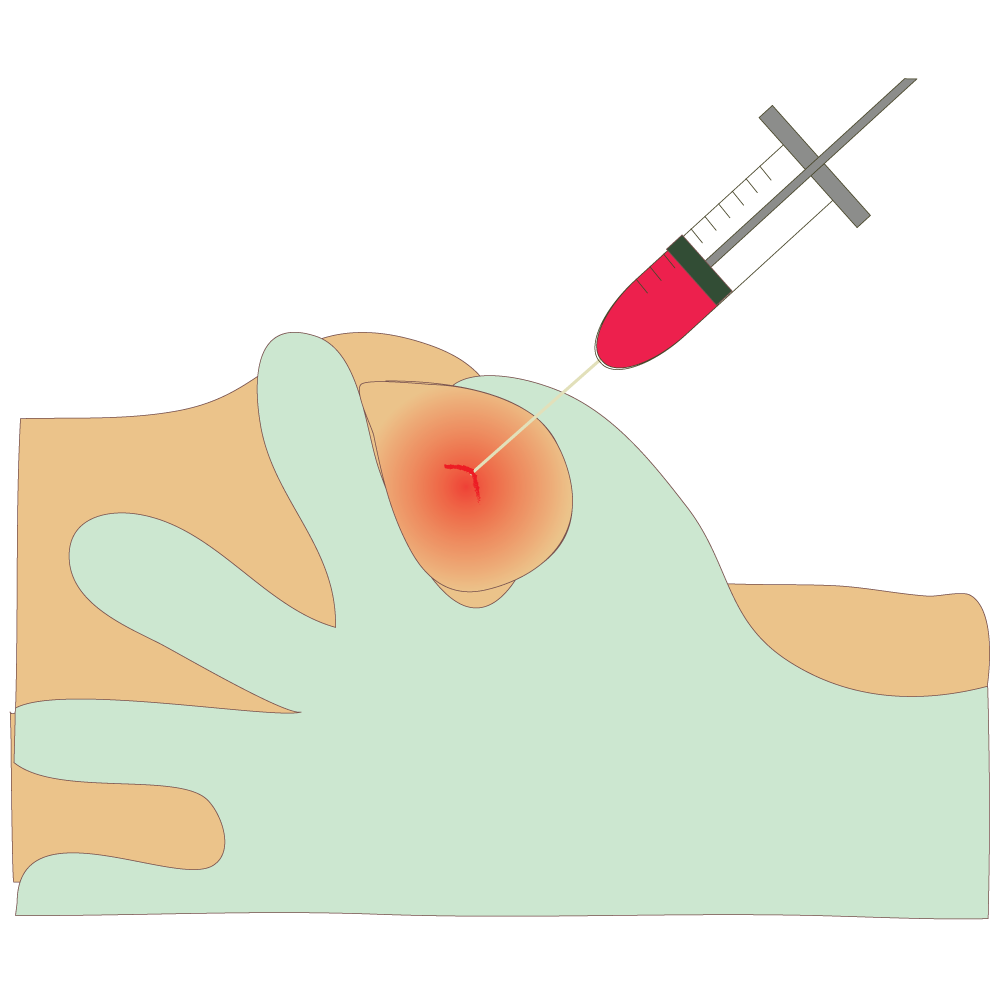
Pthirus feeding on blood inside a pubic hair follicle.
This can cause a rash.

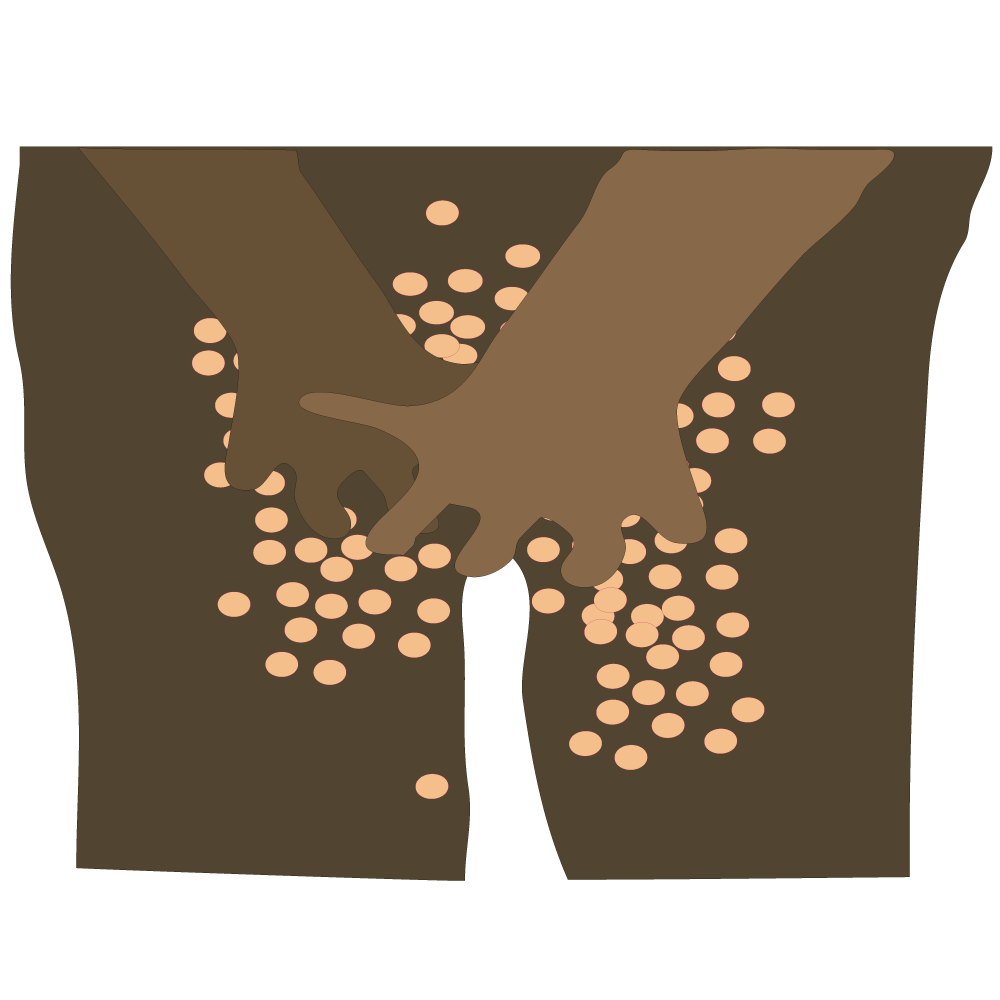
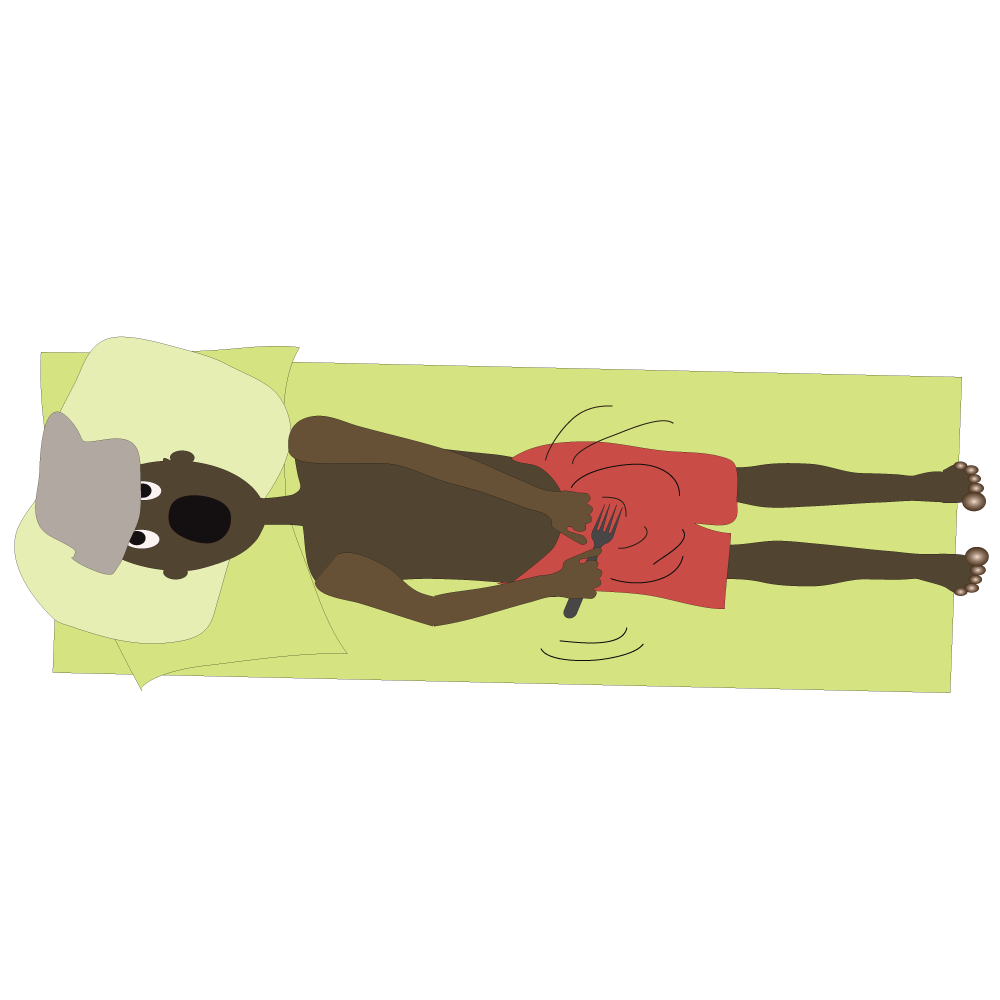
Jane and Prophet have been having sex for six months.

A few of Pthirus’ children have moved from Prophet and have laid eggs on Jane’s pubic area.
These eggs will hatch into new pubic lice in about two to four weeks.

Meanwhile - Rose comes to town and spends the night with Prophet. They are old friends.
Rose goes home to her boyfriend Peter (with extra passengers).

Peter sometimes has sex with Sibongile, who is a sex -worker.

Peter spent the weekend with Zola. They train together and have sex when Rose is away.

Zola’s boyfriend is Kenny. He is much older (and has a wife and children).
Pthirus and Pthirus’ children reproduce and spread, causing itches wherever they go!
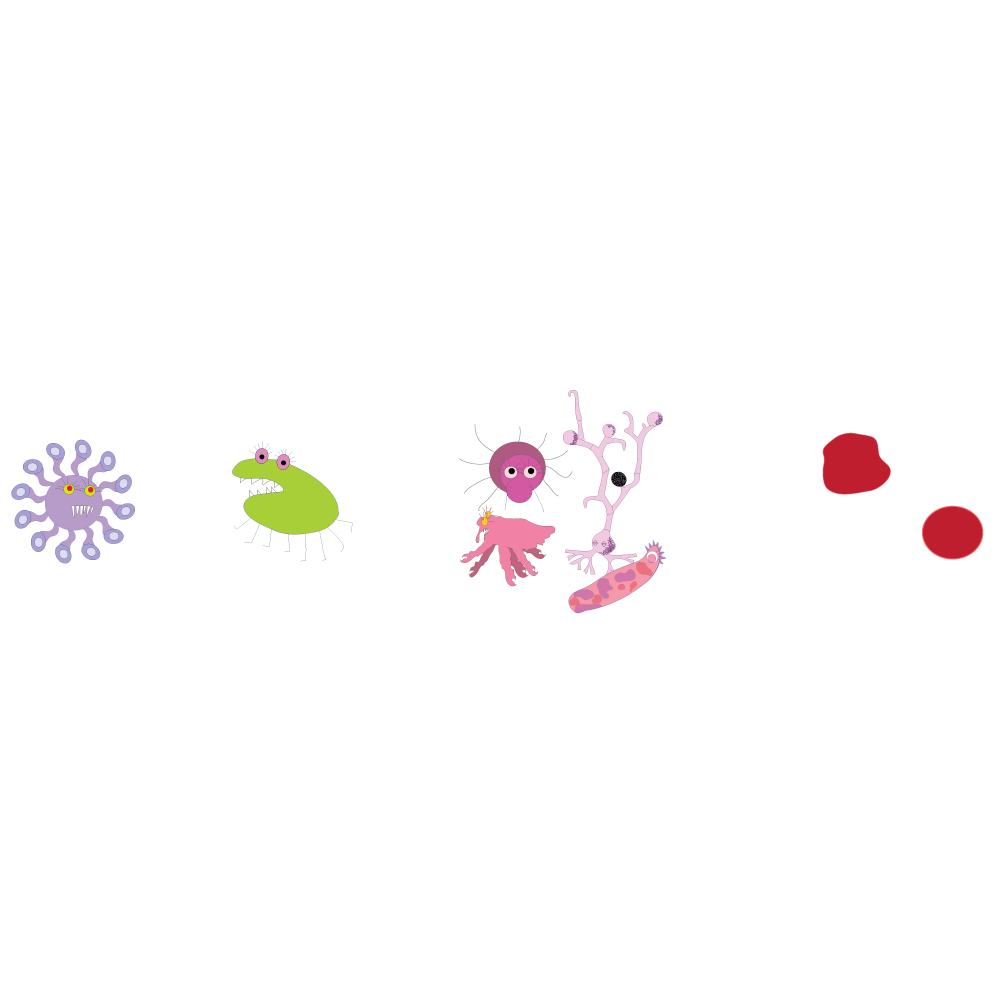
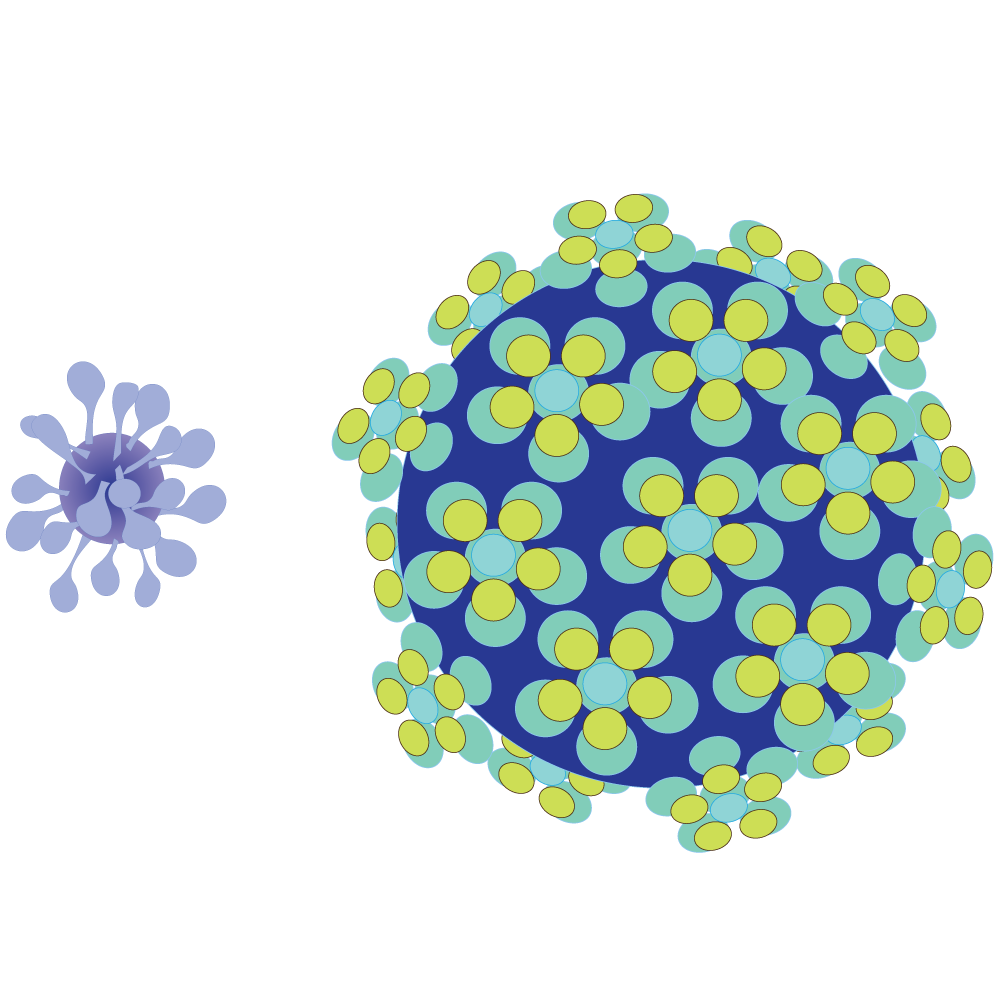
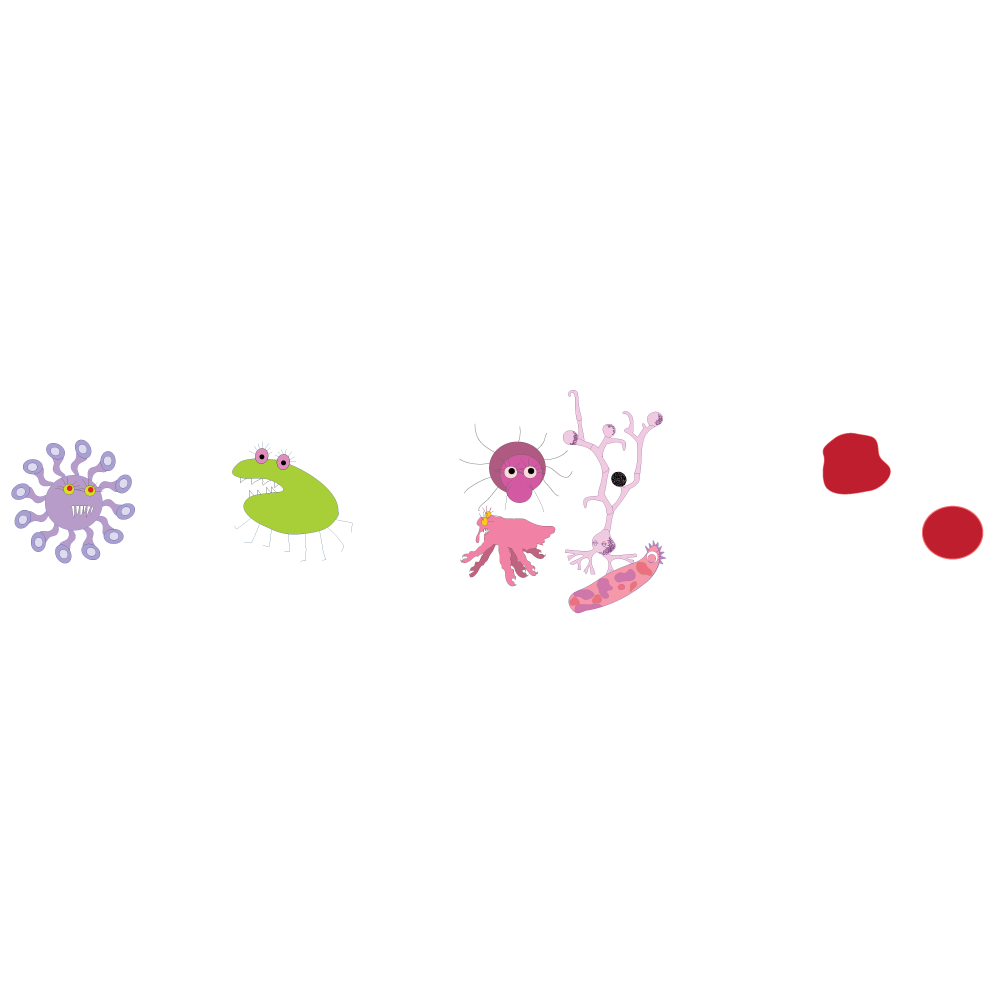
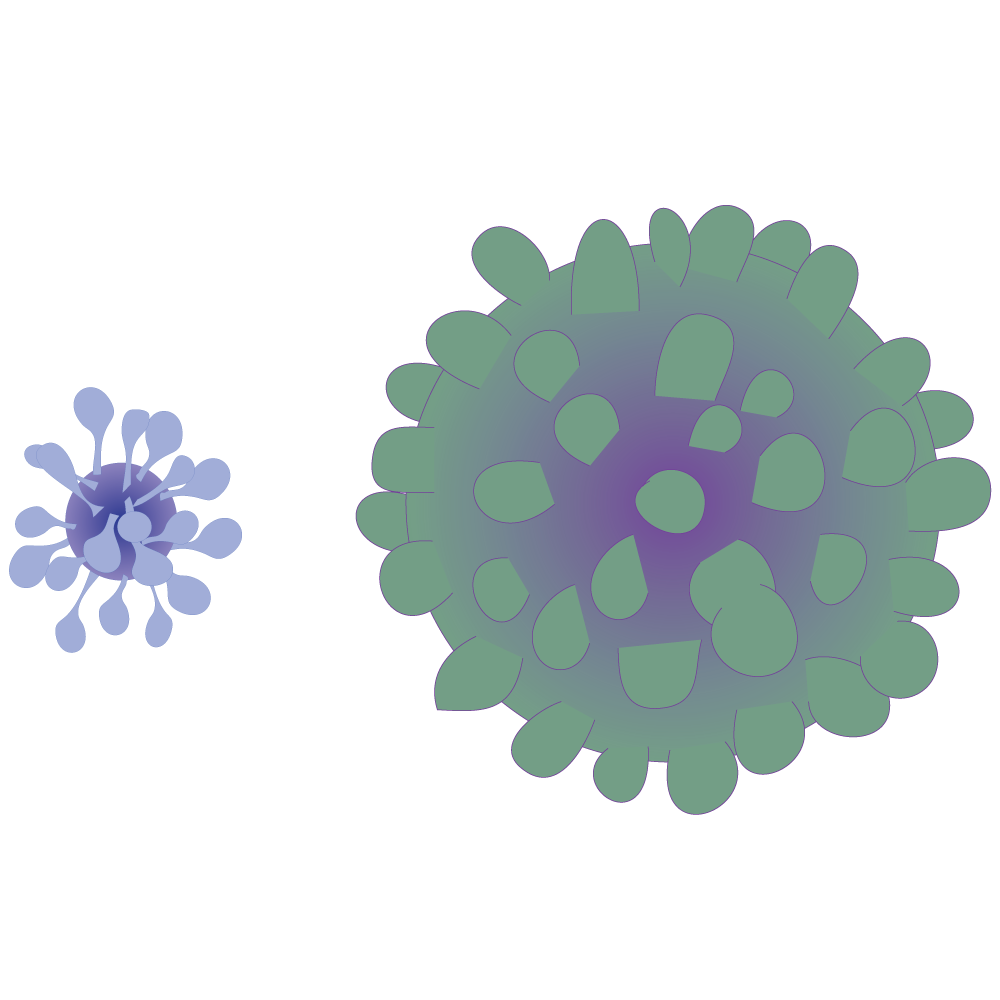
There are different types of STIs divided into three basic groups:
- Bacterial - those caused by a bacterium (germ)
- Viral - those caused by a virus
- Fungal and other - those caused by a fungus or parasite or protozoa
Genital herpes, HIV and HPV are caused by a virus.
Non-viral STI’s such as chlamydia, trichomoniasis, gonorrhoea, syphilis and chancroid can be successfully treated with antibiotics.
Infection with STI’s can lead to infertility, problem pregnancies and cervical cancer, as well as the death of infants and adults.
Some of the different names for STIs: The drop, the itch, gonorrhoea, bad blood, syphilis, crabs, HIV, morning drip, herpes, fever kiss, the clap, VD, cystitis
- Pubic lice (Crabs)
- Bacterial vaginosis
- Chlamydia
- Genital herpes
- Gonorrhoea.
- Hepatitis B and C
- HPV - Human papillomavirus infection
- Lymphogranuloma Venereum (LGV)
- Scabies
- Syphilis
- Chancroid
- PID - Pelvic inflammatory disease
- Trichomanias
- Yeast infections
There are many different STIs, and they fall under different classifications.
Most Sexually Transmitted Infections will only affect you if you have sexual contact with someone who has an STI. There are however some infections, like scabies, which are referred to as STIs because they are usually transmitted sexually but can also be passed on in other ways.
You will see how many of these infections often don’t have obvious symptoms and how easily they can therefore be passed - onto you or on by you.
Infections are divided into three main headings:
- Parasites and other
- Bacteria
- Virus
The only 100% safe prevention method is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a trusted partner.
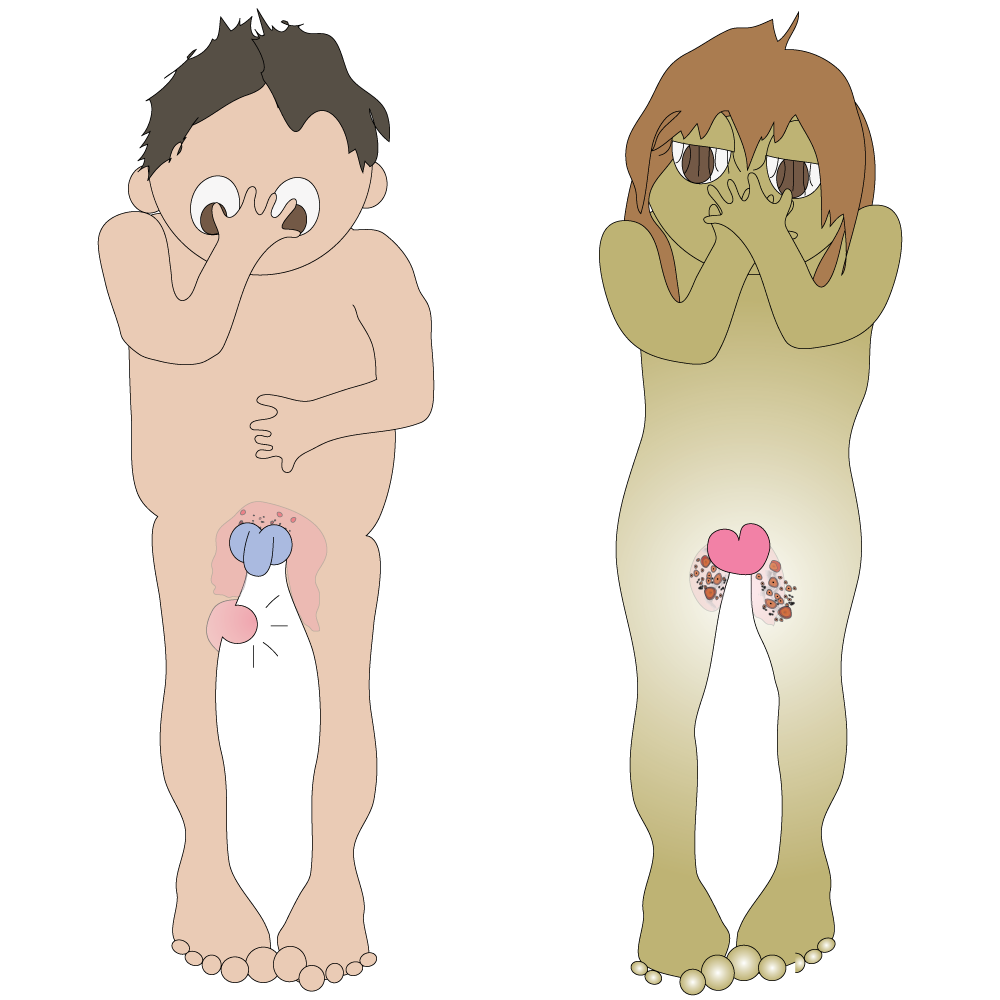
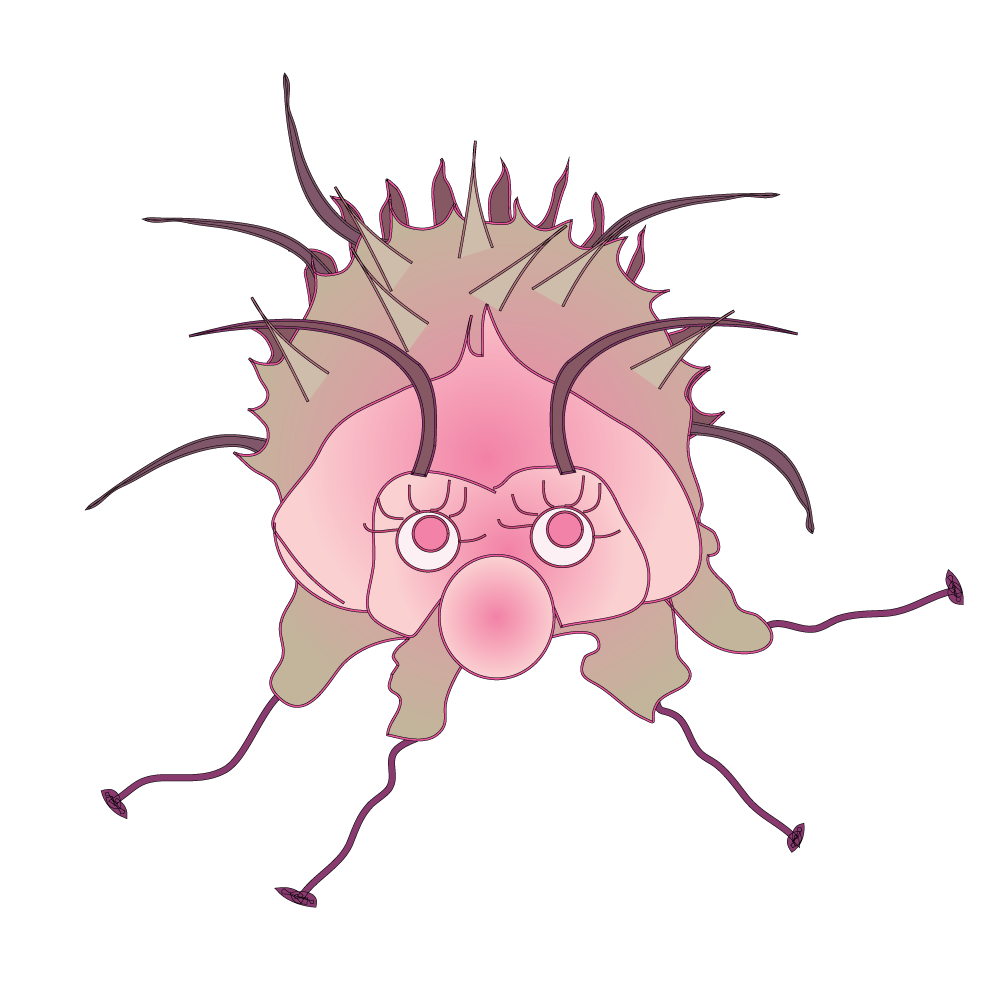
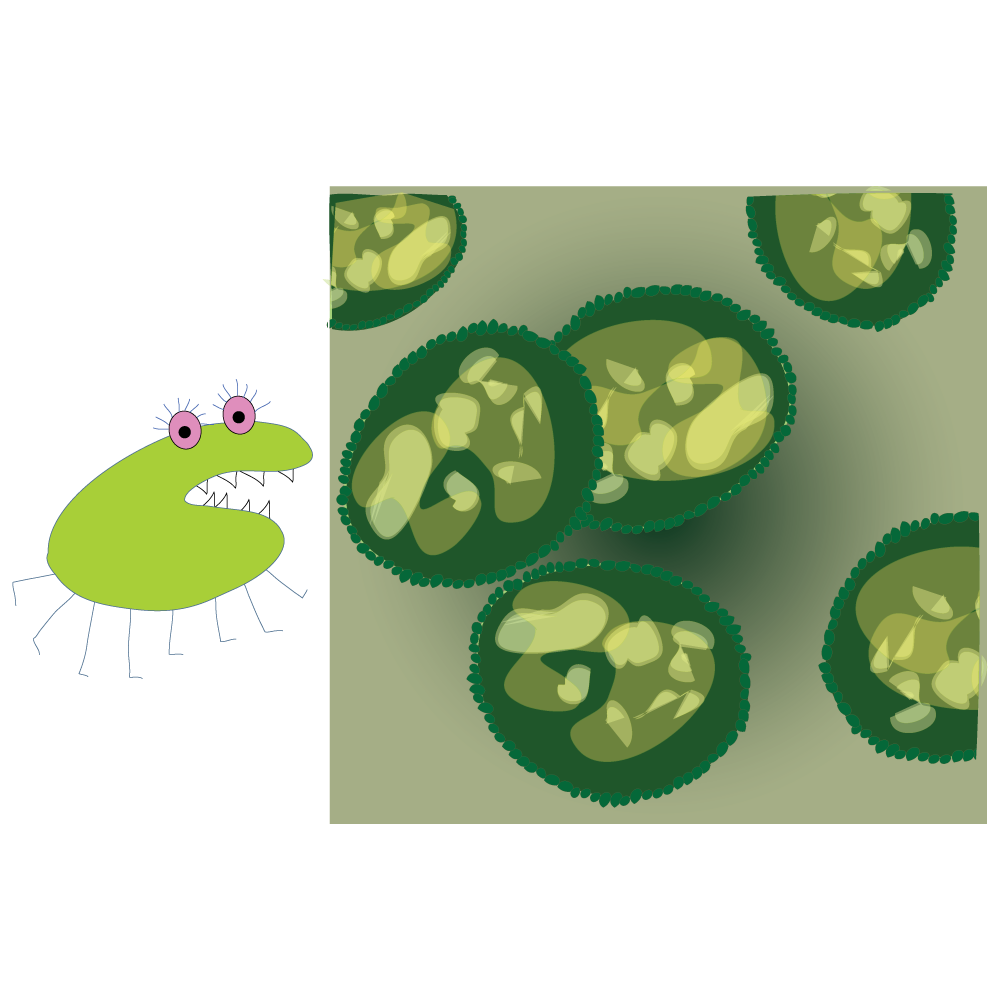
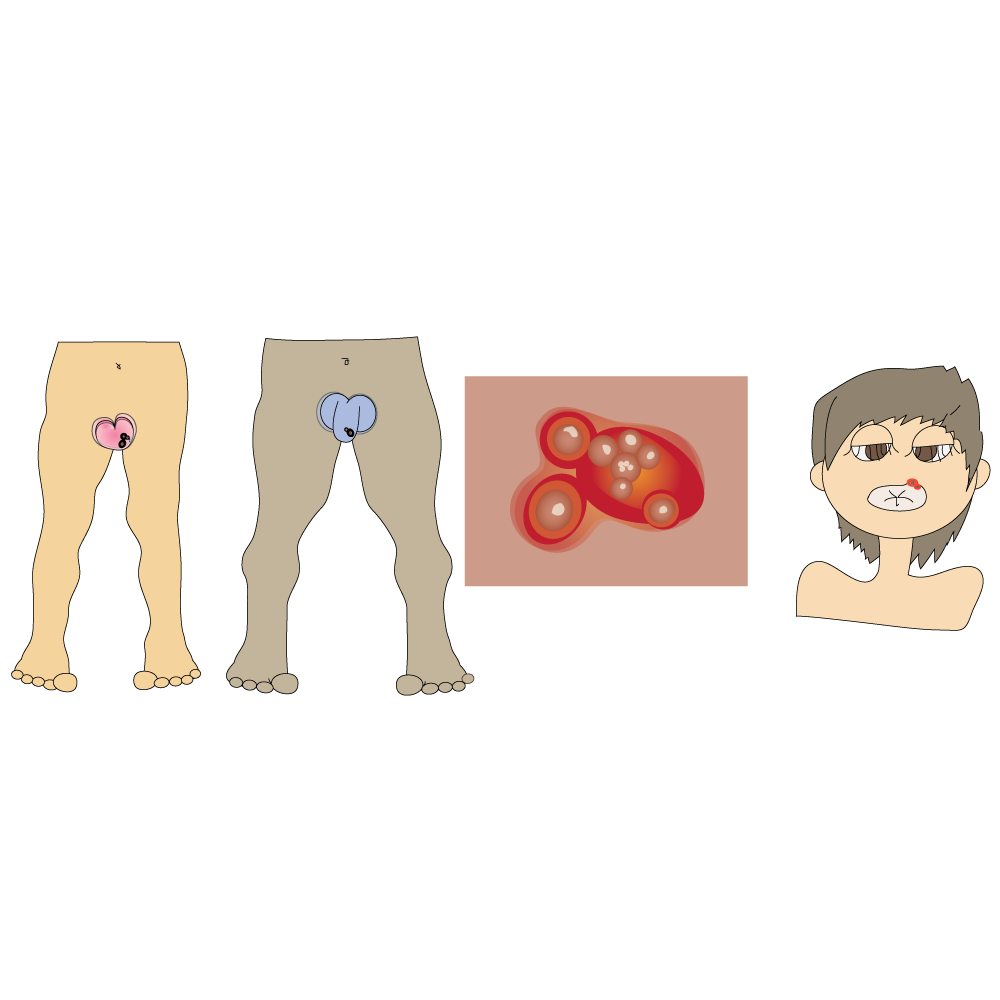
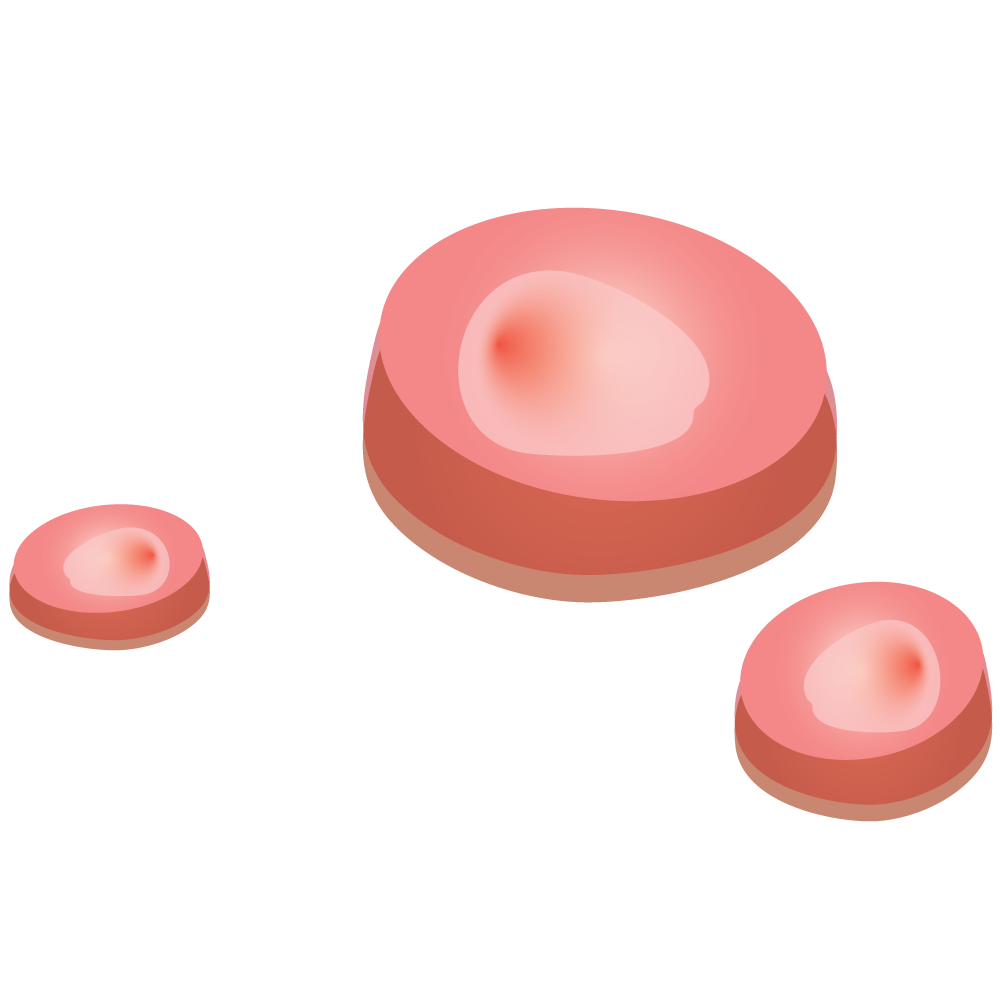
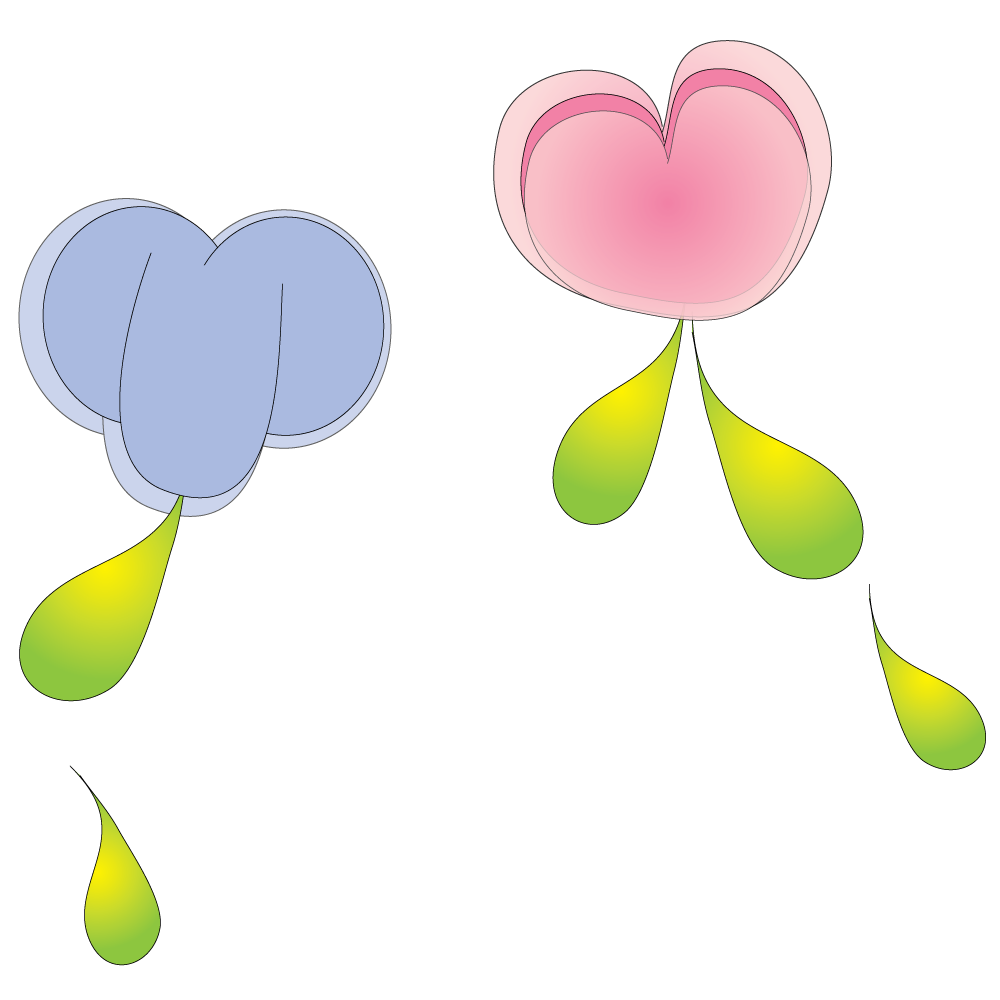
Name: Pubic Lice (crabs)
Type: Parasite
Description: Small yellow/grey crab-shaped parasites that burrow into the skin to feed on blood. They live on coarse body hair (usually pubic hair, but can also be found in armpit hair, facial hair and even on eyelashes). They use their crab-like claws to grip hair strands.
Cause: Sexually transmitted and can also be passed on through sharing clothes, towels, or bedding with someone who has them.
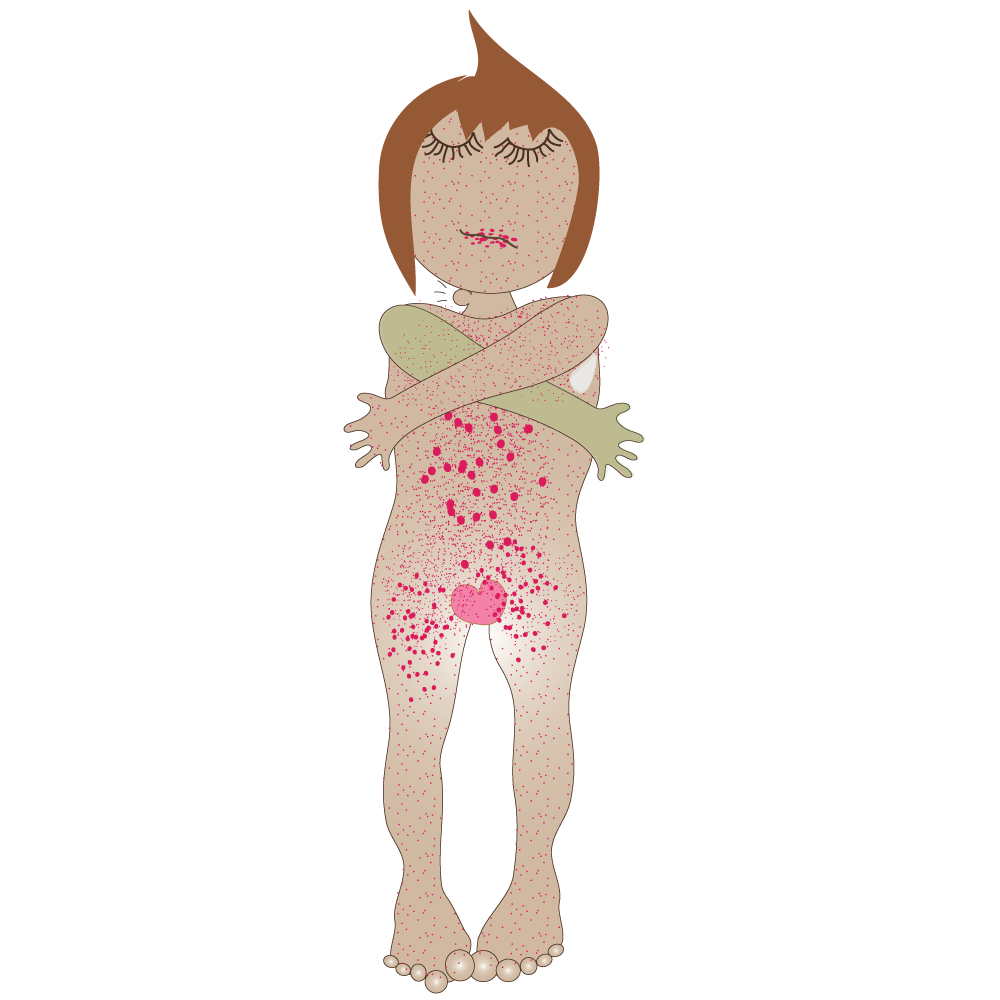
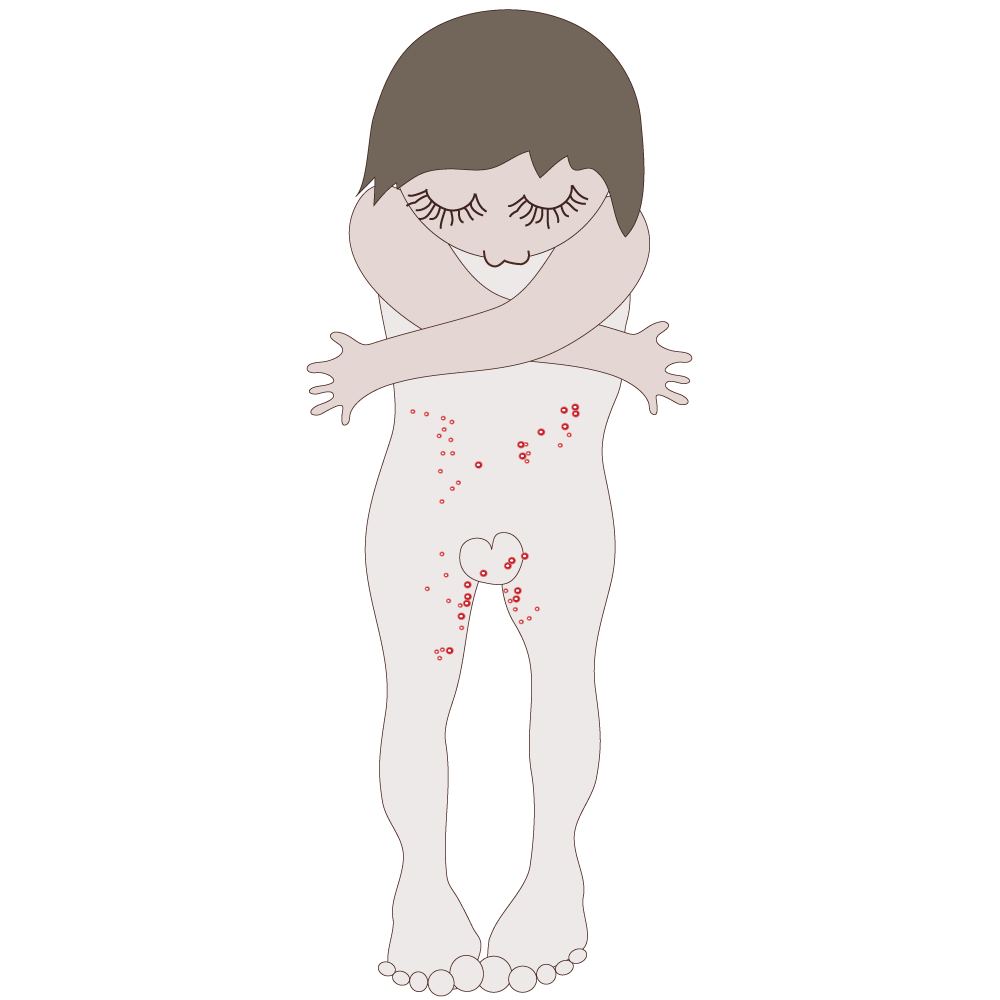
Symptoms: Live in the hairy parts of the body. Usually noticed 5 days to 7 weeks after infection. Sometimes the eggs can be seen, and lice can be spotted moving on the skin. Itchy mostly at night. Itchy red spots or rash on wrists, ankles, hands, genitals, chest and back.
Curable: Yes
Prevention: There is no effective way to prevent becoming infected during sex. A person who has crabs can reduce the risk to others by washing bedding, towels, and clothes (very hot water) to kill off the parasites.
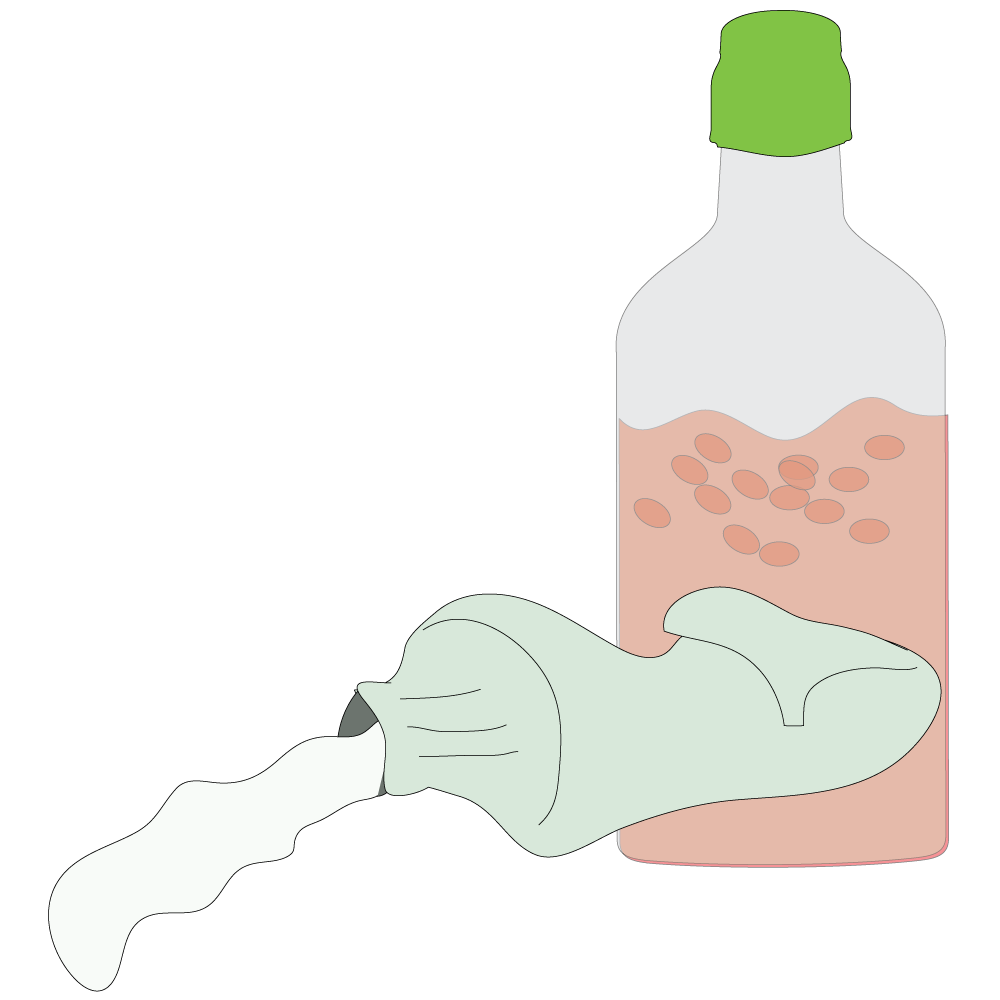
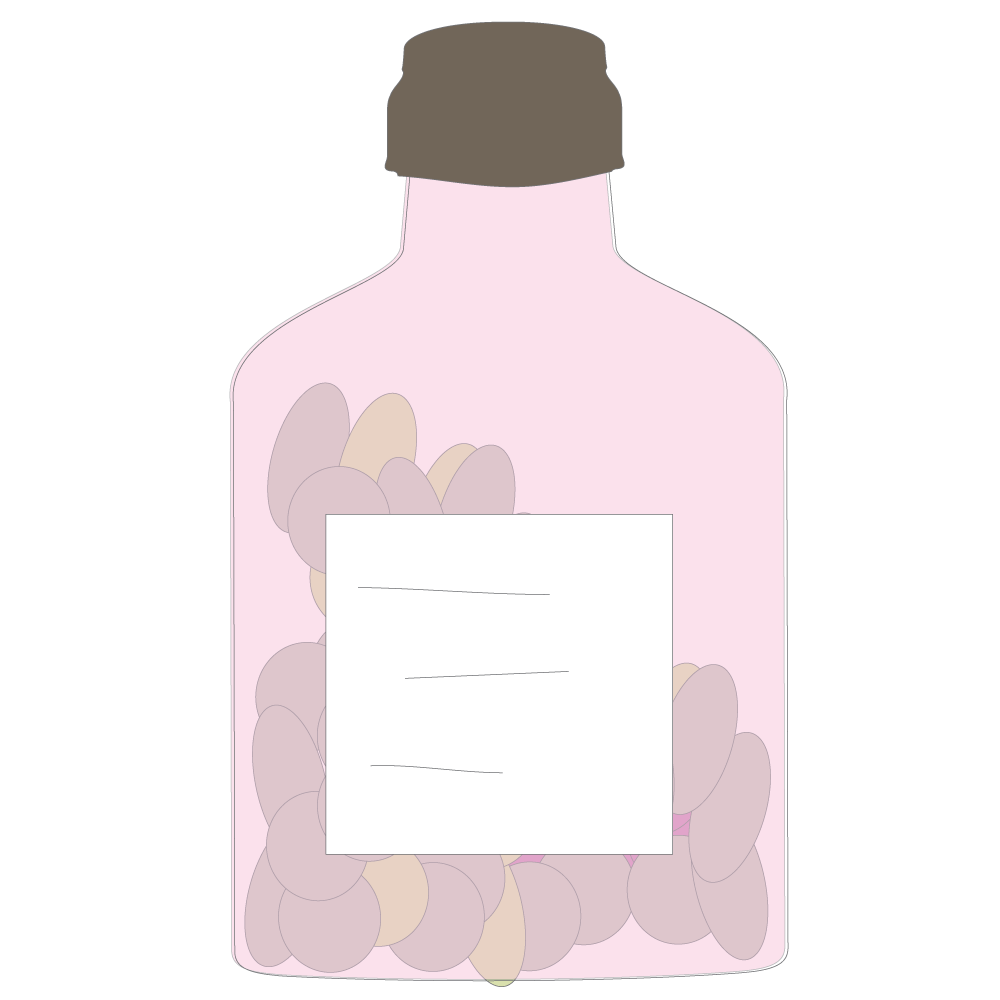
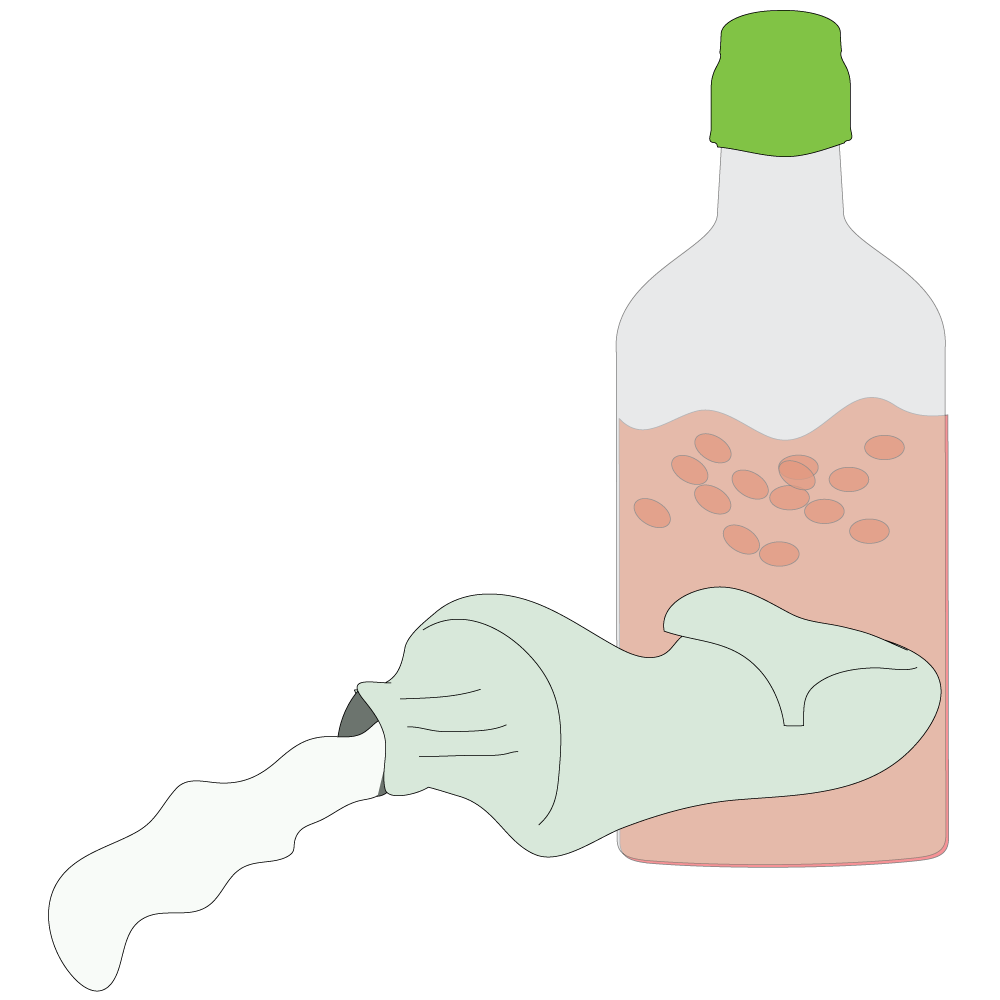
Treatment: Special shampoos, lotions and creams that kill the lice and their eggs. It’s not necessary to shave pubic hair as this is unlikely to remove all lice. Treatment might need to be repeated if all the eggs are not killed.
Name: Scabies
Type: Parasite
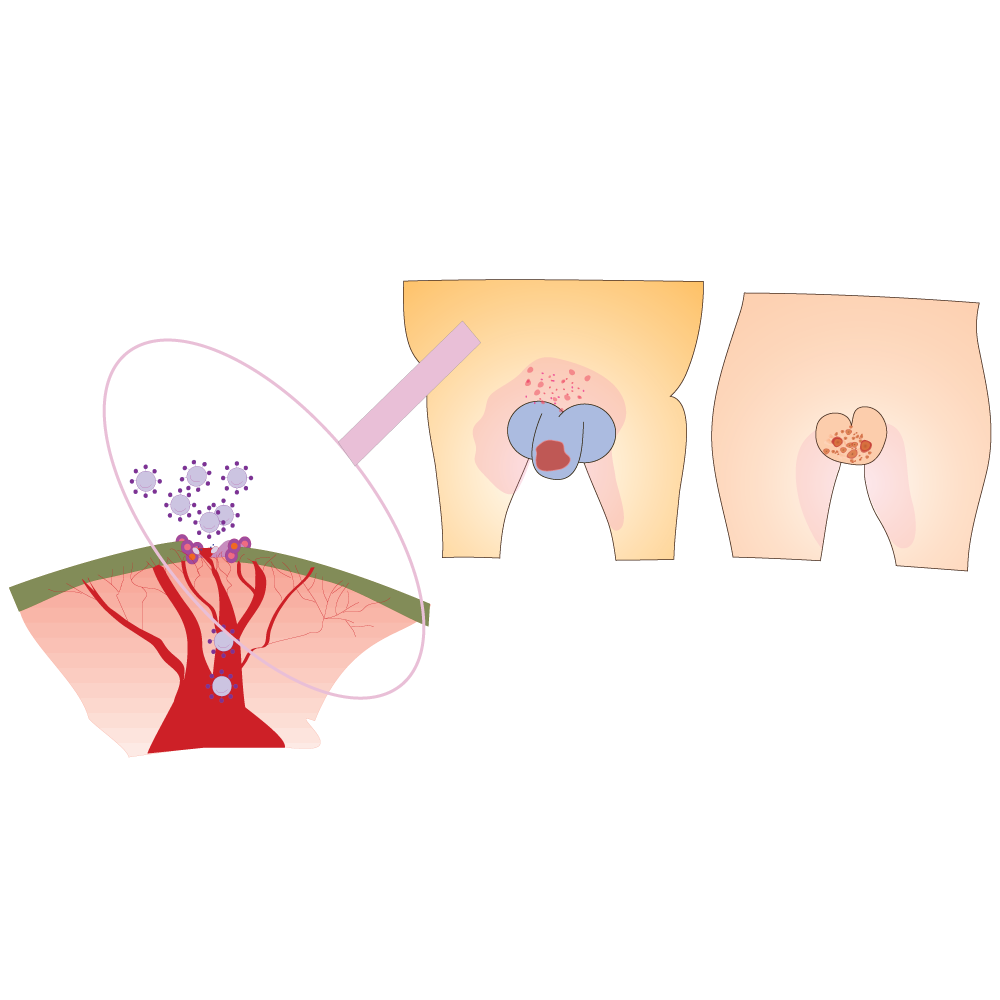
Description: An intensely itchy, contagious skin infestation of the parasitic mite. The adult female mite is barely visible to the human eye, with the male being half that size. Female mites burrow into the outer layer of the skin to lay eggs.
Cause: Sexually transmitted but can also be passed on by prolonged direct skin contact. Can spread rapidly in crowded conditions.
Symptoms: Symptoms begin 2-to-6 weeks after infection. Burrows appear as wavy lines (±15mm) in length. Usually occur on the webbing between fingers and toes, on the genitals, around the anus or on the buttocks, elbows or wrists.
Very itchy rash of inflamed pimple-like lumps – an allergic reaction to the mites, their eggs, and faeces. Itching, particularly at night or after baths when the body is warmer, as a reaction to the mites.

Curable: Yes
Prevention: There is no effective way to prevent infection, apart from avoiding direct skin contact with an infected person. An infected person can prevent the infestation spreading by washing clothes and bedding in a very hot wash to kill the mites.

Treatment: All people staying in the same household should be treated with cream /lotion from pharmacy or clinic.
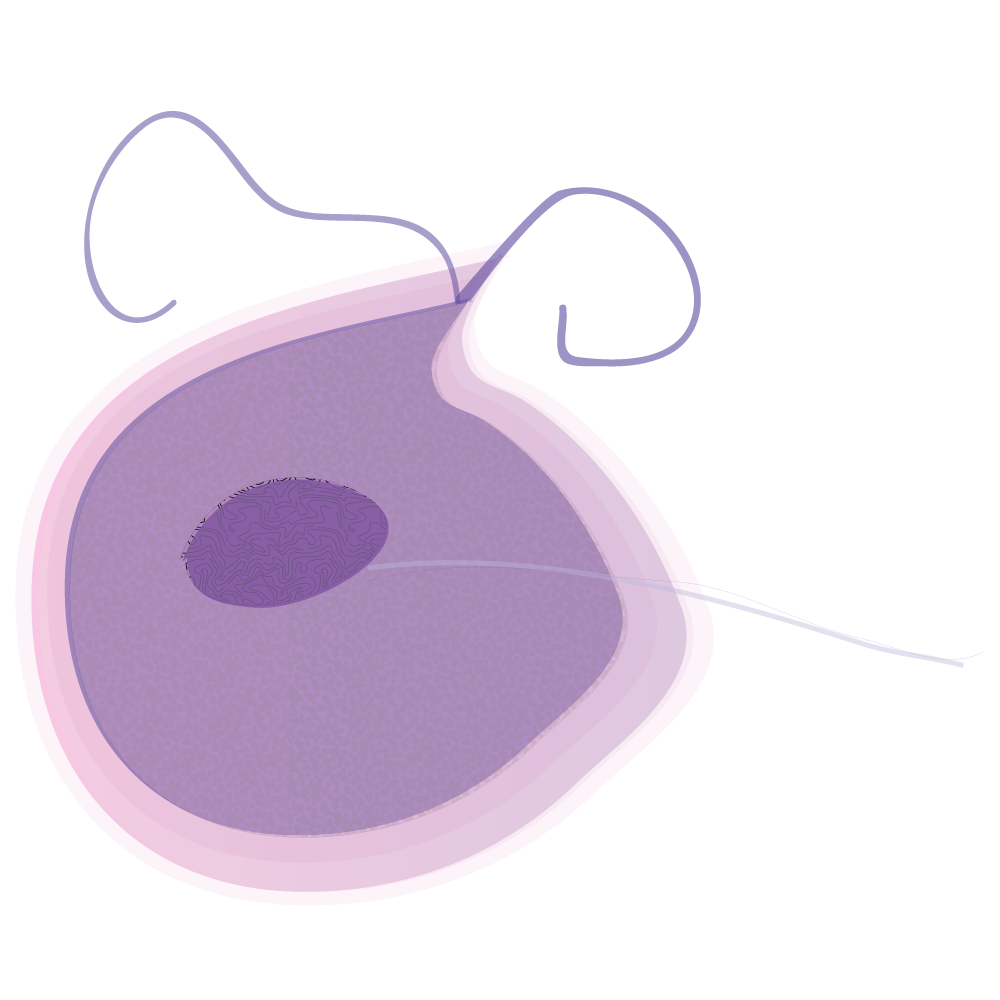
Name: Trichomoniasis (“trich”)
Type: Parasite
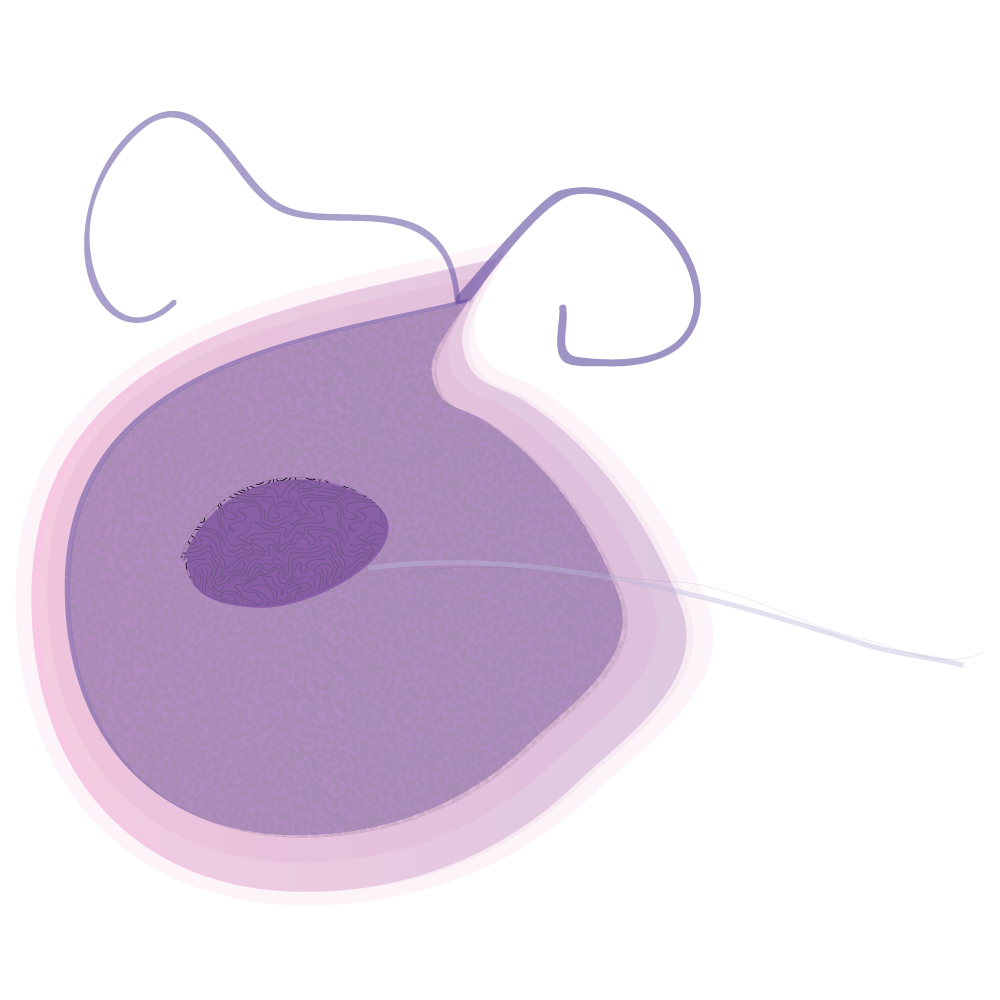
Description: A very common STI caused by a parasite (Trichomonas Vaginalis). Symptoms of the disease vary but most people who have the parasite can’t tell they are infected.
Cause: Sexually Transmitted – vaginal, anal, oral.
Symptoms: About 70% of infected people do not have any signs or symptoms. Symptoms can be a mild irritation or very severe.
Some symptoms within 5 – 28 days after being infected, but others don’t appear until much later. People without symptoms can still pass on the infection. Symptoms can come and go.
Girls may notice itching, burning, redness or soreness of the genitals, discomfort with urination, white, yellow-clear, greenish discharge with an unusual smell.
Test: Healthcare provider examination and a laboratory test.
Curable: Yes
Prevention: Condoms correctly used every time you have sex, but condoms don’t cover everything, and it is possible to get or spread this infection, even when using a condom.
Can lead to: More chance of delivering prematurely or to give birth to a low birth-weight baby, and genital inflammation that makes it easier to get infected with the HIV virus, or to pass the HIV virus on to a sexual partner.
Treatment: Drug taken orally or applied as a gel – both/all sexual partners.
Name: Yeast Infection – Genital /Vulvovaginal Candidiasis (VVC)
Type: Fungus
Description: As overgrowth of the normal yeast in the vagina.
Cause: Most infections are caused by the person’s own Candida organisms that live in the mouth, gastrointestinal tract, and vagina without usually causing symptoms. When an imbalance occurs (such as normal acidity of the vagina changes /hormonal balance changes, Candida can multiply and build-up.
Can be passed from person to person through unprotected sex.
Other causes can be:
- Pregnancy
- Diabetes
- Antibiotics
- Corticosteroid medications
- Overweight
Symptoms: Girls usually experience genital itching, burning and sometimes a ‘cottage cheese-like’ vaginal discharge.
Boys may experience an itchy rash on the penis.
The symptoms are like those of many other genital infections. Check with your healthcare provider if you have any of these symptoms.

Curable: Yes
Prevention: Condoms correctly used every time you have sex. Wearing cotton underwear may help reduce the risk. If you have many infections, your healthcare provider can prescribe other medication.
Treatment: Cream and/or pill for both /all partners. Keep genital area dry and clean.
Name: Bacterial Vaginosis (BV)
Type: Bacterial
Description: When the normal balance of bacteria in the vagina is disrupted and replaced by an overgrowth of certain bacteria.
Cause:
- Imbalance of normal vaginal bacteria
- New sex partner /multiple sex partners
- Using an intrauterine device (IUD) for contraception
Symptoms:
- Some girls have no symptoms
- Girls who have never had sex may have BV
- It is common in pregnancy
- Discharge, odour, pain, itching or burning

Prevention: BV isn’t completely understood by scientists and the best ways to prevent it are unknown. However, it is known that BV is associated with having a new sex partner or having multiple sex partners.
The following basic prevention steps can help reduce the risk of upsetting the natural balance of bacteria in the vagina:
- Be abstinent
- Limit number of sex partners
- Do not douche
Treatment: BV is treatable with antibiotics prescribed by a healthcare provider. Use all the medicine prescribed even if the signs and symptoms disappear.
Curable: Yes
Can lead to:
- easier transmission of other STIs including HIV, Herpes, Gonorrhoea
- PID (Pelvic Inflammatory Disease) following hysterectomy or abortion
- more chance of pregnancy complications and low birth-weight baby
- damage to fallopian tubes, increasing risk of infertility or ectopic pregnancy (a life-threating condition where a fertilised egg grows outside the uterus)
Name: Chlamydia
Type: Bacterial
Description: Chlamydia is a common STI caused by the bacterium Chlamydia Trachomatis, which can damage a girl’s reproductive organs.
Cause: Vaginal, anal or oral sex.

Symptoms: Usually mild or absent but if symptoms occur – it’s 1 to 3 weeks after exposure.
Girls:
- Discharge
- Burning during urination
- Lower abdominal pain
- Low back pain
- Nausea and fever
- Pain during intercourse
- Bleeding between menstrual periods
- Chlamydial infection of the cervix can spread to rectum
Boys
- Discharge from the penis
- Pain during urination
Prevention: Male condoms, used consistently and correctly, can reduce the risk of transmission of Chlamydia.
Treatment and testing: Antibiotics. Both boys and girls should be re-tested about three months after treatment for the initial infection, even if they believe that their sex partners were treated. Testing by means of urine or swab.
Curable: Yes
Can lead to:
- Serious and permanent health problems
- Pelvic Inflammatory Disease in Girls (PID)
- Complications can cause irreversible damage, including infertility which can occur ‘silently’ before a girl recognises a problem
- Early infant pneumonia and conjunctivitis (pink eye) in new-borns is common
Name: Gonorrhoea
Type: Bacterial
Description: Gonorrhoea is caused by Neisseria Gonorrhoeae, a bacterium that can grow and multiply easily in the warm, moist areas of the reproductive tract, including the cervix, uterus, and fallopian tubes in girls, and in the urethra (urine canal) in girls and boys. Can also grow in the mouth, throat, eyes and anus.
Cause: Vaginal, anal or oral sex
Symptoms:
In both sexes:
- There may be no symptoms, or they may be very mild
- Thick yellow discharge from penis/vagina, pain urinating and/or during sex
- Anal itching
- Soreness
- Painful bowel movement
- Sore throat
In girls:
- Bleeding between periods
In boys:
- Swollen or painful testicles
Prevention:
- Abstinence
- Condoms used consistently and correctly can reduce the risk of transmission

Testing and Treatment: A urine test can be used to test unless person has had anal/oral sex, in which case swabs are taken.
Curable: Yes, but treatment will not repair damage already done.
Can lead to:
- Serious complications that cause irreversible damage including infertility that can occur ‘silently’ before problem is recognised.
- Increased risk of ectopic pregnancy.
- Infecting baby if pregnant.
- Early infant pneumonia and conjunctivitis (pink eye) in new-borns is common.
- Can spread into the uterus or fallopian tubes and cause Pelvic Inflammatory Disease (PID).
- Can spread to blood and joints if untreated – this can be life-threatening.
- Increased risk of acquiring or transmitting HIV.
- In boys – a painful condition called Epididymitis in the tubes attached to the testicles. May cause sterility (not being able to father children).
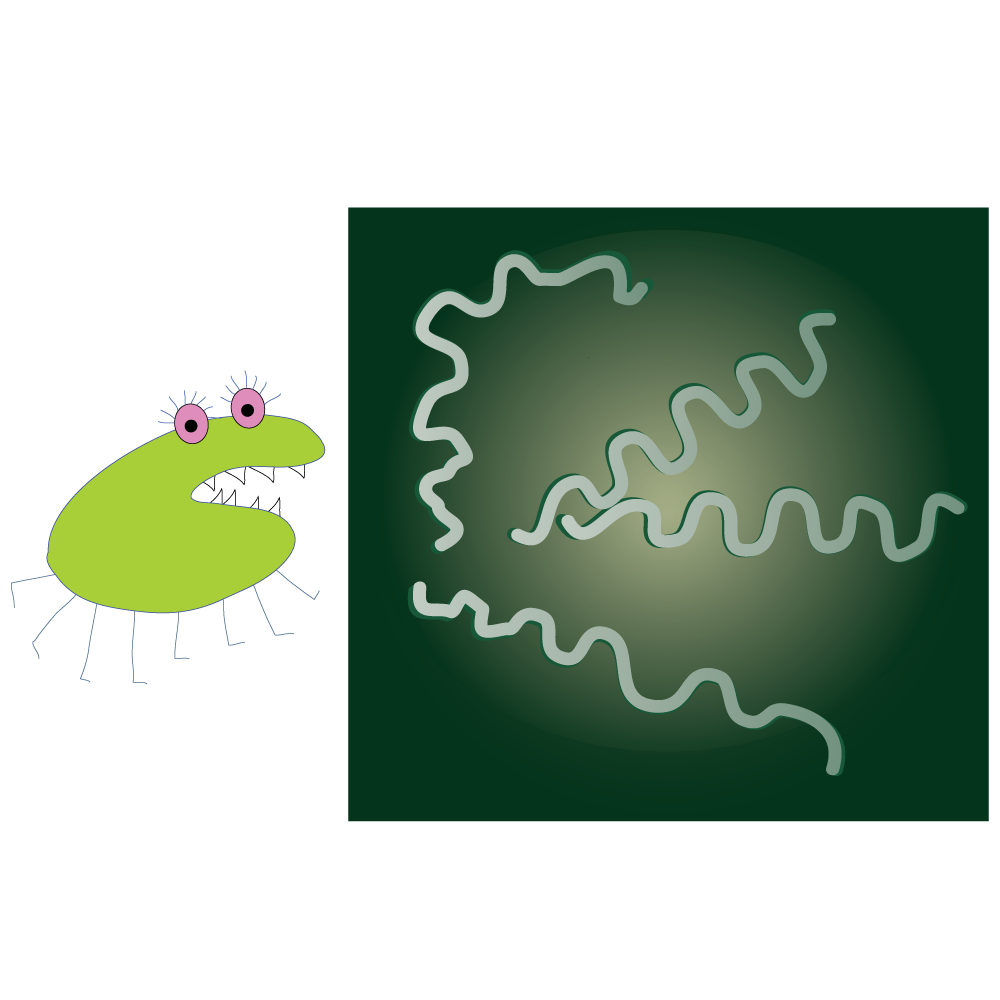
Name: Syphilis
Type: Bacterial
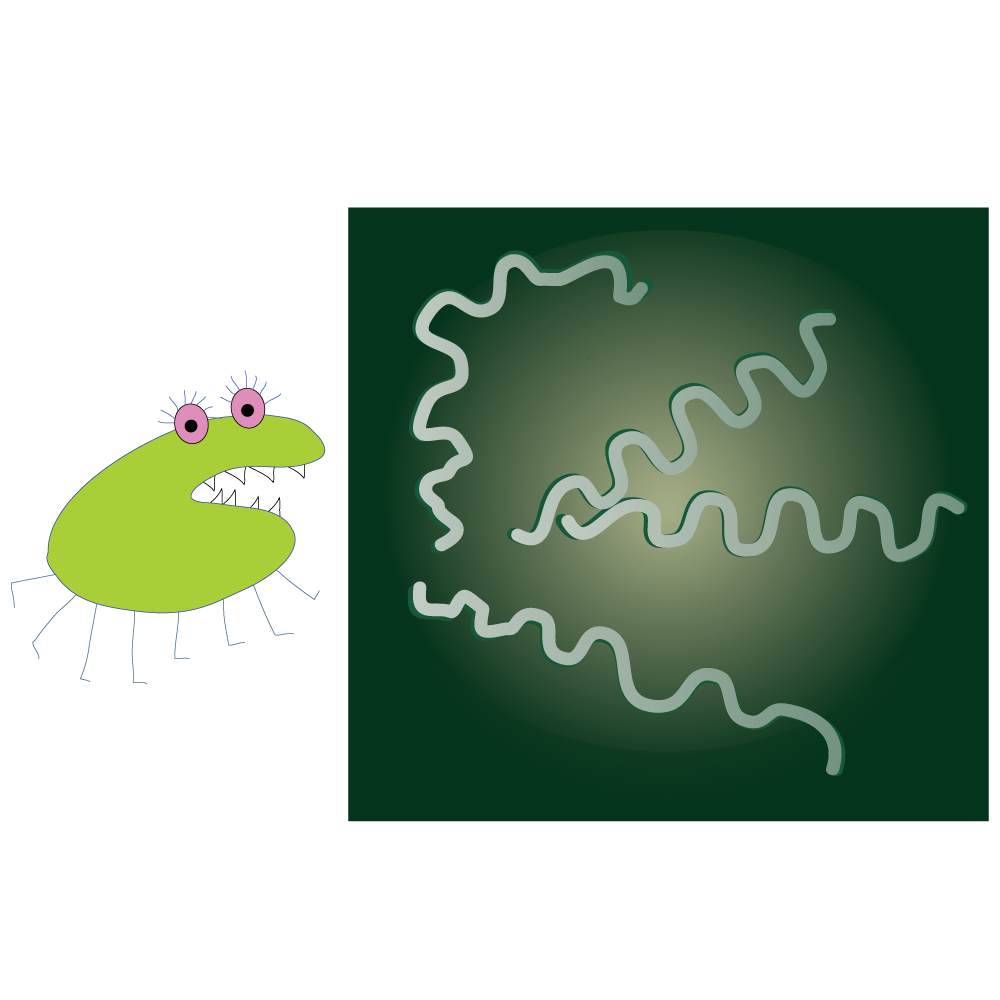
Description: Syphilis is a bacterial STI and can cause long-term complications and/or death if not adequately treated.
Cause: Vaginal, anal or oral sex by direct contact with syphilis sores. Pregnant girls can pass it to their unborn children.
Symptoms: Sores (usually firm, round and painless) occur mainly on the external genitals, vagina, anus, in the rectum, on the lips and in the mouth. The average time between infection with syphilis and appearance of the first symptom is 21 days but can range from 10 to 90 days.
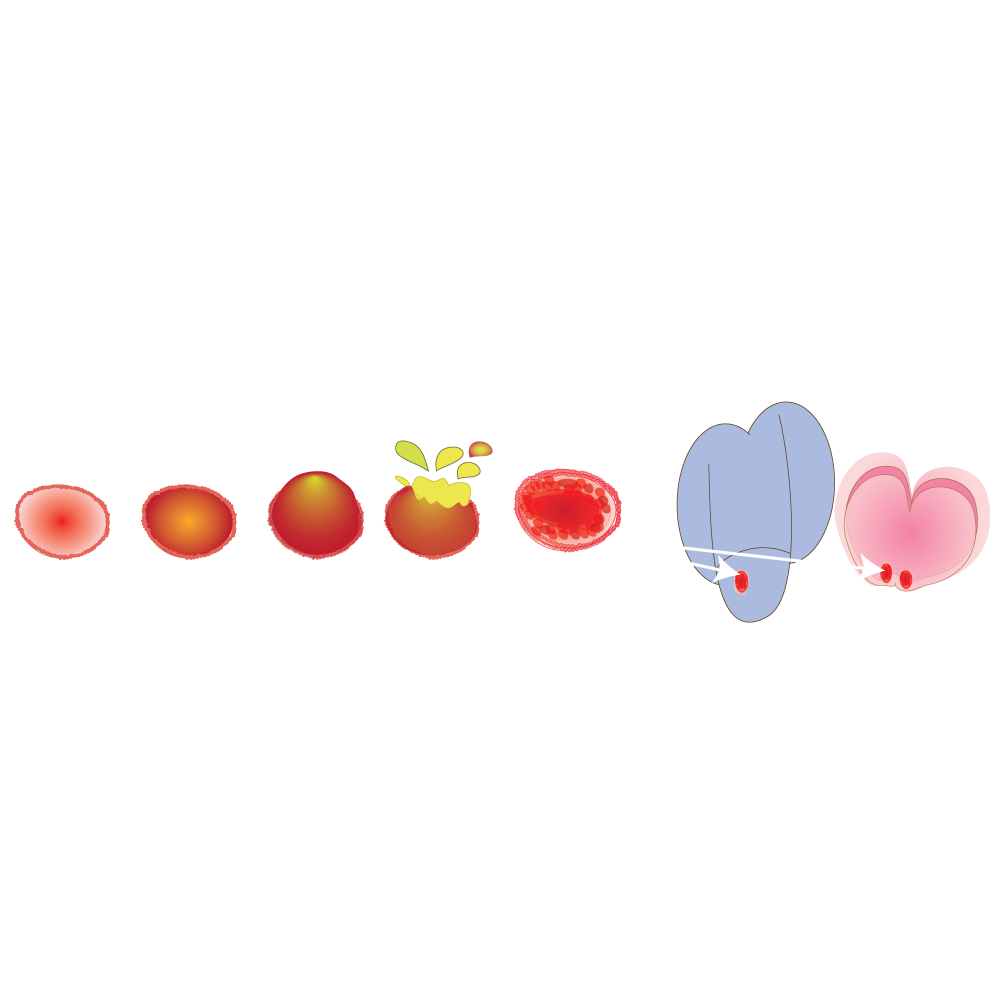
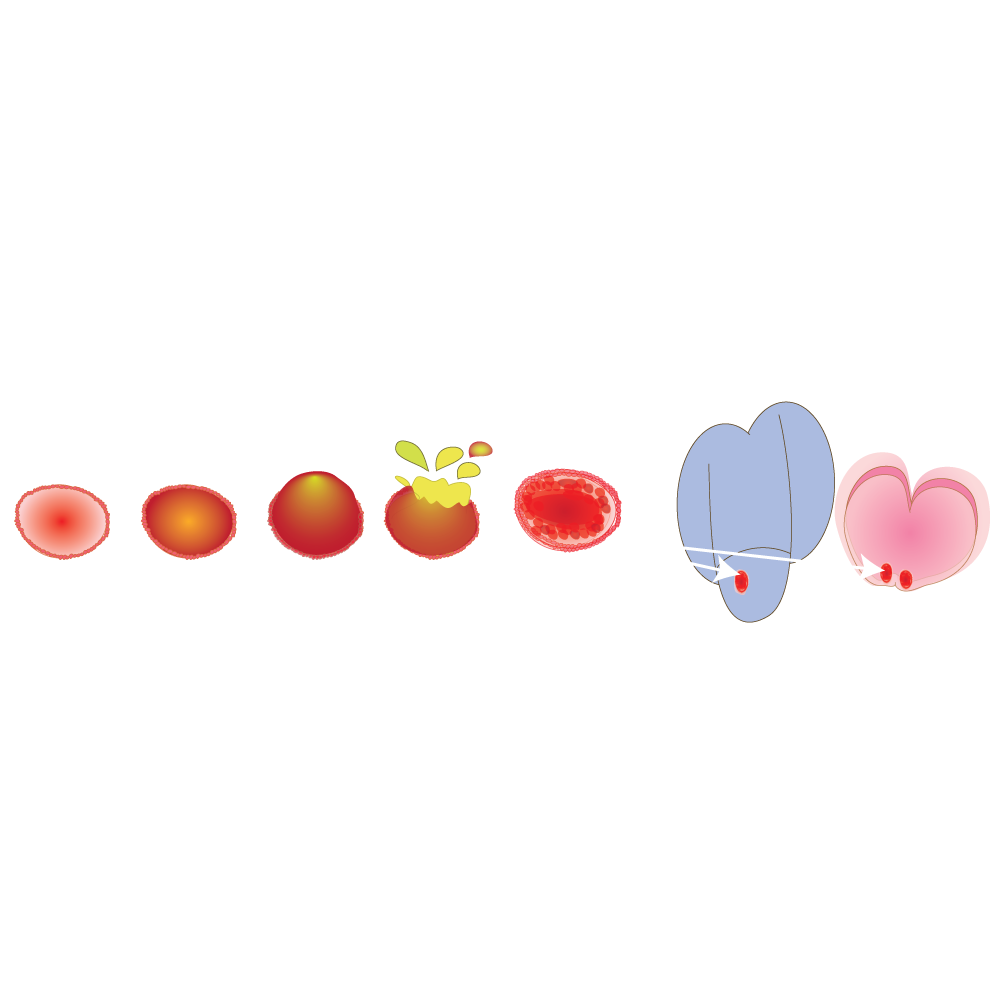
There are 4 stages of Syphilis:
- Primary Stage: the first sore/s appear where syphilis entered the body. The sore is painless so it can easily go unnoticed. It lasts 3 to 6 weeks and heals with or without treatment. A pregnant girl with syphilis can have many health problems, can have low birth weight, be born prematurely (too early) or even be born dead (stillborn).
- Secondary Stage: skin rashes in one or more parts of the body and/or sores in the mouth, vagina or anus. The rash is not itchy and may not even be noticed. Large, raised, grey or white lesions may develop in the mouth, underarm or groin region.
Other symptoms include:
- Fever
- Swollen lymph glands
- Sore throat
- Patchy hair loss
- Headaches
- Weight lass
- Muscle aches
- Fatigue
- Condylomas (wart-like lesions)
Symptoms will go away with or without treatment. Untreated, the infection will progress to the latent and possibly late stages of the disease.
Latent (hidden) Stage: The primary and secondary symptoms disappear. Without treatment there are no signs or symptoms, but Syphilis remains in the body. This latent stage can last for years.
Late Stage: Symptoms can appear 10 – 30 years after infection and include:
- Difficulty coordinating muscle movements
- Paralysis
- Numbness
- Gradual blindness
- Dementia
- The disease damages the internal organs including the brain, nerves, eyes, heart, blood vessels, liver, bones and joints. This damage can result in death.
Prevention: The only 100% safe prevention method is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a trusted partner who has been tested and is known to be uninfected. Condoms do not always protect - contact with a sore outside the condom-covered area can still cause infection.
Oral, anal, vaginal or penile syphilis sores make it easier to transmit and acquire HIV infection. You are 2 to 5 times more likely to get HIV if exposed when syphilis sores are present.
Remember: sores can also be hidden in the vagina, anus, under the foreskin or mouth.
Testing: Usually a blood test.
Every pregnant girl should be tested for syphilis during pregnancy and at delivery, because untreated syphilis can infect and kill her developing baby.
Treatment: Syphilis is usually easy to cure with antibiotics. Treatment will kill the syphilis and prevent further damage, but it will not repair damage already done.
Can lead to: See the stages of syphilis.
Name: Lymphogranuloma (LGV)
Type: Bacterial
Description: LGV is an infection caused by a variety of the bacterium Chlamydia Trachomatis (not the same as chlamydia)
Cause: Direct sexual contact with the genitals, rectum or mouth. More common in MSM (men who have sex with men).
Symptoms: Can begin a few days to a month after encountering the bacteria.
Symptoms can include:
- Pimples/blisters on male genitals /female genital tract that heal quickly without leaving a scar.
- Blood or pus from the rectum (blood in stools).
- Painful bowel movements.
- Small painless sore.
- Swelling and redness of the skin in the groin area.
- Swelling of the labia.
- Swollen groin nodes around the rectum in people who have anal intercourse.
- Diarrhoea and lower abdominal pain.
Prevention: Avoid direct contact with genitals, rectum or mouth of infected person. Remember, there may be no visible symptoms.
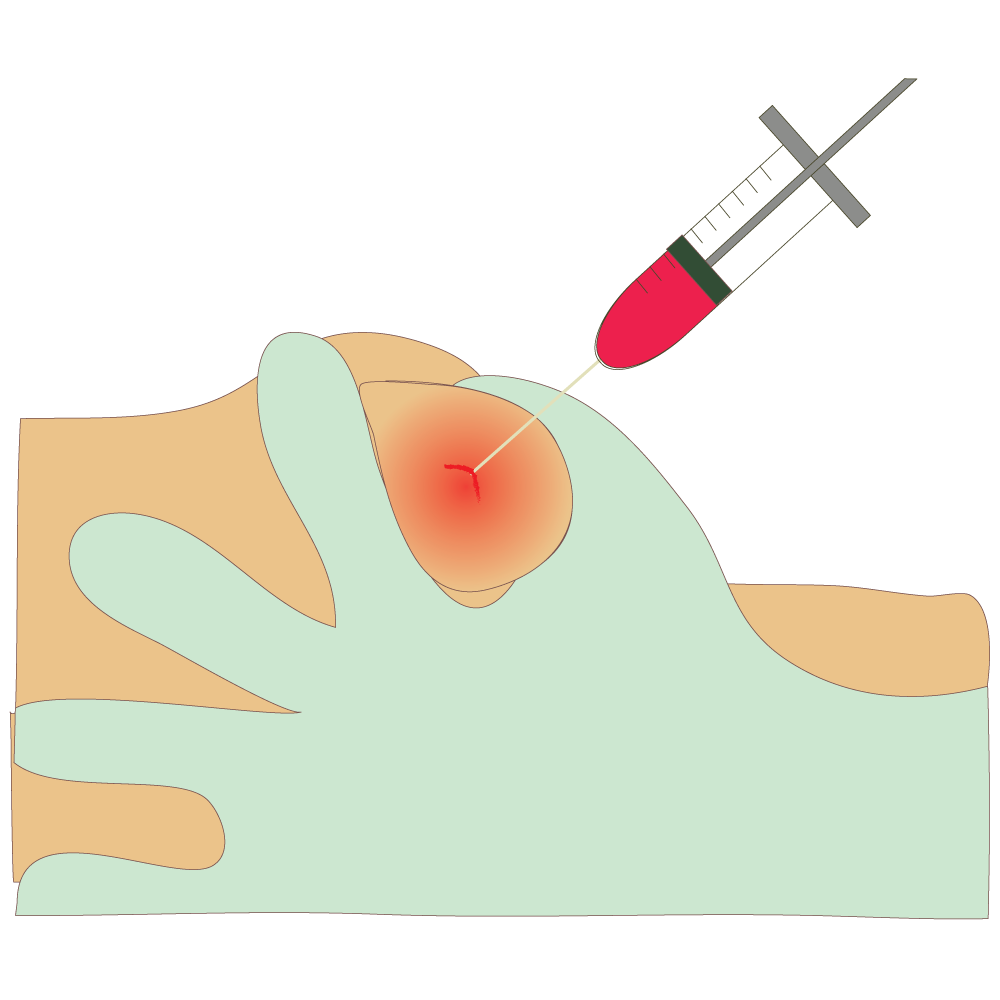
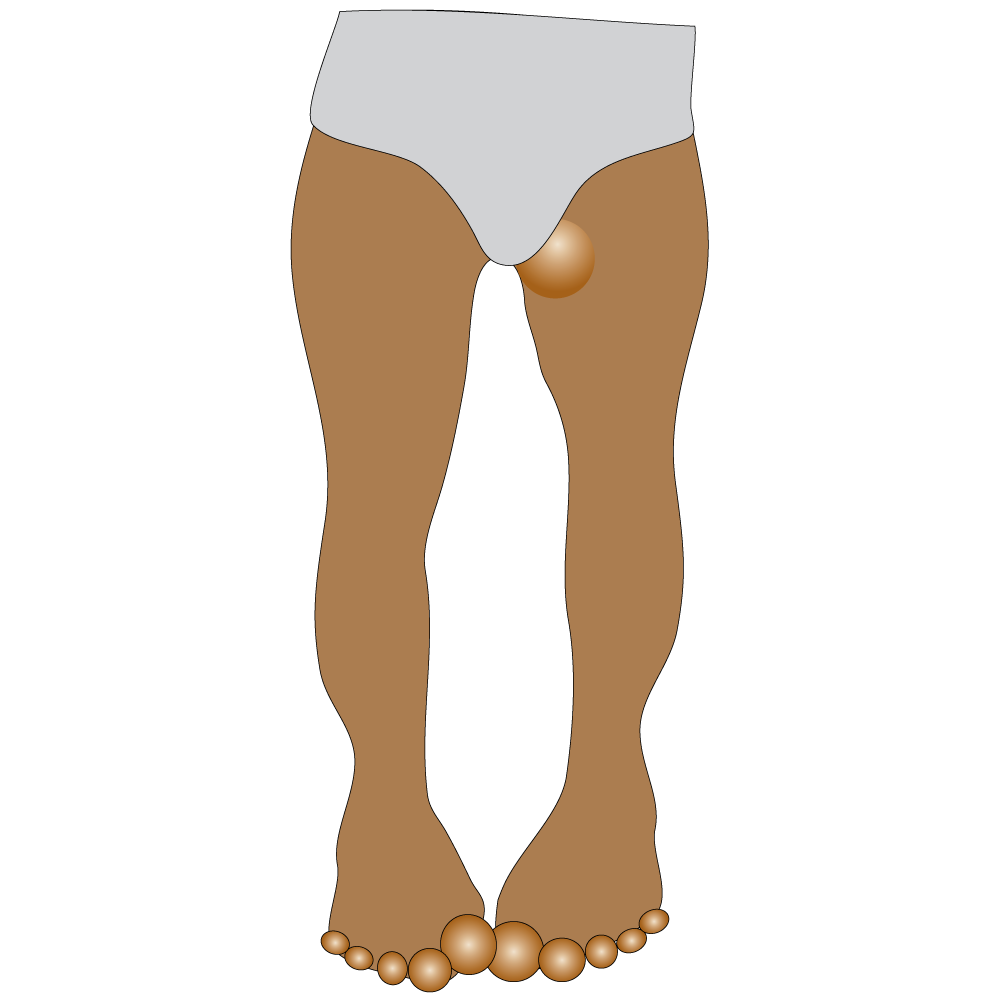
Treatment: Curable with antibiotics. Drainage of the buboes/abscesses by needle aspiration or incision.
If untreated can lead to:
- New-borns can contract the disease from infected mothers during birth.
- Abnormal connections between the rectum and vagina.
- Brain inflammation (very rare).
- Infections in the joints, eyes, heart or liver.
- Long-term inflammation and swelling of the genitals.
- Scarring and narrowing of the rectum.
- Complications can occur many years after you are first infected.
Name: Chancroid
Type: Bacterial
Description: Chancroid is an STI caused by bacterium. It is common in tropical countries but rare in other parts of the world.
Cause: Sexual contact with an infected person. More likely if personal hygiene is not practiced, and if male is not circumcised.
Symptoms: Usually one or more sores or raised bumps surrounded by red border on/in genitals, 4 to 7 days after exposure.
Sores soon become filled with pus and burst, leaving a painful open sore. In about 50% of cases the glands of the groin get bigger, hard, and painful, becoming tender, swelling lumps that can eventually burst.
Prevention: The only 100% safe prevention method is to abstain from sexual contact, or to be in a mutually monogamous relationship with a trusted partner who has been tested and is known to be uninfected.
Condoms do not always protect. Contact with a sore outside condom-covered area can still cause an infection.
If you think you are infected, avoid any sexual contact and get screened. Notify all sexual partners to get screened.
Treatment: Antibiotics will cure Chancroid (lesions and ulcers heal within two weeks).
Can lead to: If untreated can cause ulcers on the genitals that can remain for weeks or months. Risk factor for contracting HIV.
Name: Hepatitis B
Type: Viral
Description: Hepatitis B is an infectious illness of the liver caused by the Hepatitis B virus. Can also be transmitted by non-sexual contact.
Cause:
- Direct contact with hepatitis-infected body fluids (sexual fluids, blood, saliva).
- Through wound or mucous area (eye).
- Sexual contact.
- Injecting drug-use and sharing needles.
- Mother-to-child during childbirth.
- Sharing razors or toothbrushes with infected person.
Symptoms: Symptoms may go unnoticed.
When present, signs and symptoms can include:
- fever
- fatigue
- loss of appetite
- nausea
- vomiting
- abdominal pain
- dark urine
- clay-coloured bowel movements
- joint pain
- jaundice – yellow coloured skin and eye-white.
Prevention: Avoid contact with body fluids (blood, sexual fluids, saliva) of infected person.
Virus can survive outside the body for more than 7 days and still cause infection.
Treatment: For acute infection, no medication is available, treatment is supportive. For chronic infection, antiviral drugs. Persons with chronic HBV infection require medical evaluation and regular monitoring.
Can lead to:
- Chronic hepatitis.
- Cirrhosis (scarring) of the liver or liver cancer.
Name: Human Papillomavirus (HPV)
Type: Virus
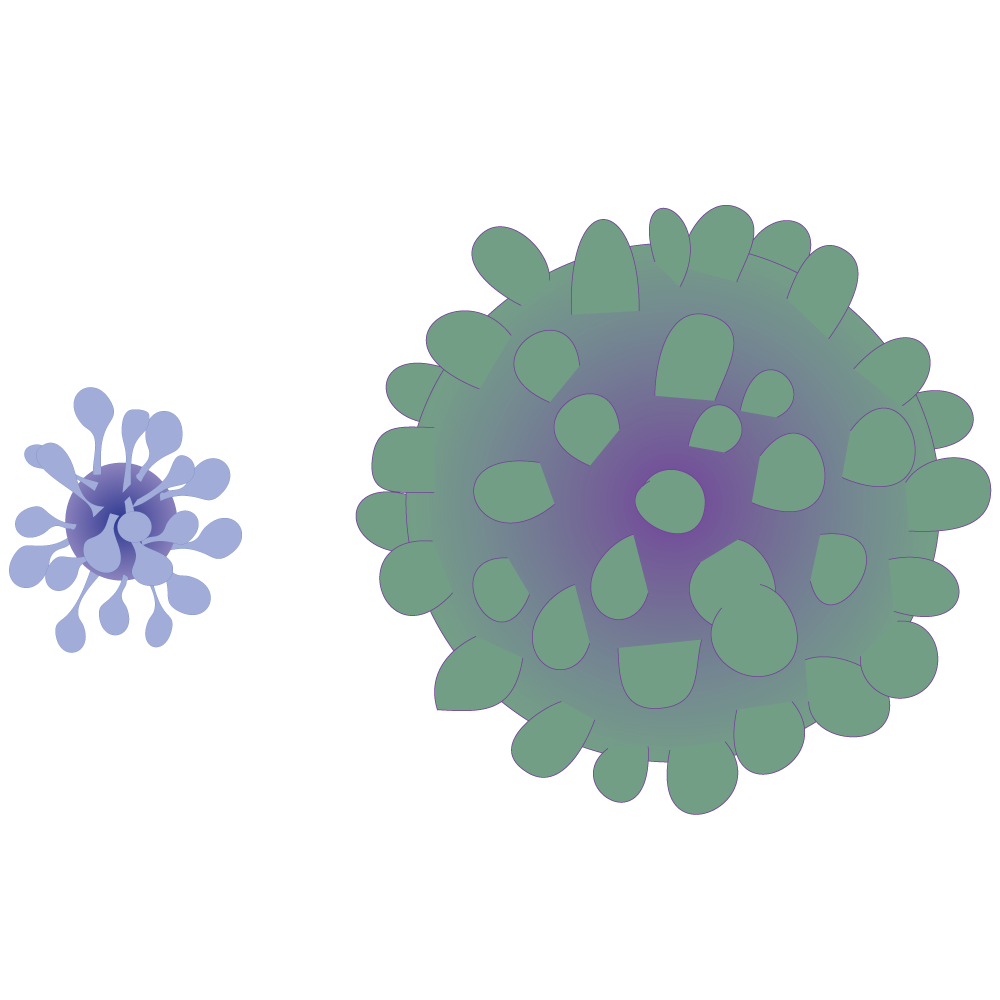
Description: HPV is a very common viral STI, of which there are more than 40 types that can infect the mouth/throat and genital areas of males and females.
Cause:
- Vaginal, anal and oral sex.
- HPV can occur years after contact.
- You can get more than one type of HPV.
- Infants can be infected during delivery.
Symptoms: Most people with HPV do not develop symptoms or health problems but they can still transmit the virus without symptoms.
The immune system usually clears HPV within two years. If not, genital warts occur as a small bump or group of bumps in the genital area. They can be small or large, raised, or flat, or shaped like a cauliflower.
Prevention:
- The only sure way to prevent HPV is to avoid all sexual activity.
- Condoms may not offer full protection as HPV can infect areas not covered.
- Vaccines can protect males and females against some of the most common types of HPV that can lead to disease or cancer. It is important to get three doses to get the best protection.
- Regular screening for cervical cancer to find early signs of disease and treatment to prevent cancer occurring. Other HPV-related cancers might not have signs or symptoms until they are advanced and hard to treat.
Treatment: Visible genital warts can be self-removed with prescribed medications or treated by a healthcare provider.
Can lead to: HPV can cause normal cells to turn abnormal in the form of genital warts or cancer. These include cancers of the cervix, vulva, vagina, penis, anus and throat.
If left untreated, genital warts might go away, remain unchanged or increase in size or number.
Name: Genital Herpes
Type: Virus
Description: Genital Herpes is an STI caused by the herpes simplex viruses. It is not curable but is treatable.
Cause: Vaginal, anal and oral sex
Symptoms: May be so mild as not to be noticed but they usually appear as one or more blisters on or around the genitals, rectum or mouth. The blisters break and leave painful sores that can take 2 to 4 weeks to heal. The first time someone has an ‘outbreak’ they may also experience flu-like symptoms such as fever, body aches and swollen glands. Repeat outbreaks of genital herpes are common.
Prevention: Correct and consistent use of latex condoms can reduce the risk of genital herpes, but outbreaks can occur in areas not covered by a condom. If sores are present, abstain from sexual activity. Even if a person does not have any symptoms, sex partners can still be infected.
Treatment: There is no cure for herpes. Antiviral medications can prevent or shorten outbreaks during the period the person takes the medication.
Can lead to:
- Increased risk of HIV transmission if either partner is HIV-infected.
- Miscarriage or premature birth.
- Infection being passed from mother to child resulting in a potentially fatal infection (neonatal herpes).
- It is dangerous for the baby to contract herpes during pregnancy.
Name: Human Immunodeficiency Virus
Type: Virus
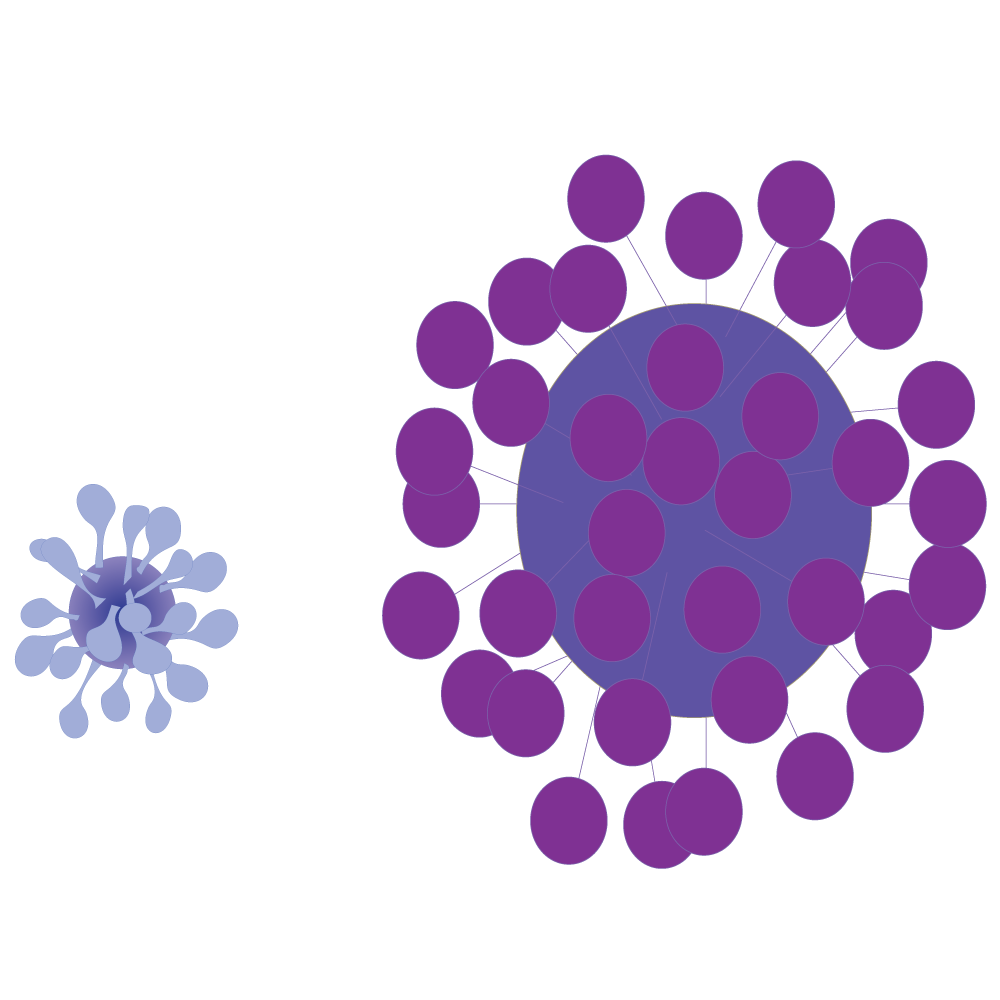
Description: HIV is the Human Immunodeficiency Virus. It is the virus that can lead to Acquired Immune Deficiency Syndrome (AIDS).
Cause: Through having unprotected sex (without a condom) with an HIV-positive person. The virus finds its way into the body more easily if there are sores (broken skin) from STIs.

Through contact with HIV-infected blood, for example:
- sharing contaminated needles
- razor blades
- tattoo needles
- scarification instrument
- unsafe blood transfusions

Through mother-to-child transmission. An HIV-infected pregnant girl can pass HIV onto her baby whilst pregnant, during birth or through breast-feeding.
Symptoms: Within a few weeks of being infected, some people develop flu-like symptoms but others have no symptoms at all.
People living with HIV may appear and feel healthy for several years. Without treatment, and as the immune system weakens, many different types of illnesses start to develop.
Prevention:
- Avoid contact with blood/sexual fluids of an infected person.
- Correct and consistent use of condoms can reduce the risk of transmission.
- Male circumcision reduces the risk of transmission from women to men during vaginal sex.
- Prevention of mother-to-child transmission if you are pregnant.
Treatment: Anti-retroviral treatment can prolong an HIV-infected person’s life to near normal lifespan if taken correctly. For ARVs to control HIV and stop it from replicating (making more of itself), you have to take at least 19 out of 20 doses. This is called adherence.
Can lead to: Without treatment, HIV can lead to AIDS, the late stage of HIV infection, when the immune system is severely damaged and has difficulty fighting diseases and certain cancers. Today, people can live an almost normal lifespan with HIV if they take ARVs correctly.
Name: Molluscum Contagiosum (MC)
Type: Viral
Description: Molluscum Contagiosum is caused by a virus that is a member of the poxvirus family. You can get the infection in several different ways.
Cause: Sexual Contact
Contact with contaminated objects, such as towels, clothing or toys.
Symptoms:
Small, painless papule/s that may become raised, often with a cheesy white dimple in the centre.
Scratching causes them to spread in a line or in groups, called crops, which causes redness (inflammation) of the skin.
Commonly seen on the genitals, abdomen and inner thigh.
Early lesions (papules) on the genitals may be mistaken for herpes or warts but, unlike herpes, these are painless. MC is common in children who become infected from direct contact with a papule.
Prevention:
- Avoid direct contact with the skin lesions.
- Do not share towels, bedding or clothes with other people.
- Avoiding sex can prevent molluscum virus. Even while using a condom, infection can still occur from contact in areas that are not covered by the condom.

Treatment: The infection will usually go away on its own after a few months (or in some cases a year or two) but in the case of weakened immune system, it can worsen.
There are medications the healthcare worker can provide for the papules, or they can be removed surgically, but may result in scarring.
Can lead to: Spreading and recurring of the lesions/papules and other skin infections.
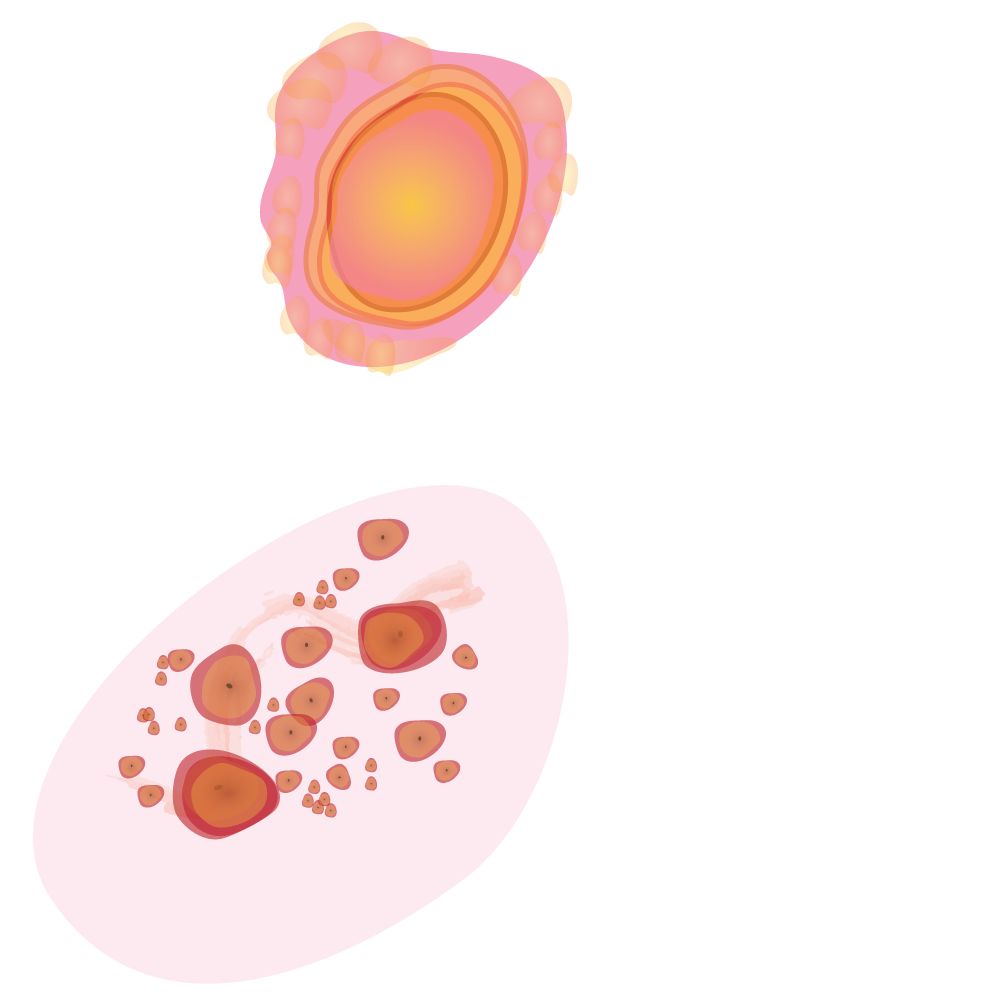
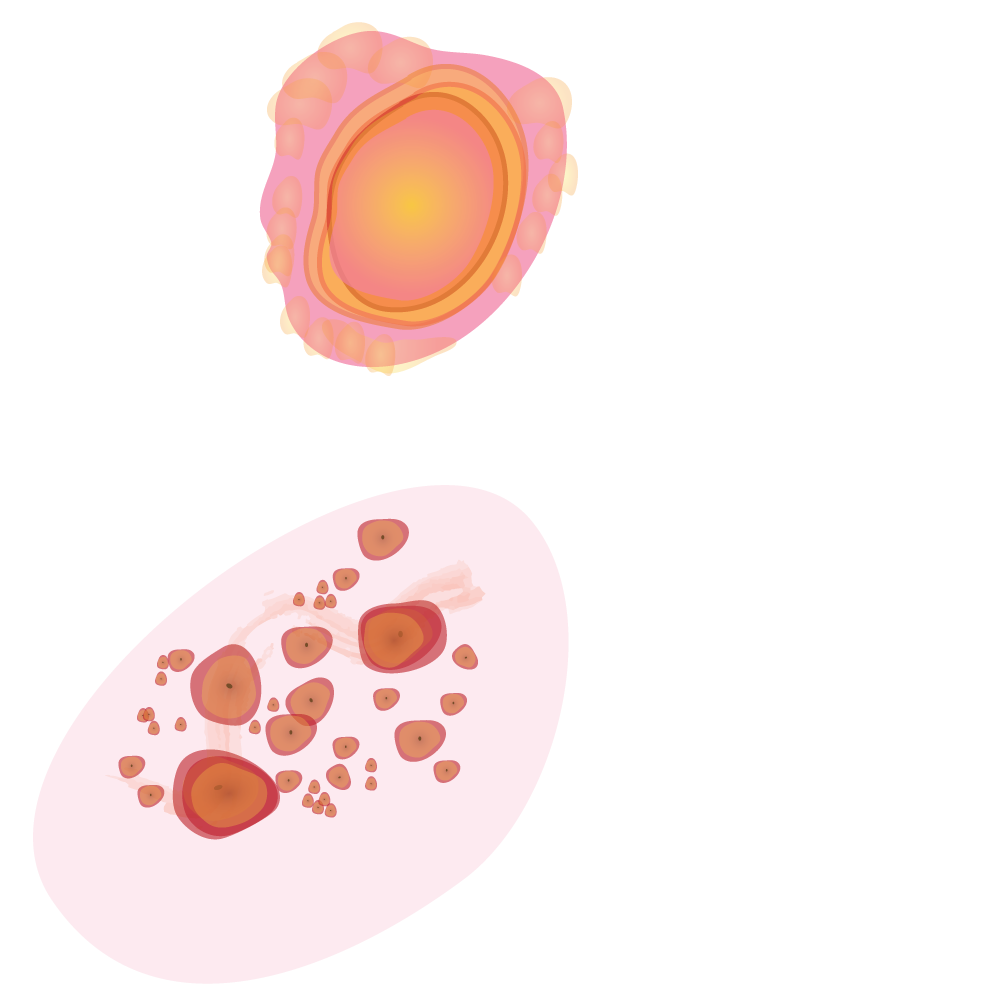
Name: Pelvic Inflammatory Disease (PID)
Type: Complication of other STIs
Description: PID is a serious complication of certain sexually transmitted infections (STIs). PID can damage the fallopian tubes and tissues in and near the uterus and ovaries. PID can lead to serious consequences, including infertility (not being able to have children), ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside of the womb) and abscess formation.
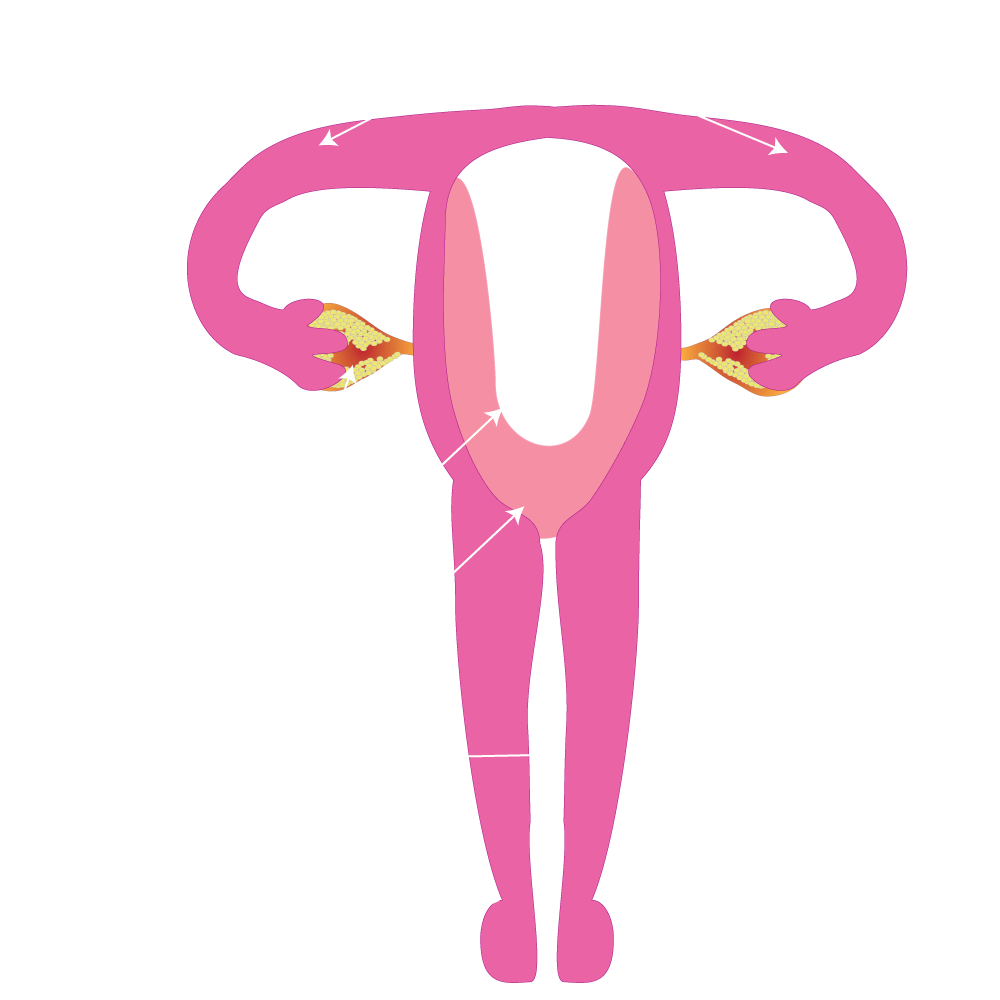
Cause:
- Untreated STIs moving upwards into the reproductive organs.
- Untreated STIs, especially chlamydia and gonorrhoea.
- PID occurs when bacteria (germs) move upward from a girl’s vagina or cervix (opening to the uterus) into her reproductive organs.
- Younger girls have more chance of PID because the cervix of teenage girls is not fully matured, increasing their chances of being infected with the STIs that are linked to PID.
- The more sex partners a girl has, the greater her risk of developing PID because of the potential for more exposure to infectious agents.
- Girls who douche (French for ''soak'' which is a method to wash inside the vagina) may have a higher risk of developing PID.
Prevention:
- Safer sexual practice.
- Screening and treatment for STIs.
- Avoid douching.
Symptoms:
- Symptoms of PID vary from mild to severe.
- Chlamydia-caused PID may result in very mild symptoms, even when serious damage is being done to the fallopian tubes and reproductive organs.
- PID is often unrecognised by girls and their healthcare providers.
- Most common symptom is lower abdominal pain.
- Other signs and symptoms include fever, unusual vaginal discharge that may have a bad smell, painful intercourse, painful urination, irregular menstrual bleeding, and pain in the right upper abdomen (rare).
Treatment: PID can be cured with several types of antibiotics, but these do not reverse any damage that has already occurred.
STIS
Izifo ezithathelwana ngocansi yizifo ezisatshalaliswa ngokuthintana ngocansi. Iningi lazo zisatshalaliswa ngocansi olungavikelekile olwenziwa ngocansi olungena esithweni sangasese, kodwa olunye lungasatshalaliswa ngocansi lomlomo nalapho ababili beshayisana indlwabu.

Zazivamise ukubizwa ngokuthi izifo zocansi noma izifo ezithathelwana ngocansi (venereal diseases/STDs).
Ezinye izifo ezithathelwana ngocansi (STIs) ezifana nehephisi, thrush, izintwala kanye ne-chlamydia zingasatshalaliswa ngocansi lomlomo nalapho ababili beshayisana indlwabu.

Iningi lezifo ezithathelwana ngocansi zingelapheka uma welashwa kusenesikhathi.

Abahlanganyela ngokocansi (bobabili/bonke} badinga ukwelashwa kungenjalo bazophinde batheleleke ngegciwane ngesikhathi beya ocansini olungavikelekile (izifo ezithathelwana ngocansi zizophinda zibuye).
Qikelela ukuthi othandana naye uthola ukwelashwa.

Izifo ezithathelwana ngocansi zisatshalaliswa zisuka kumuntu ziye kumuntu ngezindlela eziningi ezibangelwa ukuziphatha komuntu ngokocansi.

Izifo eziningi ezithathelwana ngocansi zisatshalaliswa uketshezi (amathe, umchamo, uketshezi locansi) kanye/noma ukuthintana kwegazi.
Ezinye zezifo ezithathelwana ngocansi njengehephisi, izintwala, i-thrush kanye ne- chlamydia zisatshalaliswa ngokusondelana ngokomzimba.
Ezinye izifo ezithathelwana ngocansi zingasatshalaliswa zisuka kumama ziya enganeni ngesikhathi sokukhulelwa, sokuncelisa noma ngesikhathi sokubeletha.

Izifo ezithathelwana ngocansi zingasatshalaliswa ngezindlela zegazi ezingaphephile ezifana nokwabelana ngezinalithi, ngesikhathi sokuzijova ngezidakamizwa, imikhuba yokuzigcaba izinhlanga noma ukuzidweba amatatoo.


Ukulinyazwa yizinalithi nakho kungaholela ekudluliselweni kwezifo zocansi ezithathelwanayo.
Ucansi olungavikelekile (ezinqeni, esithweni sangasese sowesifazane, kanye nomlomo). Ngokungasebenzisi amakhondomu njalo futhi ungawasebenzisi ngendlela efanele.
Ngokuya ocansini nabantu abaningi.

Ukubolekana ngezingubo zangaphansi nangamathoyizi ocansi.

Ukutheleleka okusuka kumama kuya enganeni.

Izinalithi ezingcolile/ukulinyazwa yizinalithi.
Izifo ezithathelwana ngocansi zivame ukucasha(asymptomatic). Azibonakali.

Yingakho kubalulekile ukuba uhlolwe.
Uma kungenjalo, ngeke wazi ukuthi unegciwane, ngakho-ke ngeke ukuthole ukwelashwa futhi uzodlulisela isifo sakho esithathelwana ngocansi kothandana naye noma nabo.
*Inkomba isho uphawu noma okukhombisa ukubakhona kokuthile, uphawu noma inkomba yokungahambi kahle/ isifo, ikakhulukazi uma kunoshintsho endleleni ejwayelekile yokusebenza, imizwa noma ukubukeka.
Ngesinye isikhathi akukho zinkomba noma izinkomba zithatha isikhathi ukuvela.

Ezinye zezifo ezithathelwana ngocansi (i-Chlamydia kanye nesipatsholo/ Gonorrhoea) kazinazo izinkomba, noma izinkomba ezibikezelayo (ama-STIs angabonakali).
Ukwenza ucansi olungavikelekile nomuntu one-STI engakabi nezinkomba kusho ukuthi ungatheleleka ngaphandle kokubona izimpawu kumuntu.
Lokhu kusho ukuthi ungedlulisela i-STI yakho ngaphandle kokwazi ukuthi wena qobo lwakho unayo. Ngakho-ke ama-STI angabhebhetheka agcine ephenduka izifo ezesabekayo njenge-PID (Ukutheleleka ezithweni zenzalo kwabesifazane) kanye nokungakwazi ukuthola abantwana.
Izilonda ezithweni zangasese.
Ukuqubuka/ukuvuvukala /izigaxa zembilapho.
Ukuphuma koketshezi esithweni sangasese sowesifazane noma epipini
Izinsumpa ngaphezulu, ngaphakathi nasezindaweni ezizungeze ipipi, isitho zangasese sowesifazane nangemuva ezinqeni.
Ukushisa komchamo.
Ubuhlungu emankwahleni (kubafana).
Ubuhlungu ngezansi kwesisu (entombazaneni).
Ukuluma ngenhla kwemomozi noma kwepipi (ikakhulu ebusuku).

Ukuqubuka/izilonda/izigaxa/izinhlungu emzimbeni, ukuvuvukala kwezindlala, nezinga lokushisa eliphezulu, kanye nezinye izimpawu ezihlukahlukene.

Ungaba nezifo zocansi ezithathelwanayo ezingaphezu kwesisodwa ngesikhathi.
Uma ucabanga ukuthi ungase ube ne-STI, thola ukwelashwa ngokushesha. Izifo eziningi zama-STI zelapheka kalula, kepha hhayi zonke.
Kumele uhlolelwe i-STI uma:
- Uya ocansini kepha ungakaze uhlolwe ngaphambilini
- Uke waya ocansini olungavikelekile lomlomo, lwesitho sangasese sowesifazane noma lwasezinqeni, nothandana naye noma ngaphezulu koyedwa
- Uthandana naye eke wenza ucansi olungavikelekile nomuntu othile ngaphandle kwakho
Unezimpawu ezingejwayelekile ezibandakanya:
- Uketshezi olungajwayelekile oluphuma epipini noma esithweni sangasese sowesifazane
- Uzwa ubuhlungu uma uchama
- Izilonda ezingejwayelekile noma amabhamuza esithweni sangasese noma ezinqeni
- Ukulunywa esithweni sangasese
- Ubuhlungu ngesikhathi socansi
Uma uya ocansini noma wena noma othandana naye nike naba nocansi nabanye ngale kwenu, nifanele ukuhlela ukuba niyohlolwa njalo kusukela ezinyangeni eziyi-6 kuya kweziyi-12
Ukuhlolelwa ama-STI kusho ukuthi uhlolwa wonke ama-STI ( Izifo Ezithathelwana Ngocansi) ngasikhathi sinye.
Ukuhlolwa kuvama ukubandakanya:
- Amaswabhu (isampula lokusamafinyila /isicubu /igazi okunanyathiselwa endwangini ekumuncayo exhunywe endukwini ethambile bese kuthunyelwa elebhu ukuyohlolwa)
- Ukuhlolwa kwegazi
Ukuhlolelwa ama-STI kumahhala emitholampilo kahulumeni. Uyodinga ukubhuka emitholampilo eminingi, ngaphandle uma benohlelo lokwamukela nabangabhukanga.
Uma welashelwa ama-STI qinisekisa ukuthi bonke othandana nabo, nabo bayalashwa. Uma kungenjalo, ungase futhi utheleleke uma usuya ocansini nomuntu ongelashwanga.


Qonda amaphuzu alandelayo ngaphambi kokuba uqale ukwelashwa:
- Kungani udinga umuthi
- Ungawuthatha kanjani, nini umuthi kanye/ noma ungawugcoba kuphi futhi kanjani umuthi ogcotshwayo
- Futhi umuthi wakho ungawulondoloza kanjani
- Kungenzekani uma ungawusebenzisi umuthi njengoba uyaliwe
- Ungawusebenzisa isikhathi esingakanani umuthi
Cela isisebenzi sezempilo ukuthi sikuchazele konke ngokucophelela sibhale phansi imiyalelo yokusetshenziswa kwemithi.

Kubalulekile kakhulu ukulandela imiyalo yesisebenzi sezempilo.
- Ungalokothi usebenzise imithi yakho kunoma yiziphi izimpawu zokugula ngaphandle kwalezo ozinqunyelwe.
- Ungalokothi uphuze imithi yomunye umuntu noma unikeze omunye imithi yakho.
- Ungalokothi uphuze umuthi omningi noma omncane ngaphandle uma ululekwa isisebenzi sezempilo.
- Ungalokothi weqise isikali noma unciphise isikali somuthi, ngaphandle kokuba uyalwe isisebenzi sezempilo ukwenzenjalo.
Ngabe iyosebenza kahle imithi yami?
Funda lezi zitatimende ezilandelayo. Ngabe zikhona ezikuthintayo?
- Ngesinye isikhathi ngiyakhohlwa /ngiyadebesela ukulanda imithi emisha.
- Ngesinye isikhathi ngiyakhohlwa ukusebenzisa imithi yami.
- Ngesinye isikhathi ngithatha imithi ngezikhathi okungezona.
- Ngisebenzisa imithi eminingi eyahlukene futhi ngesinye isikhathi kunzima ukuyehlukanisa.
- Ngesinye isikhathi ngiyema ukusebenzisa imithi uma sengizwa sengingcono.
- Ngesinye isikhathi ngiyeqisa noma nginciphise isikali semithi yami ngokuphambene nemiyalelo kadokotela.
- Ngesinye isikhathi ngiyayeka ukusebenzisa imithi ngoba ngicabanga ukuthi ayisebenzi.
- Angiqondi ukuthi kumele ngiyisebenzise nini imithi yami.
- Angisibuzi isisebenzi sezempilo imibuzo ngemithi yami ngenxa yamahloni nokwesaba ukuphoxeka.
Uma kukhona okukuthintayo kwesinye salezi zitatimende, kungenzeka awuyitholi yonke imihlomulo egcwele yokusebenzisa imithi yakho.
Xoxa nesisebenzi sezempilo mayelana nokusebenzisa imithi yakho ngendlela efanele – lokhu kuyokusiza ngemiphumela yokwelashwa kwakho.

Amakhondomu akuvikela kwamaningi ama-STI kodwa hhayi wonke. Indlela okuyiyona ekugcina uvikelele ngokuphelele (100%) kuma-STI yikungayi nhlobo ocansini. Amanye ama-STI awakhombisi zimpawu ezibonakalayo, ngakho ngeke wazi sonke isikhathi uma udinga ukuhlola.
Okuyiyona kuphela indlela eqinisekisiwe yokuvimbela Izifo Ezithathelwana Ngocansi wukugwema ngokuphelele ukuya ocansini, noma ukuba noyedwa esenithandane naye isikhathi eside (nothembeke ngokuphelele omunye komunye) ninobudlelwane obethembekille noseke wahlolwa kwaziwa ukuthi akathelelekile.
Amakhondomu awavikelani sonke isikhathi. Ukuthintana nesilonda endaweni engamboziwe yikhondomu kusangabangela ukutheleleka.
Enye indlela wukuxoxa ngalezi nhlobo zezifo ngaphambi kokuba niye ocansini nomusha enithandana naye, lokhu kuyosiza ukwenza izinqumo ezisekelwe olwazini mayelana nezinga lobungozi enizimisele ukubhekana nalo ngempilo yenu yocansi.

- Zithibeni ningalwenzi ucansi uma kungenzeka
- Hlehlisani ukwenza ucansi nithathe isikhathi senu ngokungenzeka
- Njalo sebenzisani ikhondomu uma ningakwazi ukuluhlehlisa ucansi
- Gwema ukuya ocansini ngenkathi usesikhathini
- Ningasebenzisi izinalithi /izinsingo nokunye ngokushintshisana
- Ningabolekani amathoyizi ocansi noma izingubo zangaphansi
- Hlala uhlolwa ngisho noma ngabe awunazo izimpawu
- Shesha uthole ukwelashelwa noma iyiphi i-STI
- Qiniseka ukuthi umuntu othandana naye noma othandana nabo, nabo bayelashwa.
- Yisebenzise uyiqede imithi yakho.
- Hlolwa njalo.
- Shintsha indlela oziphatha ngayo ngokocansi
- Zijwayeze ucansi oluphephile – sebenzisa amakhondomu ngezikhathi zonke
- Yana kogonywa (kwezinye izikhathi)
- Qonda ngokwelashwa kwakho.
- Uyisebenzisa kanjani futhi nini.

Ukuhlanzeka komuntu siqu – ukwenza isiqiniseko sokuthi umzimba wakho uhlanzekile.
Abantu banemibono eyahlukene mayelana nenhlanzeko yomuntu siqu. Abanye abantu bageza imizimba yabo okungenani njalo ngosuku futhi basebenzisa iziqedaphunga ukunqanda iphunga lamakhwapha. Imizimba inganuka kabi uma ingagezwa njalo.
Kokunye iphunga lomzimba libangelwa:
- Amakhemikhali akhiqizwa umzimba (njengama-pheromones noma amakhemikhali ocansi akhangayo-noma axosha-abanye)
- Izinto umzimba ozama ukuzisusa ngokuzikhipha lapho uphefumula (njengo galiki notshwala)
- Ukusebenza kwamagciwane esikhumbeni nasezingutsheni. Kuhlala kukhona amagciwane esikhumbeni adla amaseli esikhumba asefile kanye nomjuluko. Amanye amagciwane enza amakhemikhali anuka kabi.
Ukugeza nokusebenzisa iziqedaphunga kungasusa amaningi ala makhemikhali anephunga okwesikhashana, kodwa aphinde akheke nsukuzonke. Yingakho ukugeza njalo kusiza ukulwa nala magciwane nokuqeda iphunga.
Ukugcina isitho sangasese sihlanzekile kuyingxenye ebalulekile kakhulu yenhlanzeko yansuku zonke.

Lona ngu-“ Thalazi (Pthirus)”, intwala eba sesithweni sangasese. Incane kakhulu. Ilingana nechashaza lepensela.

Nguye lo ngaphansi kwesibonasakhulu
UThalazi njengamanje uhlala nomndeni wakhe esithweni sangasese sikaProphet. Bazalela amaqanda amaningi zonke izinsuku.
UProphet uyalunywa kakhulu, ikakhulukazi ebusuku.

UProphet akazi ukuthi uThalazi uzalela amaqanda endaweni yakhe yangasese.

Izintwala ziyalamba ebusuku.

UThalazi uzondla ngegazi ngaphakathi emsukeni wezinza.

Lokhu kungabangela ukuqubuka.

UJane benoProphet bebeya ocansini ezinyangeni eziyisithupha.

Ezimbalwa zezingane zikaThalazi sezisukile kuProphet zayozalela amaqanda esithweni sikaJane sangasese.
La maqanda azochanyuselwa abe yizintwala esikhathini esingangamasonto amabili kuya kwamane.

Ngaleso sikhathi - uRose ufika edolobheni futhi uchitha ubusuku noProphet. Bangabangani kusukela kudala.
URose uya ekhaya esokeni lakhe uPeter (nabanye abagibeli).

UPeter kwesinye isikhathi uya ocansini noSibongile, othengisa ngocansi.

UPeter uchitha impelasonto noZola. Baziqeqesha ngokugijima ndawonye futhi baye ocansini ngenkathi uRose engekho.

Isoka likaZola nguKenny. Uthi ukuba mdadlana (futhi unomkakhe nezingane).
Jzjngane zikaThalazi noThalazi’ ziyazalana zisabalale, zibange ukuluma nomaphi lapho ziyakhona!
Kunezinhlobo ezahlukene zama-STI ezahlukaniswe amaqembu amathathu:
- Amabhakthiriya- lawo abangelwa ngamabhakthiriya (amagciwane)
- Amavayirali - abangwa yivayirasi
- Amafangali nokunye – lawa abangelwa amafangasi noma amapharasaythi noma amaprotozowa
Ihephisi yesitho sangasese, i-HIV kanye ne-HPV zibangelwa yivayirasi.
Ama-STI angaqhamuki kumavayirasi njenge-chlamydia, trichomoniasis, isipatsholo (gonorrhoea), ugcusula (syphilis) kanye ne-chancroid kungelashwa ngempumelelo ngokusebenzisa ama-antibiotics.
Izifo ezivela kuma-STI zingaholela ekutheni umuntu angabatholi abantwana, izinkinga zokukhulelwa kanye nomdlavuza womlomo wesibeletho, kanjalo nasekufeni kwabantwana kanye nabantu abadala.
Amanye amagama ahlukene ama-STI: yi-drop, yi-itch, yisipatsholo (gonorrhoea), yigazi elibi, ugcusula (syphilis), crabs, yi-HIV, yi-morning drip, ihephisi,i-fever kiss, yi- clap, yi-VD, yi-cystitis.
- Izintwala esithweni sangasese (ezisazinkalankala)
- I-Bacterial vaginosis
- I-Chlamydia
- Ihephisi yesitho sangasese
- Isipatsholo (Gonorrhoea).
- I-Hepatitis B and C
- I-HPV - Human papillomavirus infection
- I-Lymphogranuloma Venereum (LGV)
- Utwayi
- I-Chancroid
- I-PID - Pelvic inflammatory disease
- I-Trichomanias
- I-Yeast infections
Kukhona ama-STI anhlobonhlobo, futhi singawehlukanisa ngemikhakha eminingi.
Eziningi Izifo Ezithathelwana Ngocansi ziyokuphatha kuphela uma uya ocansini nomuntu one-STI. Nokho kukhona izifo, njengezilonda (scabies), ezibizwa ngama-STI ngoba zivame ukuthelelwana ngocansi kodwa zinokuthelelwana nangezinye izindlela.
Uzobona ukuthi zingakanani izifo zalolu hlobo ezingenazo izimpawu ezisobala nokuthi zingadlulela kalula kanjani kwabanye – zize kuwe noma zedluliswe nguwe.
Ukutheleleka kungahlukaniswa izigaba ezintathu:
- Amapharasaythi nokunye
- Amabhakthiriya
- Amavayirasi
Indlela okuyiyonayona yokugwema ephephile ngokugcwele (100 %) ukungayi ocansini noma ukuba sebudlelwaneni besikhathi eside nomuntu oyedwa (ukwethembeka ngokugcwele/100%) othandana naye.
Igama: Izintwala eziba sezithweni zangasese (izinkalankala /crabs)
Uhlobo: Amapharasaythi
Incazelo: Izimuncagazi ezincane ezime okwenkalankala eziphuzi ezinamathelayo esikhumbeni zimunce igazi. Ziphila oboyeni obusemzimbeni (ikakhulu obusezithweni zangasese, nobusemakhwapheni, obusebusweni, ngisho nasemashiyeni). Zisebenzisa izinzipho zazo ezifana nezenkalankala ukubambelela ezinweleni.
Imbangela: Zithathelwana ngocansi kepha zingedluliselwa ngokubolekana izingubo, amathawula, nangezingubo zokulala nibolekana nomuntu osenazo.
Izimpawu: Zihlala ezingxenyeni zomzimba ezinoboya. Ngokujwayelekile zibonakala ezinsukwini ezi-5 kuya emasontweni ayisi-7 emva kokuba uthelelekile. Kwesinye isikhathi amaqanda ayabonakala, futhi nezintwala zingabonakala zihamba esikhumbeni. Kuyaluma kakhulu ebusuku. Amabala abomvu alumayo nokuqubuka ezihlakaleni, emaqakaleni, ezandleni, ezithweni zangasese esifubeni nasemhlane.
Ziyelapheka: YeBO
Ukuvimbela: Ayikho indlela esebenzayo yokuvimbela ukungenwa yigciwane ngesikhathi socansi. Umuntu onaleli gciwane elisankalankala anganciphisa ingozi yokuledlulisela kwabanye ngokuba awashe izingubo zakhe zokulala, amathawula, nezingubo azigqokile (ngamanzi ashisa kakhulu) ukubulala lezi muncagazi.
Ukwelapha: Amashampoo akhethekile, nokokugcoba okubulala izintwala namaqanda azo. Akudingekile ukushefa izinwele ezithweni zangasese ngoba lokho ngeke kuziqede izintwala. Ukwelashwa kungase kudinge kuphindwe ukuze kufe onke amaqanda.
Igama: Izilonda (Scabies)
Uhlobo: Amapharasaythi
Ukuluma: Ukulunywa okungamandla, kwesikhumba esithelelekile yizimbuzane ezimunca igazi. Izimbuzane zesifazane esezikhulile azibonakali ngeso lenyama, ezesilisa ngobukhulu ziyingxenye uma uziqhathanisa nezesifazane. Izimbuzane zesifazane zimba isikhumba ngaphandle zizalele kuso amaqanda.
Imbangela: Zidluliseka ngocansi kodwa zingadluliseka futhi ngokuthintana ngqo nesikhumba isikhathi eside. Zingasabalala ngokushesha endaweni enesiminyaminya.
Izimpawu: Ziqala emasontweni ama-2 kuya kwayi-6 emva kokutheleleka. Imigojana ebonakala njengemigqa yamagagasi (± 5mm) ubude. Zivamise ukutholakala phakathi kweminwe nezinzwane, ezithweni zangasese, nasezinqeni, ezindololwaneni nasezihlakaleni.
Ukuqubuka okulumayo kakhulu kwezigaxa ezinjengezinduna – lokhu kuyikuziphendulela kwesikhumba kulezi mbuzane, amaqanda azo, namakaka azo. Ukuluma ikakhulukazi ebusuku, noma emva kokugeza ngenkathi umzimba ufudumele, lokhu kubangelwa yizimbuzane.

Ziyelapheka: Yebo
Ukukugwema: Ayikho indlela ephumelelayo yokugwema ukutheleleka ngaphandle kokugwema ukuthintana ngqo nomuntu othelelekile. Umuntu othelelekile anganqanda ukubhebhetheka kokutheleleka ngokuwasha izingubo azigqokayo nezingubo zokulala ngamanzi ashisa kakhulu ukuze kufe izimbuzane.

Ukwelashwa: Bonke abantu abahlala endlini eyodwa kufanele balashwe ngokusebenzisa okokugcoba okungatholaka ekhemisi noma emtholampilo.
Igama: Trichomoniasis (‘trich’)
Uhlobo: Ipharasaythi
Incazelo: Ejwayelekile kakhulu i-STI ebangelwa yipharasaythi (Trichomonas Vaginalis). Izimpawu zesifo ziyehlukana kodwa abantu abaningi abanepharasaythi kabazi noma bathelelekile.
Imbangela: Ithelelwana ngocansi – ucansi lwesitho sangasese sowesifazane, ucansi lwangemuva ezinqeni, nolomlomo.
Izimpawu: Cishe abangama-70% abantu abathelelekile kabanazo izimpawu noma izinkomba. Izinkomba kungaba yikutheleleka okungatheni noma okukhulu kakhulu.
Ezinye izinkomba zivela ezinsukwini ezi-5 kuya kwezi ngama-28 ngemuva kokutheleleka, kodwa ezinye kaziveli kuze kube yisikhathi eside. Abantu abangenazo izinkomba noma izimpawu basangakwedlulisa ukutheleleka. Izinkomba zingavela zibuye zinyamalale.
Amantombazane angase ezwe ukuluma, ubuhlungu, ukuba bomvana noma izilonjana ezithweni zangasese, ubuhlungu uma echama, uketshezana olumhlophe, oluphuzi, noma oluluhlazana olunuka ngendlela engajwayelekile.
Ukuhlolwa: Ukuhlolwa yisisebenzi sezempilo kanye nokuhlolwa yilabhorethri.
Ukulapheka: Yebo
Ukugwema: Ngokusebenzisa amakhondomu ngendlela eyiyo ngaso sonke isikhathi uma uya ocansini, kepha amakhondomu awasizi kukho konke, futhi kungenzeka ukuba utheleleke usisabalalise lesi sifo, ngisho uwasebenzisa amakhondomu.
Kungaholela kulokhu: Emathubeni amaningi okubeletha ngaphambi kwesikhathi noma okubeletha ingane enesisindo esincane, kanye nokuvuvukala kwesitho sangasese okwenza kube lula ukungenwa yigciwane le-HIV, noma ukudlulisa igciwane le-HIV koya naye ocansini.
Ukwelapha: Umuthi ophuzwayo noma ogcotshwayo nobabili/noma nabobonke oya nabo ocansini.
Igama: Ukutheleleka nge-Yeast – Genital /Vulvovaginal Candidiasis (VVC)
Uhlobo: Ifangasi
Incazelo: Wukwanda kwe-yeast ejwayelekile emgudwini wesitho sangasese sowesifazane
Imbangela: Okuningi ukutheleleka kubangelwa yizinto eziphila kuyi-Candida/Yeast esemlonyeni, emgudwini wamathumbu nesisu kanye nasemgudwini wesitho sowesifazane sangasese ngaphandle kokuveza izimpawu. Uma kushintsha isilinganiso se-esidi ejwayelekile /kushintsha isilinganiso samahomoni, i-Candida/Yeast iyanda ikhule kakhulu.
Ingadluliseka isuka kumuntu iye kumuntu uma kwenziwa ucansi olungavikelekile.
Ezinye izimbangela kungaba yilezi:
- Ukukhulelwa
- Isifo sikashukela
- Ama-Antibiotics
- Imithi ye-Corticosteroid
- Ukukhuluphala ngokweqile
Izimpawu: Amantombazane ajwayele ukulunywa esithweni sangasese, ubuhlungu nokuphuma kwento eshube njengamasi esithweni sangasese.
Abafana bangase babe nokuqubuka okulumayo epipini.
Izimpawu ziyefana njengakwezinye izifo eziningi zesitho sangasese. Buza isisebenzi sezempilo uma unanoma yiluphi lwalezi zimpawu.

Ukwelapheka: YeBO
Ukugwema: Ukusebenzisa amakhondomu ngendlela efanele njalo uma uya ocansini. Ukugqoka izingubo zangaphansi ezenziwe ngokotini kungase kusize ukunciphisa isimo esingaba yingozi. Uma unezifo eziningi, umeluleki wakho wezempilo angakubhalela imithi okumele uyisebenzise.
Ukwelashwa: Okokugcoba kanye/noma iphilisi labo bobabili/bonke othandana nabo. Gcina isitho sangasese somile futhi sihlanzekile.
Igama: I-Bacterial Vaginosis (BV)
Uhlobo: Ibhakthiriya
Incazelo: Uma isilinganiso sebhakthiriya eyejwayelekile emgudwini wesitho sangasese siphazamisekile kwase kwanda kakhulu izinhlobo ezithile zebhakthiriya.
Imbangela:
- Wukuncipha noma ukwanda kwesilinganiso esijwayelekile samabhakthiriya asemgudwini wesitho sangasese.
- Ukuba nomuntu noma abantu abasha osuthandana nabo
- Ukusebenzisa i-IUD esibelethweni ukuvimbela ukukhulelwa
Izimpawu:
- Amanye amantombazane awabi nazo izimpawu
- Amantombazane angakaze aye ocansini angase abe ne-BV
- Ivamile ngesikhathi sokukhulelwa
- Ukuphuma koketshezi esithweni sangasese, iphunga, izinhlungu, nokulunywa

Ukuvimbela: I-BV abayiqondi ngokugcwele ososayensi kanti nezindlela ezingcono zokuyivimbela kazaziwa. Nokho-ke, kuyaziwa ukuthi i-BV ihlotshaniswa nokuba nomuntu omusha othandana naye noma ukuba nabantu abaningi oya nabo ocansini.
Lezi zinyathelo zokuvimbela eziyisisekelo zingasiza ukunciphisa ubungozi bokuphazamisa isilinganiso esijwayelekile sebhakthiriya emgudwini wesitho sangasese:
- Ungayi ocansini
- Nciphisa oya nabo ocansini
- Ungakhaphezeli (douche)
Ukwelashwa: I-BV iyalapheka ngama-antibiotics anikezwa yisisebenzi sezempilo. Sebenzisa yonke imithi oyinikiwe uyiqede ngisho noma ngabe izimpawu noma izinkomba sezinyamalele.

Ukwelapheka: Yebo
Kungaholela kulokhu:
- Ukusabalala kalula kwamanye ama-STI okufaka phakathi i-HIV, iHephisi, nesipatsholo (Gonorrhoea)
- I-PID (Isifo sokutheleleka ezithweni zokuzala) emuva kokukhipha isibeletho (hysterectomy) noma ukuphuphuma kwesisu
- Amathuba amaningi omonakalo ngesikhathi sokukhulelwa kanye nokubeletha ingane enesisindo esincane kakhulu
- Umonakalo emashubhini enzalo (fallopian tubes), ukwanda kobungozi yokungatholakali kwabantwana noma i-ectopic pregnancy (isimo esiyingozi enkulu lapho iqanda elivundisiwe likhulela ngaphandle kwesibeletho)
Igama: I-Chlamydia
Uhlobo: Ibhakthiriya
Incazelo: I-Chlamydia yi-STI ejwayelekile ebangelwa yibhakthiriya i-Chlamydia Trachomatis, engalimaza izitho zokuzala zentombazane.
Imbangela: Wucansi olubandakanya umgudu wesitho sangasese, isitho sangemuva ezinqeni noma ucansi lomlomo.

Izimpawu: Ngokujwayelekile ezingatheni noma zingabikho kodwa uma zikhona izimpawu – zithatha isonto eli-1 kuya kwama-3 ngemuva kokwenza ucansi.
Amantombazane:
- Uketshezana oluphuma emgudwini wesitho sangasese
- Ubuhlungu uma uchama
- Izinhlungu esinyeni
- Izinhlungu ngaphansi nomhlane
- Isicanucanu nemfiva
- Ubuhlungu ngesikhathi socansi
- Ukopha phakathi kwezikhathi zokuya esikhathini
- Ukutheleleka kwe-Chlamydia yomlomo wesibeletho kungasabalala kuze kufike esithweni sangemuva phakathi kwezinqe.
Abafana:
- Uketshezana oluphuma epipini
- Ubuhlungu uma uchama
Ukuvimbela: Amakhondomu abesilisa, esetshenziswa njalo futhi ngendlela efanele, anganciphisa ubungozi bokwedlulisa i-Chlamydia.
Ukwelapha kanye nokuhlolwa: Ama-Antibiotics. Bobabili umfana nentombazane kumele baphinde bahlolwe ezinyangeni ezintathu ngemuva kokwelashelwa ukutheleleka kokuqala, ngisho noma ngabe omunye uyakholwa wukuthi athandana naye welashwa. Kungahlolwa umchamo noma iswabhu.
Ukwelapheka: Yebo
Singaholela kulokhu:
- Izinkinga zempilo ezinkulu nezingasoze zaphela.
- Ukudlebeleka kwesifo kungabangela umonakalo ongeke walungiswa, okufaka phakathi ukungatholi abantwana okungenzeka ‘isinyelela’ ngaphambi kokuba intombazane iyibone inkinga
- Ukuphathwa yi-pneumonia kanye ne-conjunctivitis (pink eye) kubantwana abazelwe kujwayelekile
Igama: Isipatsholo (Gonorrhoea)
Uhlobo: Ibhakthiriya
Incazelo: Isipatsholo (Gonorrhoea) sibangelwa yibhakthiriya i-Neisseria Gonorrhoeae, ekwazi ukukhula futhi yande kalula endaweni efudumele futhi eswakeme njengomgudu wezitho zokuzala, lokhu kuhlanganisa:
- Umlomo wesibeletho, isibeletho, amashubhu okuhamba kuwo amaqanda (fallopian tubed), emantombazaneni
- Umgudu womchamo (urine canal) kubafana namantombazane.
Singakhula futhi emlonyeni, emphinjeni, emehlweni nangemuva phakathi kwezinqe.
Imbangela: Ucansi lomgudu wesitho sangasese, ngemuva phakathi kwezinqe kanye nocansi lomlomo
Izimpawu:
Kubo bobubili ubulili:
- Kungase kungabikho zimpawu, noma kube zimpawu ezingatheni
- Okusaketshezi olushubile oluphuzi oluphuma epipini/emgudwini wesitho sowesifazane sangasese, ubuhlungu uma uchama kanye/noma ngesikhathi socansi
- Ukuluma esithweni sangemuva phakathi kwezinqe
- Izinhlungu
- Ubuhlungu bomgudu wokudla
- Umphimbo obuhlungu
Emantombazaneni:
- Ukopha phakathi kokuya esikhathini
Kubafana:
- Amankwahla abuhlungu noma avuvukele
Ukuvimbela:
- Ukungayi ocansini
- Ukusetshenziswa njalo kwamakhondomu nangendlela efanele kunganciphisa ubungozi bokwedlulisa isifo
Ukuhlolwa kanye Nokwelashwa: Kungahlolwa umchamo ngaphandle kokuba umuntu eye ocansini ngesitho sangemuva phakathi kwezinqe/ocansini lomlomo, lapho-ke kumele kuhlolwe iswabhu.
Ukwelapheka: Yebo, kodwa ukwelapha ngeke kulungise umonakalo osuwenzekile.
Lokhu kungaholela:
- Ukudlebeleka okuyingozi kwesifo okungabangela umonakalo ongalungiseki ofaka phakathi ukungabatholi abantwana okungenzeka ‘isinyelela’ ngaphambi kokuba inkinga ibonakele.
- Ubungozi obukhulu obungenzeka bokukhulelwa ngaphandle kwesibeletho.
- Okhulelwe angathelela ingane.
- Ukuphathwa yi-pneumonia kanye ne-conjunctivitis (pink eye) kubantwana abazelwe kujwayelekile.
- Singasabalala siyofika esibelethweni noma emashubhini okuhamba kuwo amaqanda sibange i-PID (Isifo sokutheleleka kwezitho zenzalo kwabesifazane).
- Singangena egazini nasemalungeni uma singelashwa – lokhu kungaba yingozi enkulu.
- Ubungozi obukhulu bokuthola noma ukusabalalisai-HIV.
- Kubafana – isifo sezinhlungu esibizwa Epididymitis emashubhini athintene namankwahla. Kungabangela ukuphela kwenzalo (ukungakwazi ukuthola abantwana).
Igama: Ugcusula (Syphilis)
Uhlobo: Ibhakthiriya
Incazelo: Ugcusula (Syphilis) yi-STI ebangwa yibhakthiriya engabanga ukudlebeleka kwesifo kanye/noma ukufa uma ungelashwanga ngokwanele.
Imbangela: Ucansi olubandakanya umgudu wesitho sowesifazane sangasese, isitho sangemuva phakathi kwezinqe noma ngocansi lomlomo ngokuthintana ngqo nezilonda zikagcusula. Amantombazane akhulelwe angasedlulisela kubantwana abangakazalwa.
Izimpawu: Izilonda (ngokujwayelekile eziqinile, eziyindilinga futhi ezingebuhlungu) ziba khona ikakhulukazi ngaphandle ezithweni zangasese, emgudwini wesitho sowesifazane sangasese, esithweni esingemuva phakathi kwezinqe, ekugcineni kwethumbu elixhumene nesitho sangemuva (rectum), ezindebeni kanye nasemlonyeni. Isikhathi esilinganiswayo phakathi kokutheleleka ngogcusula kanye nokuvela kophawu lokuqala yizinsuku ezingama-21 kodwa umehluko ungaba phakathi kwezinsuku eziyi-10 kuya kwezingama-90.
Kunezigaba ezi-4 zikagcusula:
- Isigaba sokuqala: isilonda/ izilonda zokuqala zivela lapho ugcusula wangena khona emzimbeni. Isilonda asibuhlungu ngakho singase singanakeki. Sihlala amasonto ama-3 kuya kwayi-6 futhi selapheka ngokulashwa noma ngaphandle kokwelashwa. Intombazane ekhulile enogcusula ingaba nezinkinga eziningi zempilo, ingazala ingane enesisindo esincane, ingane ingazalwa ngaphambi kwesikhathi noma izalwe isishonile.
- Isigaba Sesibili: ukuqubuka kwesikhumba engxenyeni eyodwa noma ngaphezulu komzimba kanye/noma izilonda emlonyeni, esithweni sangasese noma esithweni sangemuva phakathi kwezinqe. Ukuqubuka akulumi futhi kungase kungabonakali. Izilonda ezinkulu ezivuvukele, ezimpunga noma ezimhlophe zingase zivele emlonyeni, emakhwapheni noma embilaphweni.
Ezinye izimpawu zibandakanya:
- Imfiva
- Izindlala ezivuvukele ezinoketshezi i-lymph (lymph glands)
- Umphimbo obuhlungu
- Ukuqothuka kwezinwele
- Ikhanda elibuhlungu
- Ukuncipha kwesisindo
- Ubuhlungu bezicubu
- Ukukhathala
- I-Condylomas (izilonda ezifana nezinsumpa)
Izimpawu ziphela ngokwelashwa nangaphandle kokwelashwa. Uma ungelashwa, ukutheleleka kuzodlulela esigabeni esicashile futhi okungenzeka kube isigaba sokugcina sesifo.
Isigaba esicashile ( esifihlekile): Izimpawu zesigaba sokuqala nesesibili ziyanyamalala. Ngaphandle kokwelashwa azikho izimpawu, kodwa ugcusula uba khona emzimbeni. Lesi sigaba sicashile singahlala iminyaka.
Isigaba sakamuva: Izimpawu zingavela eminyakeni eyi-10 kuya kwengama-30 ngemuva kokutheleleka futhi zibandakanya:
- Ubunzima ekuxhumaniseni ukunyakaza izicubu ngendlela
- Ukukhubazeka
- Ukuba ndikindiki
- Kuya ngokuya amehlo eya ngokufiphala angaboni kahle
- Isifo sokukhohlwa
- Lesi sifo silimaza izitho zangaphakathi okubalwa kuzo ubuchopho, imizwa, amehlo, inhliziyo, imithambo, namalunga. Lo monakalo ungaholela ekufeni.

Ukuvimbela: Indlela okuyiyonayona ephephe ngokugcwele (100%) ekugwemeni lesi sifo ukugwema ukuya ocansini, noma ukuthandana nomuntu oyedwa isikhathi eside ebudlelwaneni bakho ngokocansi, nomuntu omethembayo ohloliwe futhi owaziwayo ukuthi akanalo igciwane. Amakhondomu awakuvikeli ngasosonke isikhathi - ukuthintana nesilonda esisendaweni ebingamboziwe yikhondomu kungenza utheleleke.
Izilonda zikagcusula ezisemlonyeni, ngemuva phakathi kwezinqe, emgudwini wesitho sowesifazane sangasese noma epipini zenza kube lula ukudlulisela noma ukuthola ukutheleleka nge-HIV. Usengcupheni ephindwe ka-2 kuya koku-5 yokuthola i-HIV uma ungavikelekile lapho kukhona khona izilonda zikagcusula.
Khumbula: izilonda zingafihleka esithweni sowesifazane sangasese, ngemuva phakathi kwezinqe, ngaphansi kwejwabu noma emlonyeni.
Ukuhlolwa: Ngokujwayelekile kuhlolwa igazi.
Wonke umuntu wesifazane okhulelwe kufanele ahlolelwe ugcusula ngesikhathi ekhulelwe nalapho ebeletha, ngoba ugcusula ongelashiwe ungangena futhi ubulale ingane yakhe ayikhulelwe.
Ukwelashwa: Ugcusula ngokujwayelekile kulula ukuwelapha ngama-antibiotics. Ukwelashwa kungawuqeda ugcusula futhi kuvimbe umonakalao omkhulu ongenzeka, kepha ngeke kwalungiseka umonakalo obese wenzekile.
Kungaholela: Buka izigaba zikagcusula.
Igama: I-Lymphogranuloma (LGV)
Uhlobo: Ibhakthiriya
Incazelo: I-LGV iwukutheleleka okubangelwa yizinhlobonhlobo zebhakthiriya i-iChlamydia Trachomatis (okungeyona i-chlamydia)
Imbangela: Ukuthintana ngqo ngocansi olubandakanya izitho zangasese, umgudu we-rectum noma ngocansi lomlomo. Ijwayeleke kakhulu emadodeni enza ucansi namanye amadoda.
Izimpawu: Zingaqala ezinsukwini ezimbalwa kuya enyangeni emva kokuthola ibhakthiriya.
Izimpawu zingafaka phakathi:
- Izinduna/amabhamuza ezithweni zowesilisa zangasese /emgudwini wezitho zowesifazane zangasese okwelapheka kalula ngaphandle kokushiya umaka.
- Igazi noma ubovu obuvela emgudwini wethumbu, i-rectum (igazi endleni).
- Ubuhlungu uma uzikhulula.
- Izilonda ezincane ezingebuhlungu.
- Ukuvuvuka nokuba bomvu kwesikhumba endaweni yembilapho.
- Ukuvuvuka kwezindebe zemomozi.
- Ukuvuvuka kwemithambo yembilapho maduze nomgudu we-rectum kubantu abaya ocansini olubandakanya isitho sangemuva phakathi kwezinqe.
- Uhudo kanye nezinhlungu esinyeni.
Ukugwema: Gwema ukuthintana ngqo nezitho zangasese, umgudu we-rectum noma umlomo womuntu othelelekile. Khumbula kungase kungabi khona izimpawu ezibonakalayo.
Ukwelashwa: Kuyelapheka ngama-antibiotics. Ukukhanywa kwezindawo ezivuvukele/ezinobovu ngokusebenzisa inalithi noma ngokusika izicubu.
Uma ungalashiwe kungaholela:
- Izingane ezisanda kuzalwa zingathola lesi sifo komama abanalesi sifo ngesikhathi zibelethwa.
- Ukuxhumana okungajwayelekile phakathi komgudu we-rectum nesitho sangasese.
- Ukutheleleka kobuchopho (okungavamile kakhulu).
- Ukutheleleka kwamalunga, amehlo, inhliziyo noma isibindi.
- Ukuvuvukala okuthatha isikhathi eside nokuvuvukala kwezitho zangasese.
- Ukulimala nokuncipha komgudu we-rectum.
- Izinkinga zingenzeka eminyakani eminingi ngemva kokuba utheleleke okokuqala.
Igama: I-Chancroid
Uhlobo: Ibhakthiriya
Incazelo: I-Chancroid yi-STI ebangwa yibhakthiriya. Ijwayele ukutholakala emazweni aseduze nenkabazwe kodwa ayivamile kwezinye izingxenye zomhlaba.
Imbangela: Ukuya ocansini nomuntu onegciwane. Amathuba maningi okungenwa yileli gciwane uma umuntu engagcini imithetho yenhlanzeko futhi uma owesilisa engasokile.
Izimpawu: Ngokujwayelekile yisilonda esisodwa noma eziningana noma amaqhubu azungezwe ngumbala obomvu ngaphandle noma ngaphakathi esithweni sangasese, kungathatha izinsuku ezi-4 kuya kweziyi-7 ngemva kokutheleleka.
Izilonda zingashesha ukugcwala ubovu futhi ziqhume, zishiye izilonda ezivulekile ezibuhlungu. Kwabayingxenye abathelelekile izindlala zembilapho ziba nkulu, ziqine, zibe buhlungu, ziphenduke izigaxa ezithambile ezivuvukele ezingagcina ngokuqhuma.
Ukugwema: Indlela okuyiyona ephephe ngokugcwele (100 %) wukugwema ukuthintana ngokocansi, noma ukuba sebudlelwaneni bothando nomuntu oyedwa othembekile ohloliwe futhi omaziyo ukuthi akanalo igciwane.
Amakhondomu awavikeli ngasosonke isikhathi. Ukuthintana nesilonda esisendaweni ebingamboziwe yikhondomu kungenza utheleleke.
Uma ucabanga ukuthi unegciwane gwema noma yikuphi ukuxhumana ngocansi futhi uhlolwe. Yazisa nabobonke oya nabo ocansini ukuze bahlolwe.
Ukwelashwa: Ama-Antibiotics ayayelapha i-Chancroid (izilonda ziphola engakapheli amasonto amabili).
Lokhu kungaholela: Uma kungelashiwe kungabangela izilonda ezithweni zangasese ezingahlala amaviki noma izinyanga. Ingozi inkulu yokuthola i-HIV.
Igama: I-Hepatitis B
Uhlobo: Ivayirasi
Incazelo: I-Hepatitis B yisifo esithathelwanayo sesibindi esibangelwa yivayirasi ye-Hepatitis B. Ingadluliseka nangokuthintana okungekona okocansi.
Imbangela:
- Ukuthintana ngqo noketshezi lomzimba olutheleleke nge-hepatitis (uketshezi locansi, igazi, amathe).
- Ngenxeba noma ngezindawo eziswakeme ngaphakathi (iso).
- Ukuthintana ngokocansi.
- Ukujova usebenzisa izidakamizwa kanye nokubolekisana ngezinalithi.
- Ukuthelelana ngenkathi yokubeletha kusuka kumama kuya enganeni.
- Ukubolekisana ngezinsingo noma ngezixubho nomuntu onegciwane.
Izimpawu: Izimpawu zingase zingabonakali.
Uma zikhona, izimpawu zingabandakanya:
- imfiva
- ukukhathala
- ukungathandi ukudla
- isicanucanu
- ukuphalaza
- isisu esibuhlungu
- umchamo omnyama
- indle enombala osabumba
- ubuhlungu bamalunga
- ijondisi – isikhumba siba nombala ophuzi amehlo abemhlophe
Ukuvimbela: Gwema ukuthintana noketshezi lomzimba (igazi, uketshezi locansi, amathe) womuntu othelelekile.
Ivayirasi iyakwazi ukuphila ngaphandle komzimba womuntu ngaphezu kwezinsuku eziyi-7 iqhubeke nokubanga ukutheleleka.

Ukwelapha: Uma ukutheleleka kukukhulu, ayikho imithi yokukwelapha, ukwelapha ngokokweseka isiguli.
Uma ukutheleleka kuyisimbelambela, kudingeka imishanguzo. Kubantu abane- HBV eyisimbelambela ukutheleleka kudinga ukuhlolwa njalo kwemithi esetshenziswayo nokukuqaphela njalo njalo.
Ingaholela kulokhu:
- I-hepatitis eyisimbelambela.
- I-Cirrhosis (ukushiya izibazi) yesibindi noma umdlavuza wesibindi.
Igama: I-Human Papillomavirus (HPV)
Uhlobo: Ivayirasi
Incazelo: I-HPV yi-STI edalwa yivayirasi futhi ijwayelekile kakhulu, kanti futhi kunezinhlobo ezingaphezu kwama-40 ezingatholakala emlonyeni/emphinjeni kanye nasezithweni zangasese zabesilisa ezabesifazane.
Imbangela:
- Ucansi olubandakanya umgudu wesitho sangasese sowesifazane, isitho sangemuva phakathi kwezinqe kanye nocansi lomlomo.
- I-HPV ingaqubuka emva kweminyaka kwaba nokuthintana.
- Ungathola ngaphezu kohlobo olulodwa lwe-HPV.
- Izingana ezizelwe zingatheleleka ngesikhathi sokubeletha.
Izimpawu: Abaningi abantu abane-HPV abanazo izimpawu noma izinkinga ngokwempilo kodwa basangayedlulisa ivayirasi ngaphandle kwezimpawu.
Uhlelo lokuzivikela komzimba luyayiqeda i-HPV eminyakeni emibili. Uma kungenjalo, kuba nezinsumpa esithweni sangasese zixhobelane kube yiqhutshana noma kuhambe kuba ngamaqhutshana amaningi esithweni sangasese. Izinsumpa zingaba zincane noma zibe nkulu, zenze igqunyana, noma zisabalale ngaphandle kokwenza igqunyana kanti isimo sazo zibukeka njengo-cauliflower.

Ukuvimbela:
- Okuyiyona ndlela eyodwa ephephile yokuvimbela i-HPV wukugwema zonke izinhlobo zocansi.
- Amakhondomu angahle angavikeli ngokuphelele ngoba izindawo ezingamboziwe yikhondomu zingatheleleka nge-HPV.
- Imigomo (vaccines) ingabavikela abesilisa nabesifazane ezinhlontsheni eziningi ezijwayelekile ze-HPV ezingaholela ezifweni noma umdlavuza. Kubalulekile ukugonywa kathathu ukuthola ukuvikeleka okuphelele.
- Ukuhlolwa njalo uhlolelwa umdlavuza womlomo wesibeletho ukuze uthole izimpawu nokwelashwa ukuvikela umdlavuza. Okunye okungumdlavuza ohlobene ne-HPV kungahle kungabi nankomba noma izimpawu kuze kufike lapho sekuhambe kakhulu kwaze kwanzima ukukwelapha.
Ukwelapha: Izinsumpa zesitho sangasese ezibonakalayo ungazisusela zona ngokusebenzisa imithi oyiyalelwe ngabezempilo noma zingelashwa yisisebenzi sezempilo.
Kungaholela kulokhu: I-HPV ingenza ukuthi amaseli (cells) ajwayelekile aphenduke angejwayelekile eziveza ngesimo sezinsumpa zesitho sangasese noma umdlavuza. Lokhu kufaka phakathi umdlavuza womlomo wesibeletho, wemomozi, womgudu wesitho sangasese sabesifazane, wepipi, wesitho sangemuva phakathi kwezinqe kanye nowomphimbo.
Uma ingelashwanga, izinsumpa kungenzeka zinyamalale, zihlale zikhona noma zande ngobuningi noma zikhule zibe nkulu.
Igama: Ihephisi yezitho zangasese (Genital Herpes)
Uhlobo: Ivayirasi
Incazelo: I-Genital Herpes yi-STI ebangelwa ngamavariyasi e-herpes simplex. Ayelapheki kodwa iyathibeka.
Imbangela: Ucansi lwesitho sangasese sowesifazane, lwesitho sangemuva phakathi kwezinqe, nolomlomo.
Izimpawu: Zingase zingabi mawala kangako, zingase zingabonakali kodwa ngokujwayelekile zivela njengebhamuza elilodwa noma ngaphezulu esithweni sangasese noma ezindaweni ezizungeze isitho sangasese, emgudwini we-rectum noma emlonyeni. Kuba namabhamuza avelayo ashiya izilonda ezibuhlungu ezingathatha amasonto ama-2 kuya kwa-4 ukuba ziphole. Uma iqala iziveza umuntu angathola enezimpawu ezinjengomkhuhlane, imfiva, ubuhlungu bomzimba nokuvuvuka kwezindlala. Ukuphindaphindeka kokuvela kwe-genital herpes kuyinto ejwayelekile.
Ukuyigwema: Ukusetshenziswa ngokufanele kwamakhondomu e-latex kunganciphisa ingozi ye-genital herpes, kodwa ingaziveza ezindaweni ezingamboziwe ikhondomu. Uma kukhona izilonda, gwema ukuya ocansini. Ngisho noma umuntu engenazo izimpawu, labo aya nabo ocansini bangatheleleka.
Ukwelashwa: Alikho ikhambi le-herpes. Imishanguzo inganqanda noma inciphise ukuqubuka kwezifo ngesikhathi umuntu elashwa.
Kungaholela kulokhu:
- Amathuba makhuu okwedlulisela i-HIV uma omunye wezithandani ene-HIV.
- Ekuphuphumeni kwesisu noma ukuzalwa komntwana kungakabi yisikhathi.
- Umama angadlulisela ukutheleleka emntwaneni okungaholela ekuthelelekeni okwesabekayo (neonatal herpes).
- Kuyingozi emntwaneni ukuthola i-herpes ngesikhatho sokukhulelwa.
Igama: I-Human Immunodeficiency Virus (HIV)
Uhlobo: Ivayirasi
Incazelo: I-HIV yi- Human Immunodeficiency Virus. Yivayirasi elingaholela ekutholeni i-Acquired Immune Deficiency Syndrome (AIDS).
Imbangela: Ngokwenza ucansi olungavikelekile (ngaphandle kwekhondomu) nomuntu one-HIV. Ivayirasi liyathubeleza emzimbeni kalula uma kunezilonda (isikhumba esisikekile) zama-STI.
Ngokuthintana negazi elitheleleke ngegciwane le-HIV. Isibonelo:
- Ukubolekana ngezinalithi ezingcolile
- Izinsingo
- Izinsingo zokuzidweba esikhumbeni (tattoo needles)
- Amathuluzi okubhala noma okudweba isikhumba
- Ukwabelana ngegazi okungaphephile.

Ngokuyedlulisa isuka kumama iya emntwaneni. Intombazane ekhulelwe ene-HIV ingadlulisela i-HIV emntwaneni ngenkathi ikhulelwe, ngesikhathi ibeletha noma ngokuncelisa.
Izimpawu: Emavikini okuqala umuntu ethelelekile, abanye abantu baba nezimpawu zomkhuhlane, kodwa abanye abanazo nhlobo.
Abantu abaphila ne-HIV bangabukeka futhi bazizwele bephilile iminyaka eminingi. Ngaphandle kokwelashwa, futhi ngenkathi uhlelo lomzimba lokuzivikela luba buthaka, izinhlobo eziningi zokugula zingaqala ukubonakala.

Ukuvimbela:
- Gwema ukuthintana negazi/uketshezi locansi lomuntu othelelekile.
- Ukusetshenziswa njalo kwamakhondomu ngendlela efanele kungayinciphisa ingozi yokuthelelana.
- Ukusoka kwabesilisa kunciphisa ingozi yokuthelelana kusuka kwabesifazane kuya kwabesilisa ngesikhathi socansi olubandakanya umgudu wesitho sangasese sowesifazane.
- Ukuvimbela ukuthelelana phakathi kukamama nomntwana uma ukhulelwe.
Ukwelashwa: Ukwelashwa ngemishanguzo kungayelula impilo yomuntu one-HIV aphile impilo ejwayelekile uma kwenziwa ngendlela efanele. Ukuze imishanguzo (ARVs) ikwazi ukulawula i-HIV nokuyivimba ukuthi ingasabalali (izandise), kumele okungenani uthathe imithamo eyi-19 kwengama-20. Lokhu kubizwa ngokunamathela kokulindelekile.
Okungaholela kukho: Ngaphandle kokwelashwa i-HIV, lokho kungaholela ekubeni nengculazi (AIDS) esigabeni sokugcina se-HIV, lapho uhlelo lokuzivikela komzimba selulimele kakhulu futhi umuntu esenenkinga yokulwa nezifo kanye nemidlavuza ethile. Namuhla abantu bangaphila cishe iminyaka benayo i-HIV uma besebenzisa ngokufanele ama-ARVs.
Igama: I-Molluscum Contagiosum (MC)
Uhlobo: Ivayirasi
Incazelo: I-Molluscum Contagiosum ibangelwa yivayirasi eyilungu lomndeni we-poxvirus. Ungathola ukutheleleka ngezindlela ezinhlobonhlobo.
Imbangela: Ukuthintana ngocansi kanye nokuthintana nezinto ezingcolile, njengamathawula, izingubo kanye namathoyizi.
Izimpawu:
Amaqhutshana amancane angenabuhlungu abuye athi ukuphakama, abe nombadlana othi awube mhloshana noma phuzi maphakathi nendawo kuwo.
Ukuwenwaya kungawandisa abe ngumugqa noma abe ngamaqoqwana abizwa ngokuthi yizitshalo futhi kwenze sibe bomvu isikhumba.
Ngokujwayelekile abonakala ezithweni zangasese, esiswini nangaphakathi kwamathanga.
Izilonda ezivela ngasekuqaleni (amaqhutshana) eziba sezithweni zangasese ezingase zichazwe ngokuliphutha njenge-hephisi noma izinsumpa kodwa kungafani nehephisi, ngoba zona azibuhlungu. I-MC ijwayelekile ezinganeni ezitheleleka ngokuthintana naleli qhutshana.
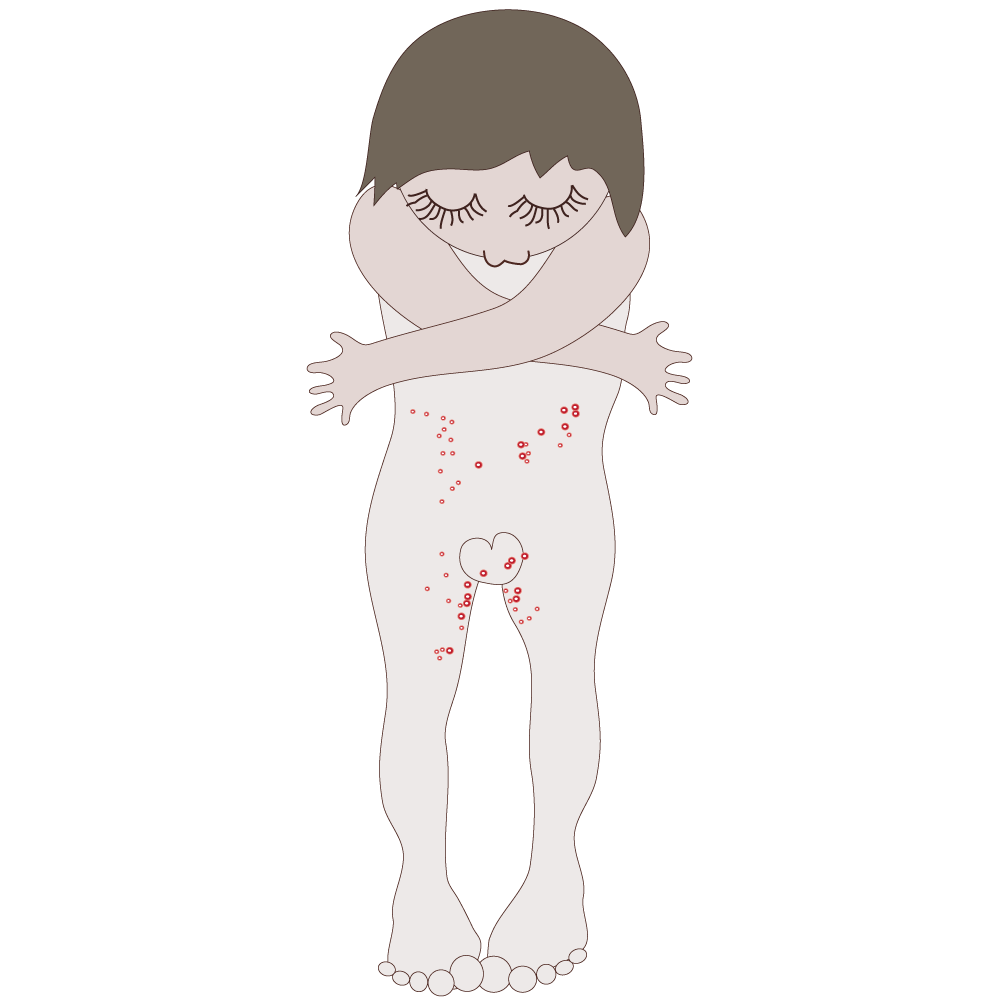
Ukugwema:
- Gwema ukuthintana ngqo nezilonda zesikhumba.
- Ningabolekisani ngamathawula, ngezingubo zokulala, ngezingubo zokugqoka nabanye abantu.
- Ukugwema ucansi kungakuvimba ukutheleleka nge-molluscum virus. Ngisho nangesikhathi usebenzisa ikhondomu ukutheleleka kusengenzeka ngokuthintana ezindaweni ezingamboziwe yikhondomu.

Ukwelashwa: Lokhu kutheleleka ngaleli gciwane kuyaziphelela ngokwakho emva kwezinyangana ezimbalwa (kwesinye isikhathi kungaba ngunyaka noma iminyaka emibili) kepha esimweni lapho uhlelo lokuzivikela komzimba lubuthakathaka isimo singaba sibi.
Kunemithi isisebenzi sezempilo esingakunika yona ukwelapha la maqhutshana, kepha futhi angasuswa ngokuhlinzwa kepha lokho kungase kudale izibazi.
Kungaholela kulokhu: Ukusabalala nokuphindaphindeka kwezilonda/amaqhutshana nezinye izifo zesikhumba ezithathelwanayo.
Igama: Isifo sokutheleleka ezithweni zenzalo (Pelvic Inflammatory Disease /PID)
Uhlobo: Ukudlebeleka kwamanye ama-STI
Incazelo: I-PID iwukudlebeleka okuyingozi kwezifo ezithile ezithathelwana ngocansi (STI). I-PID ingawalimaza amashubu enzalo (fallopian tubes) kanye nezicubu ngaphakathi naseduze kwesibeletho kanye nama-ovari. I-PID ingaholela emiphumeleni engemihle neze, okufaka phakathi ukuphelelwa yinzalo (ukungakwazi ukuthola abantwana), ukukhulelwa ngaphandle kwesibeletho (ectopic pregnancy) kanye nokudaleka kwamathumba.
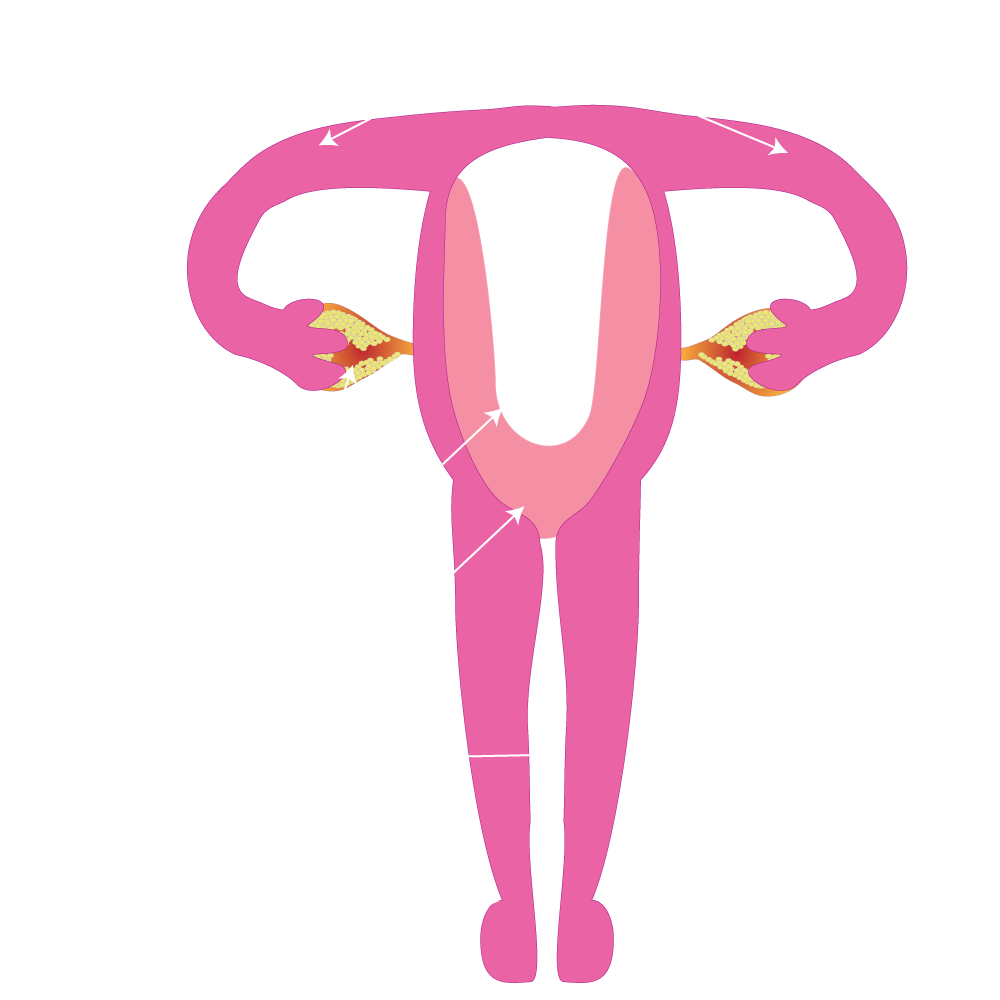
Imbangela:
- Izifo ezithathelwana ngocansi ezingelashiwe ezenyukela phezulu ezithweni zokuzala.
- Izifo ezithathelwana ngocansi ezingelashiwe, ikakhulu i-chlamydia kanye nesipatsholo (gonorrhoea).
- I-PID yenzeka lapho amabhakthiriya (amagciwane) enyukela phezulu esuka emgudwini wesitho sentombazane sangasese noma umlomo wesibeletho eyongena ezithweni zokuzala.
- Amantombazane asemancane asemathubeni amaningi e-PID ngoba umlomo wesibeletho sawo awukhulile ngokwanele, lokhu kwenyusa amathuba okutheleleka ngama-STI ahlobene ne-PID.
- Intombazane eya ocansini nabantu abaningi, inamathuba amakhulu engozi yokuba ne-PID ngenxa yokuhlala isengozini enkulu yokutheleleka.
- Amantombazane akhaphazela (douche) ngemikhiqizo engaphephile ukugeza ingaphakathi lezitho zangasese azibeka engozini enkulu yokuba ne-PID.
Ukuvimbela:
- SUkwenza ucansi oluphephile.
- Ukuhlolwa nokwelashwa kwama-STI.
- Gwema ukugeza izitho zangasese ngemikhiqizo engaphephile.
Izimpawu:
- Izimpawu ze-PID ziyehlukana ukusuka kwezincane kuya kwezinzima
- I-PID ebangelwa yi-Chlamydia ingaholela ezimpawini ezingatheni, ngisho noma umonakalo omkhulu wenzekile emashubhini enzalo nasezithweni zenzalo.
- Amantombazane kanye nezisebenzi zezempilo kabavamisile ukuyibona i-PID
- Uphawu olujwayeleke kakhulu wubuhlungu esinyeni.
- Ezinye izinkomba nezimpawu zifaka phakathi imfiva, uketshezi oluphuma emgudwini wesitho sowesifazane sangasese olungajwayelekile olungaba nephunga elibi, ucansi olubuhlungu, ubuhlungu uma uchama, ukuya esikhathini okungejwayelekile, kanye nobuhlungu phezulu nesisu esandleni sokudla (okungejwayelekile).
Ukwelashwa: I-PID ingelapheka ngezinhlobo eziningi zama-antibiotics kodwa lokhu akuwulungisi umonakalo osewenzekile
DISTI
DiSTI ke ditshwaetso (mafu) a namang ka thobalano. Hangata di nama ka thobalano e sa sireletsehang eo ho yona kwae/ntoto e kengwang ka hara kuku kapa ka maraong a motho e mong , empa tse ding di ka nama ka ho momonwa ha setho sa botona kapa sa botshehadi le ho tsohedisana.

Di ne di tlwaetse ho bitswa mafu a fumanwang mothong ya seng a tshwaeditswe kapa mafu a fetiswang ka thobalano.
DiSTI tse kang maqhanyatsa/dipudula sethong sa botona/botshehadi (herpes), lekgopo, dinta le tshwaetso e bakwang ke baktheria e bitswang Chlamydia trachomatis di ka nama ka ho momonwa sethong sa botona/botshehadi le ho tsohedisana.

Boholo ba diSTI bo ka alafshwa haeba kalafo e fumanwa ka nako.

Balekane ba etsang thobalano (ka bobedi/kaofela) ba hloka ho alafshwa kapa ba tla tshwaetseha hape nakong ya thobalano e sa sireletsehang (STI e tla kgutla).
Netefatsa hore molekane wa hao le yena o fumana kalafo.

SDitshwaetso tse fetiswang ka thobalano (mafu) di nama ho tloha mothong e mong ho ya ho e mong ka boitshwaro ba mefuta e fapaneng ba thobalano.

DiSTI tse ngata di namiswa ke ho tswa ha lero (mathe, moroto, lero la ditho tsa bong) le/kapa ho tshwara madi a motho e mong.
DiSTI tse ding tse kang maqhanyatsa/dipudula sethong sa botona/botshehadi, dinta, lekgopo le tshwaetso e bakwang ke baktheria e bitswang Chlamydia trachomatis di nama ka ho kopana ha mmele ya batho.
DiSTI tse ding di ka nama ho tloha ho mme ho ya leseeng nakong eo mme a imileng, a nyantshang letswele kapa a belehang.

DiSTI di ka boela tsa fetiswa ka ho sebetsa ka madi ka tsela e sa bolokehang jwalo ka ho sebedisa nelete e le nngwe bathong ba fapaneng, nakong eo batho ba kenyang dithethefatsi ka ho itlhaba ka nalete methapong ya madi, ho itsheha letlalo hore ho be le mabadi a sa tloheng ho etsetsa tumelo e itseng setjheso kapa ho etsa thathu.


Maqeba a nalete e hlabang letlalo a ka fetisa le diSTI.
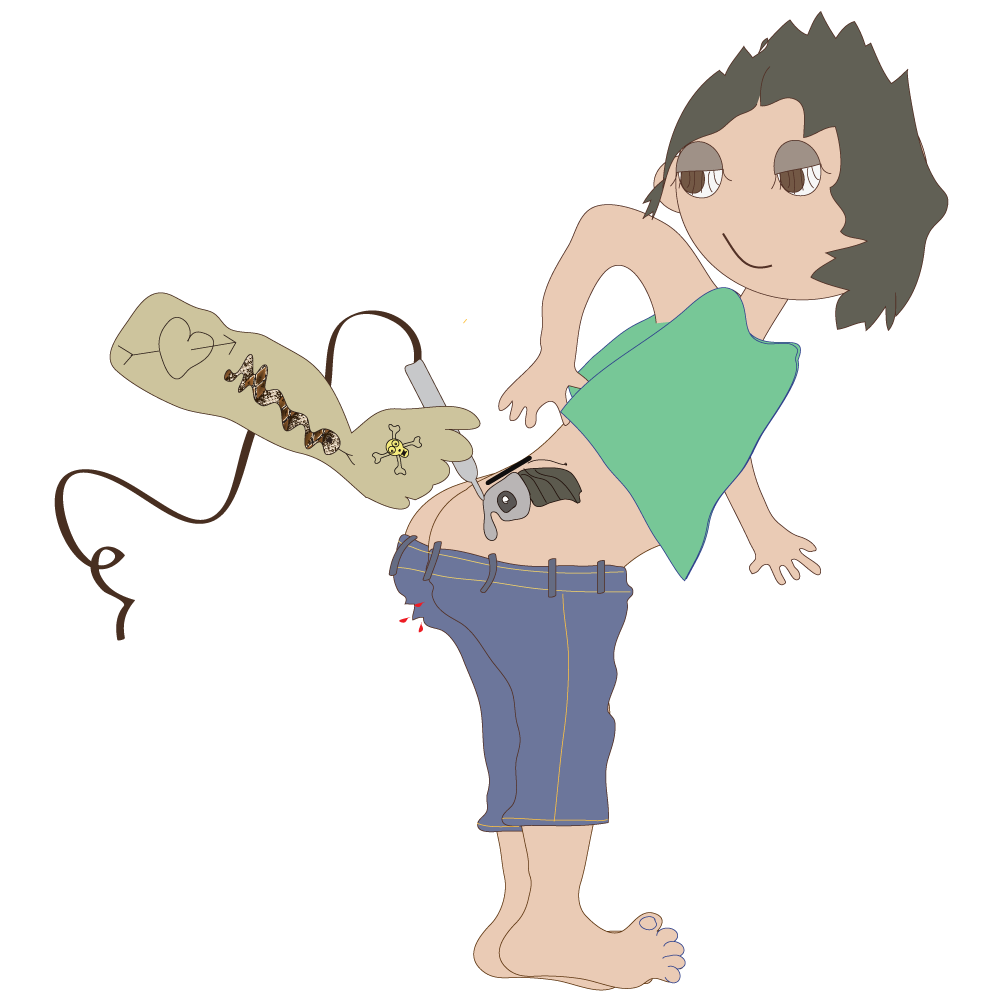
Thobalano e sa sireletsehang (ka maraong, kukung le ho momonwa ha setho sa botona/botshehadi). Ho se sebedise dikhondomo ketsahalong e nngwe le e nngwe le hona ka nepo.
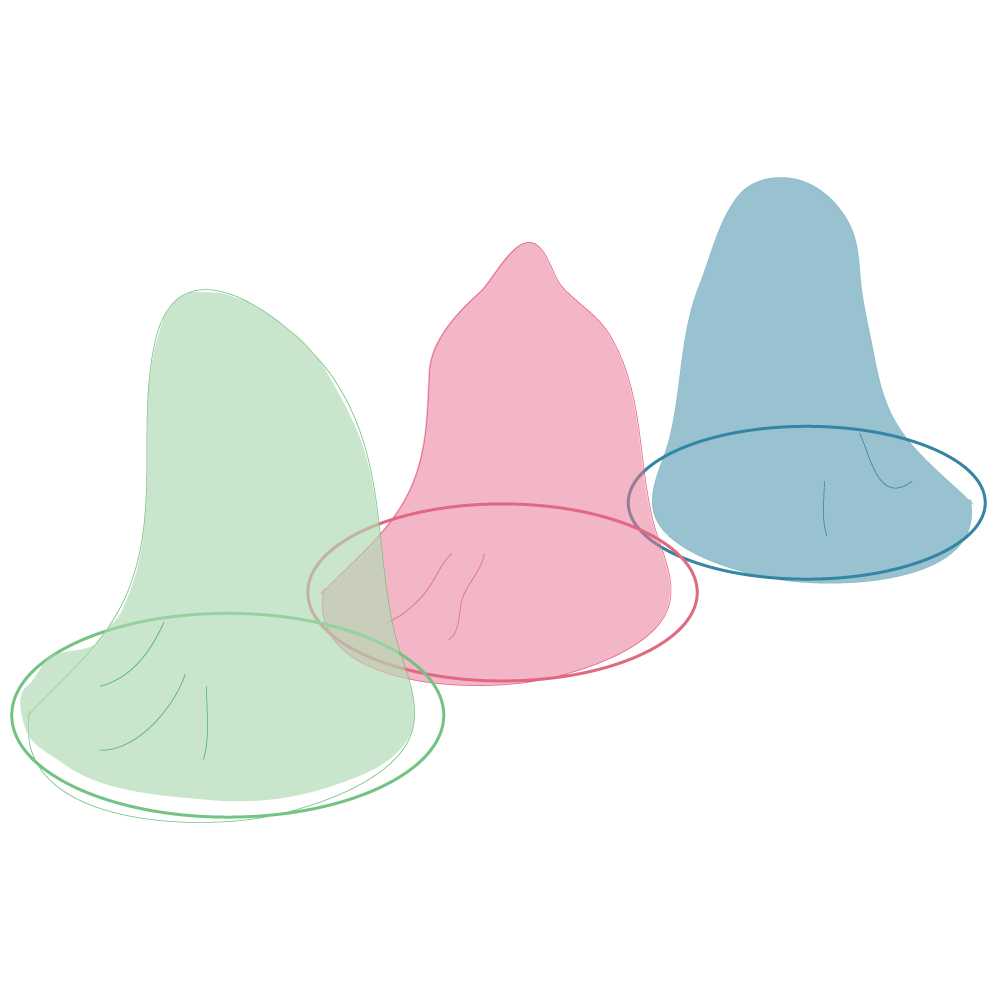
Ho ba le balekane ba bangata ba thobalano.

Ho apara diaparo tsa motho e mong tsa ka hare/ho sebedisa dibapadiswa tsa motho e mong tsa thobalano.

Ho fetisa ho tloha ho mme ho ya ngwaneng.

Dinalete tse sa hlwekang/leqeba la nalete e hlabang letlalo.
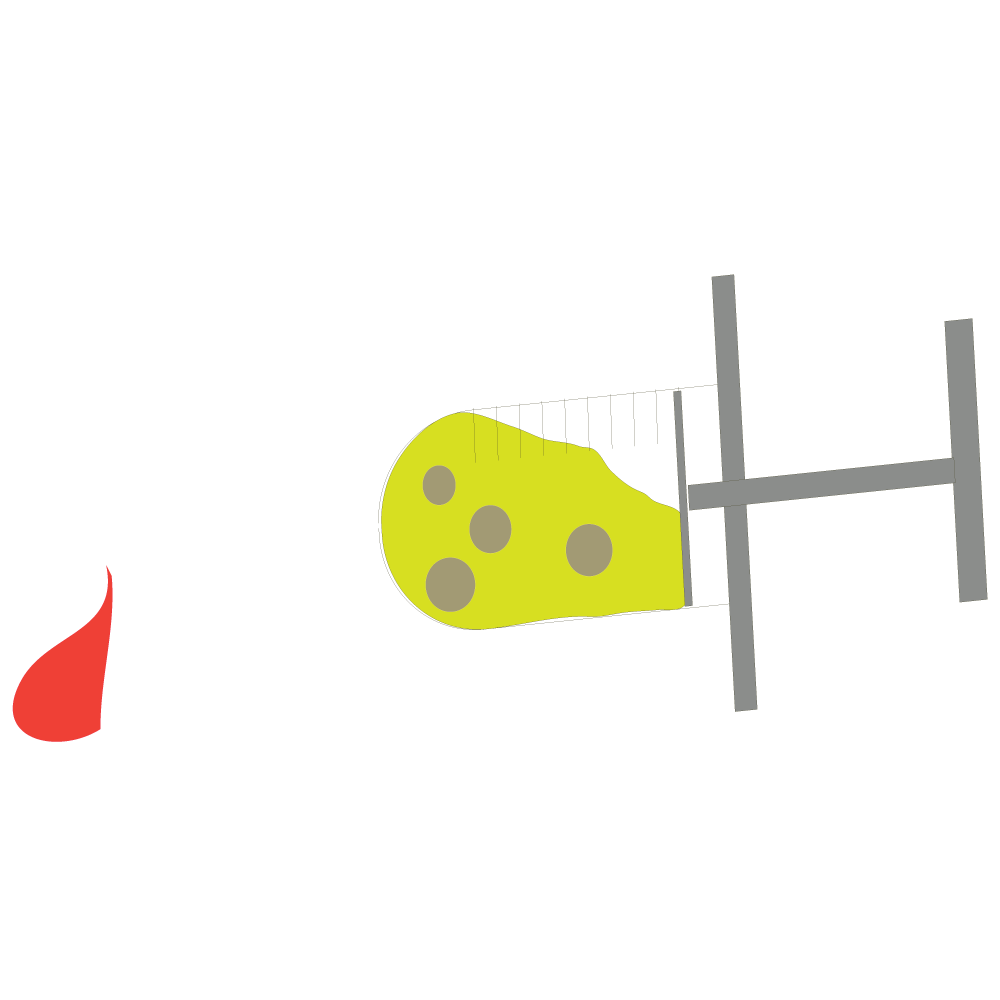
Hangata diSTI ha di utlwahale (ho ba le tshwaetso o sa be le matshwao). Ha di kgone ho bonwa.

Ke kahoo ho leng bohlokwa ho hlahlojwa.
Haeba o sa hlahlobe, o ke ke wa tseba hore o tshwaeditswe, kahoo o ke ke wa fumana kalafo mme o tla fetisetsa STI ya hao ba/molekaneng eo o etsang thobalano le yena.
* Letshwao le bolela hore ho na le ntho e leng teng, letshwao kapa ntho e bontshang ntho e sa tsamayeng hantle/lefu, haholoholo ha e le phetoho ya mosebetsi, maikutlo kapa ho bonahala ha ntho e sa tlwaelehang.
Ka dinako tse ding ha ho na matshwao kapa matshwao a nka nako ho hlaha.

DiSTI tse ding (Chlamydia le Morotwana (Gonorrhoea) ha di na matshwao, kapa ha di na matshwao qalong (DiSTI tse sa bontsheng).
Ho etsa thobalano e sa sireletsehang le motho ya nang le STI e mohatong o sa bonahaleng ho bolela hore o ka tshwaetswa ntle le ho bona matshwao afe kapa afe mothong.
Hona ho bolela hore o ka fetisa STI ya hao o sa tsebe le hore o na le yona. Kahoo diSTI di ka nama ho feta mme tsa baka mathata a jwalo ka tshwaetso popelong, ditjhupung tsa Fallopian kapa diouvaring (Pelvic Inflammatory Diseases (PID) le ho se be le pelehi.
Diso dithong tsa botona/botshehadi.
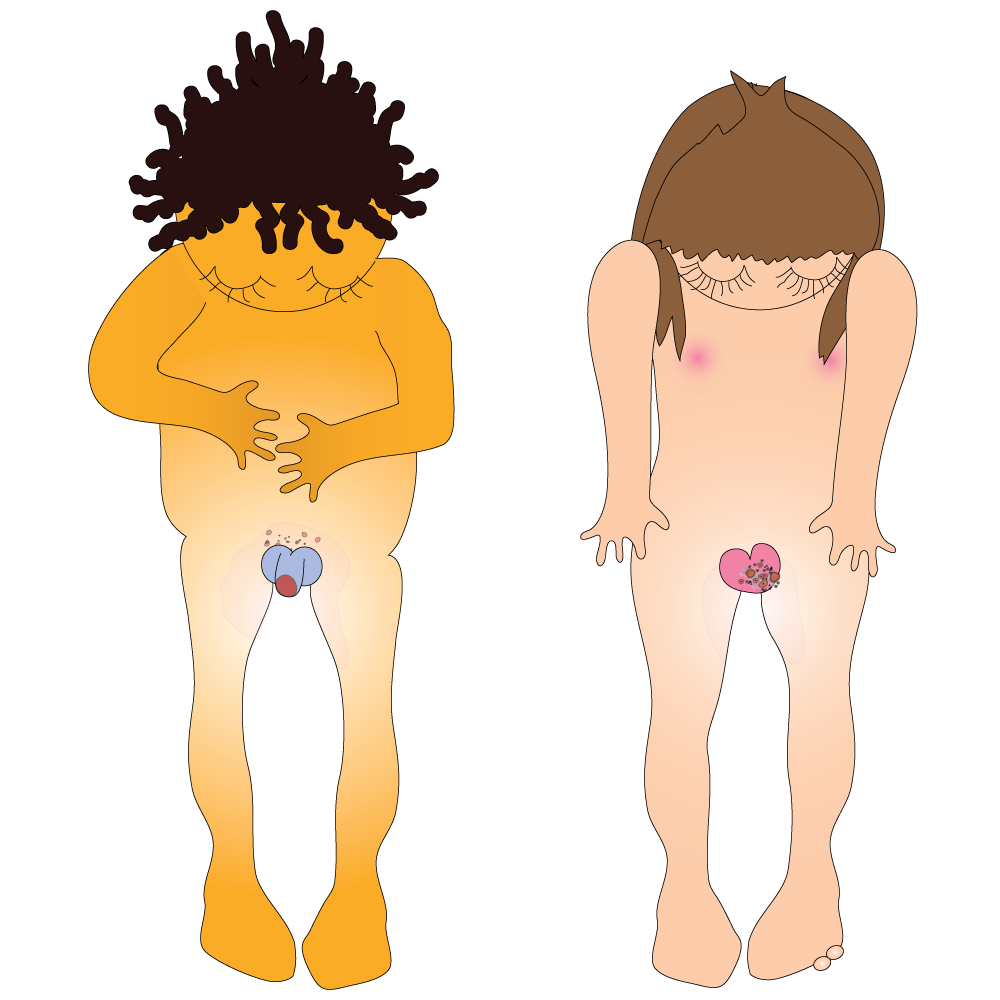
Makgopo /ho ruruha /ditshwelesa nokeng.
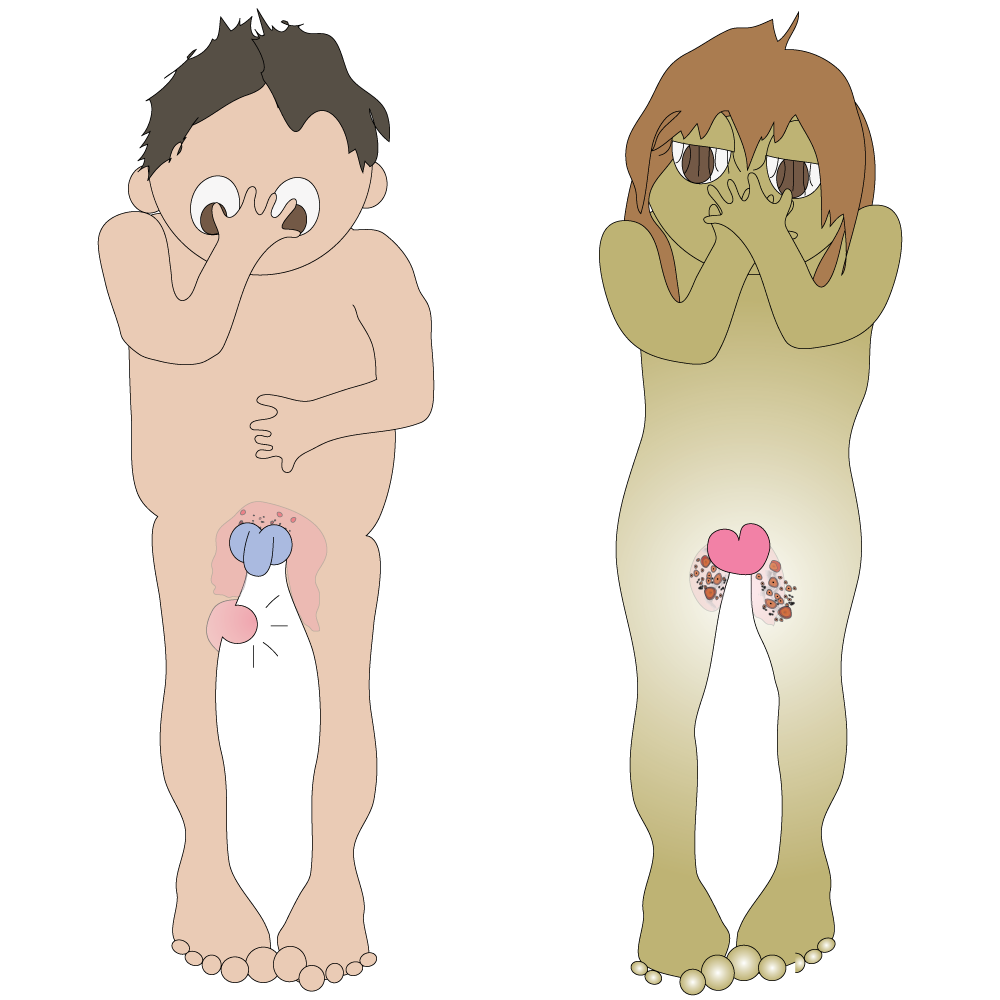
Lero le tswang kwaeng/ntotong kapa kukung.
Dihloba ka hare le ho potoloha kwae/ntoto kapa kuku /mokoteng.

Ho tjha ha o rota/ntsha metsi.

Lehlaba makwalateng/ditapoleng (bashemane).
Lehlaba mpeng e ka tlase (banana).
Ho hlohlona sebakeng se kantle ho ditho tsa botona/botshehadi (haholoholo bosiu).

Makgopo/maqeba/ditshwelesa/diso, ho opelwa le mahlaba mmeleng, ditshwelesa tse ruruhileng, le themphereitjha e hodimo, le matshwao a mang a mefuta.

O ka ba le STI e le nngwe kapa ho feta ka nako.
Haeba o nahana hore o na le STI, fumana kalafo ka potlako kamoo ho ka kgonehang. Boholo ba diSTI le ha e se tsona kaofela, bo alafeha habobebe.
O lokela ho hlahlobelwa STI haeba:
- o etsa thobalano mme o sa etsa tlhahlobo pele
- o entse thobalano e sa sireletsehang ya ho momonwa setho sa botona/botshehadi, ka kukung kapa ka mokoteng le molekane a le mong kapa ba bangata
- molekane wa hao wa thobalano o entse thobalano e sa sireletsehang le motho e mong eo e seng wena
O na le matshwao afe kapa afe a sa tlwaelehang a kenyeletsang:
- lero le sa tlwaelehang le tswang kwaeng/ntotong kapa kukung
- o utlwa bohloko ha o rota/ntsha metsi
- o na le diso kapa matswabadi a sa tlwaelehang sebakeng sa ditho tsa botona/botshehadi kapa ka (mokoteng)
- ho hlohlona kapa ho longwa karolong ya ditho tsa botona kapa tsa botshehadi
- ho utlwa bohloko nakong ya thobalano
Haeba o etsa thobalano mme wena kapa molekane wa hao a ka be a etsa thobalano le motho e mong osele, o lokela ho hlophisetsa ho etsa tlhahlobo dikgwedi tse ding le tse ding tse 6 -12.
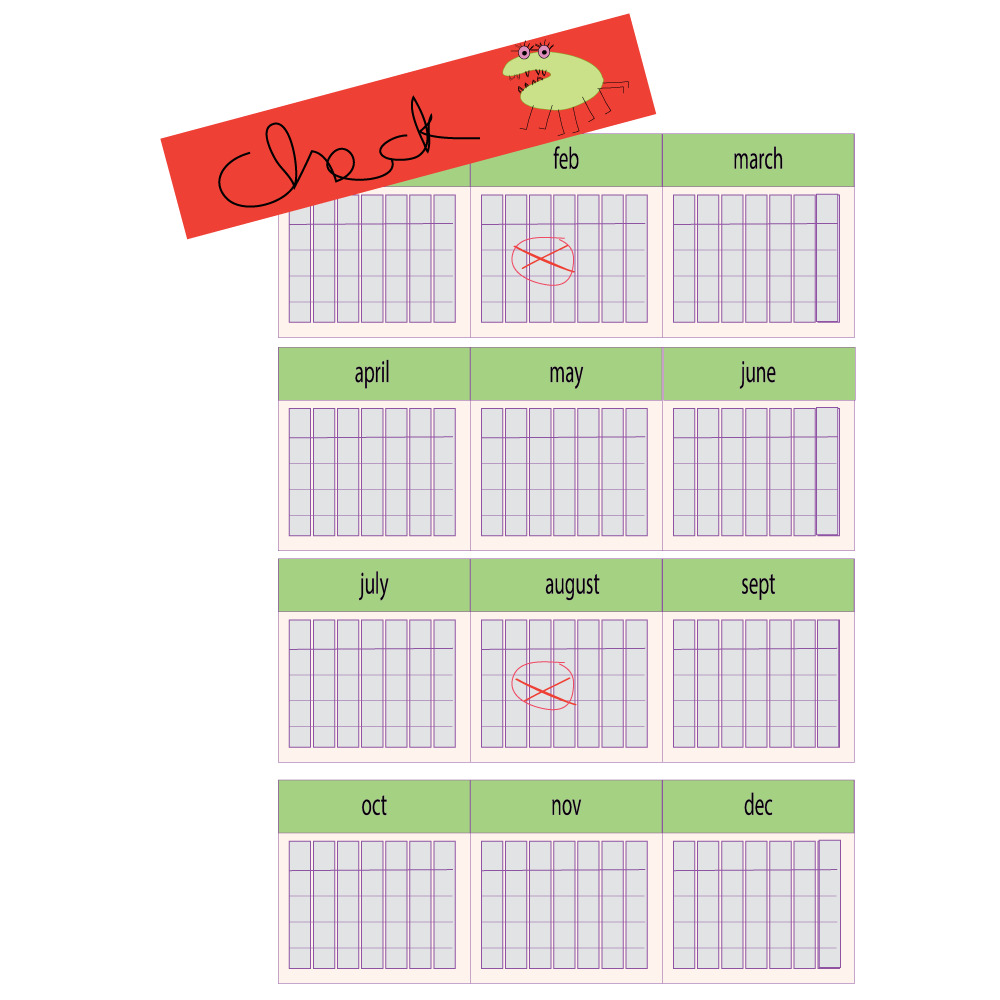
Ho hlahlobela STI ho bolela hore o etswa diteko tsa Ditshwaetso kaofela tse Fetiswang ka Thobalano ka nako e le nngwe.
Ho hlahloba hangata ho kenyeletsa:
- Diswapo (sampole ya mamina /thishu /madi e nkwang e kenngwe ka sekgetjana sa methiriele o monyang o kgomareditsweng thutswaneng e bonolo le ho romelwa laboratring ho ya etswa ditlhahlobo)
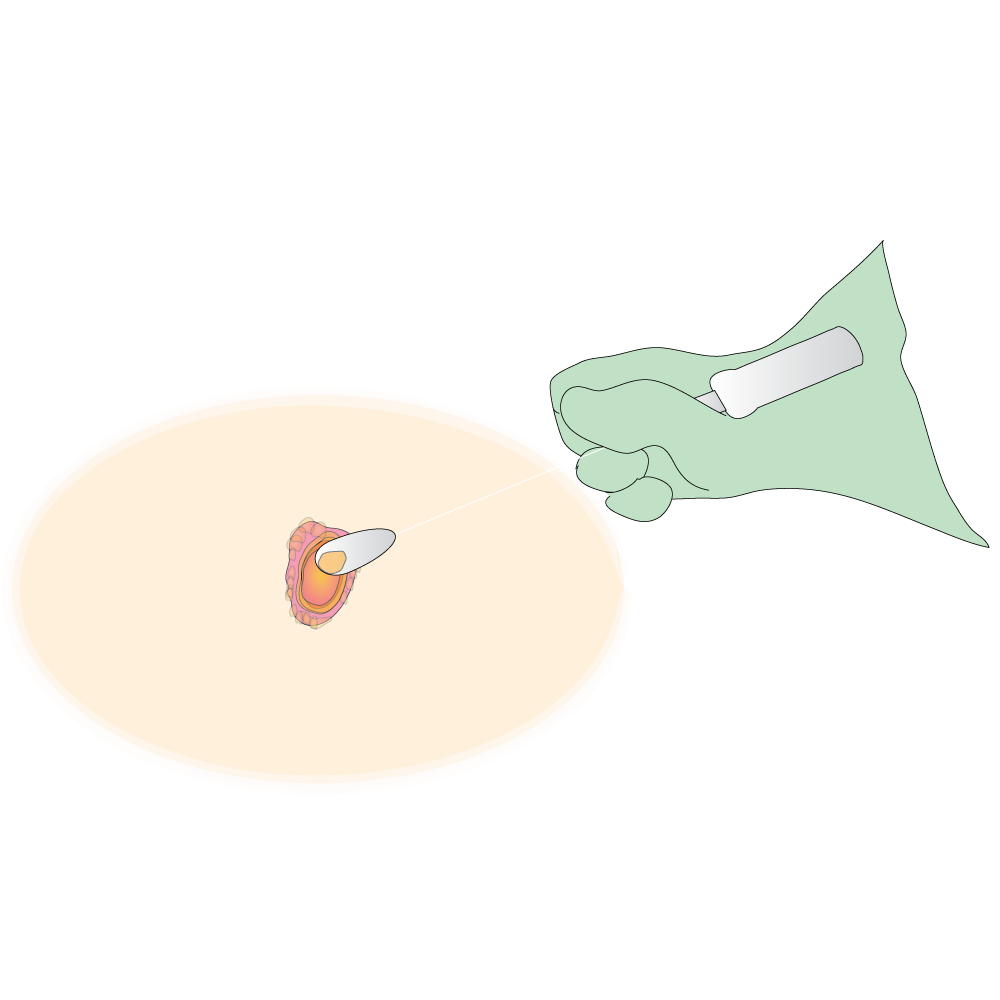
- Diteko tsa madi
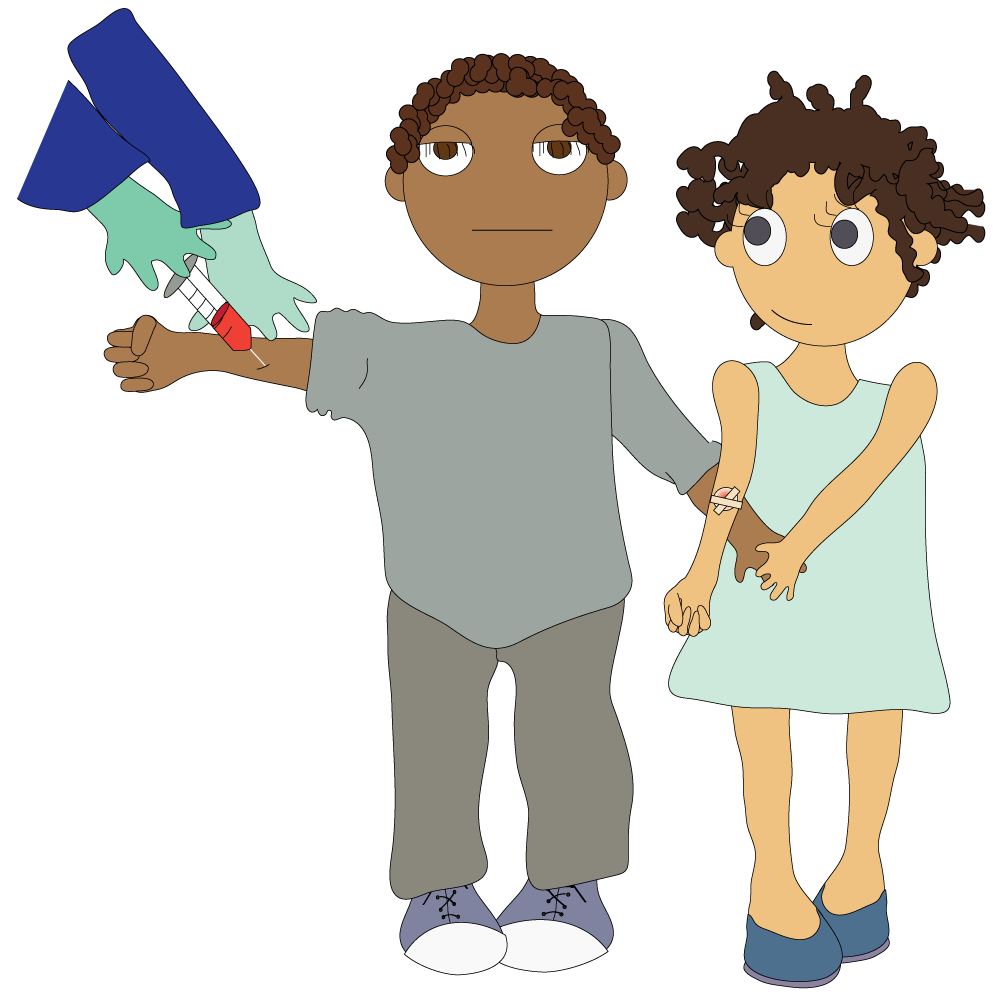
Ho hlahlobelwa STI ke mahala ditleleniking tsa mmuso. O tla hloka ho beheletsa letsatsi le nako ditleleniking tse ngata, ntle le ha ba fana ka tshebeletso ya ho itlela feela.
Ha o fumana kalafo ya STI netefatsa hore balekane ba hao kaofela ba thobalano ba a alafshwa. Haeba ho se jwalo, o ka fumana STI hape ha o boela o etsa thobalano le motho ya sa alafshwang.


Utlwisisa dintlha tse latelang pele o qala kalafo:
- Hobaneng o hloka moriana
- O nwa moriana jwang le hore neng le/kapa setlolo o se tlotsa hokae le hona jwang
- O boloka moriana jwang
- Ho ka etsahala eng haeba o sa nwe moriana jwalo ka ha ho laetswe
- O nwa moriana nako e kae
Kopa mosebetsi wa hao wa tlhokomelo ya bophelo hore a hlalose ntho e nngwe le e nngwe ka hloko le ho ngola ditaelo tsa meriana.

Ho bohlokwa haholo ho latela ditaelo tsa mosebetsi wa hao wa tlhokomelo ya bophelo.
- O se ke wa sebedisa moriana wa hao matshwaong afe kapa afe a lefu le leng ntle le lebakeng la matshwao ao e leng a moriana oo o laetsweng ho o nwa.
- O se ke wa nwa moriana wa motho e mong kapa wa fa motho e mong moriana wa hao.
- O se ke wa nwa moriana o mongata kapa o ka tlasa taelo, ntle le ha mosebetsi wa hao wa tlhokomelo ya bophelo a laetse jwalo.
Moriana wa ka o tla sebetsa hlantle hakae?
Bala dipolelo tse latelang. Na ho na le polelo efe kapa efe e o amang?
- Ka dinako tse ding ke lebala /kgutlisetsa nako ya ho Iata meriana ya ka ha e feela morao.
- Ka dinako tse ding ke lebala ho nwa meriana ya ka.
- Ka dinako tse ding ke nwa meriana ya ka ka dinako tse fosahetseng.
- Ke nwa meriana e mengata e fapaneng mme ka dinako tse ding ho boima ho e tseba.
- Ka dinako tse ding ke kgaotsa ho nwa meriana ha ke ikutlwa ke le betere.
- Ka dinako tse ding ke nwa meriana haholo kapa ka tlase ho taelo ya ngaka ya ka.
- Ka dinako tse ding ke kgaotsa ho nwa meriana ya ka hobane ke nahana hore ha e sebetse.
- Ha ke utlwisise hore ke tlameha ho nwa meriana ya ka neng.
- Ha ke botse mosebetsi wa ka wa tlhokomelo ya bophelo dipotso ka meriana ya ka hobane ke na le dihlong kapa ke a swaba.
Haeba o tshwaile boloko bofe kapa bofe, e ka nna ya ba ha o fumane molemo o felletseng merianeng ya hao.
Bua le mosebetsi wa hao wa tlhokomelo ya bophelo ka ho nwa meriana ya hao ka nepo - hoo ho tla thusa ka diphetho tsa kalafo ya hao e le ka nnete.

Dikhondomo di sireletsa boholo ba diSTI empa e seng kaofela ha tsona. Tsela e le nngwe feela ya ho dula o sireletsehile diphesente tse 100 ho diSTI ke ho se etse thobalano ho hang. DiSTI tse ding ha di bontshe matshwao, kahoo ha se kamehla o tlang ho tseba hore na o hloka ho hlahlojwa.
Tsela e le nngwe feela e thibelang Ditshwaetso tse Fetiswang ka Thobalano e le ka nnete ke ho se etse thobalano ka hohlehohle, kapa ho ba kamanong ya nako e telele le molekane a le mong, (ho tshepahala 100%) ya tshepahalang, ya entsweng diteko le ho tsejwa hore ha a tshwaetswa.
Dikhondomo ha di sireletse kamehla. Ho thetsa seso ka ntle ho karolo e kwahetsweng ke khondomo ho ntse ho ka baka tshwaetso.
Mokgwa o mong ke wa ho bua ka mefuta ena ya ditshwaetso pele o etsa thobalano le molekane e motjha, hore o kgone ho etsa dikgetho o na le kutlwisiso ka boemo ba kotsi boo o thabelang ho bo nka ka bophelo ba hao ba thobalano.

- Tlohela ho etsa thobalano haeba o kgona
- Diehisa ketso ya thobalano ha feela o ka kgona
- Sebedisa khondomo kamehla haeba o sa kgone ho diehisa thobalano
- Qoba ho etsa thobalano ha o le matsatsing
- O se ke wa sebedisa dinalete/mahare, jj. tse sedisitsweng ke motho e mong
- O se ke wa sebedisa dibapadiswa tsa thobalano kapa diaparo tsa ka hare tse sebedisitsweng ke motho e mong
- Hlahloba le ha o se na matshwao
- Fumana kalafo ya STI efe kapa efe e sa le nako
- Netefatsa hore ba/molekane wa hao le yena o fumana kalafo
- Qeta ho nwa kalafo ya hao
- Etsa ditlhahlobo kamehla
- Fetola boitshwaro ba hao ketsong ya thobalano
- Etsa thobalano e bolokehileng - sebedisa dikhondomo nako e nngwe le e nngwe
- Meento (diketsahalong tse itseng)
- Utlwisisa kalafo ya hao.
- Hore o e nwa jwang le hona neng

Bohlweki - ho netefatsa hore mmele wa hao o hlwekile.
Batho ba na le mehopolo e fapaneng ka bohlweki. Batho ba bang ba hlapa mmele ya bona bonyane letsatsi le leng le le leng le ho sebedisa senkgisamonate ho etsa hore mahwafi a se ke a nkga. Mmele e ka nkga hampe ha e sa hlatswe kgafetsa.
Ho nkga ha mmele ho bakwa ke:
- Dikhemikhale tse etswang ke mmele (tse jwalo ka dikhemikhale tse ntshwang ke mmele ho etsa hore motho e mong a kgalle ho etsa thobalano kapa dikhemikhale tsa 'thobalano’ tse hohelang – kapa lelekang – batho ba bang)
- Dintho tseo mmele o lekang ho di ntsha ka ho di hema (tse jwalo ka konofolo le jwala)
- Dintho tse etswang ke baktheria letlalong le diaparong. Letlalo le dula le na le dibaktheria (dikokwanahloko), tse ‘jang’ disele le mofufutso wa letlalo la ntho e shweleng. Tse ding tsa dibaktheria tsena di etsa dikhemikhale tse nkgang hampe.
Ho hlapa le ho itlotsa ka senkgisamonate ho ka fedisa bongata ba dikhemikhale tsena tse nkgang nakwana, empa di ahella hape letsatsi le leng le le leng. Ke ka lebaka leo ho hlapa kamehla ho thusang ho leleka dikokwanahloko le menkgo.
Ho boloka sebaka sa ditho tsa bong se hlwekile ke karolo ya bohlokwa haholo ya bohlweki ba letsatsi le letsatsi.

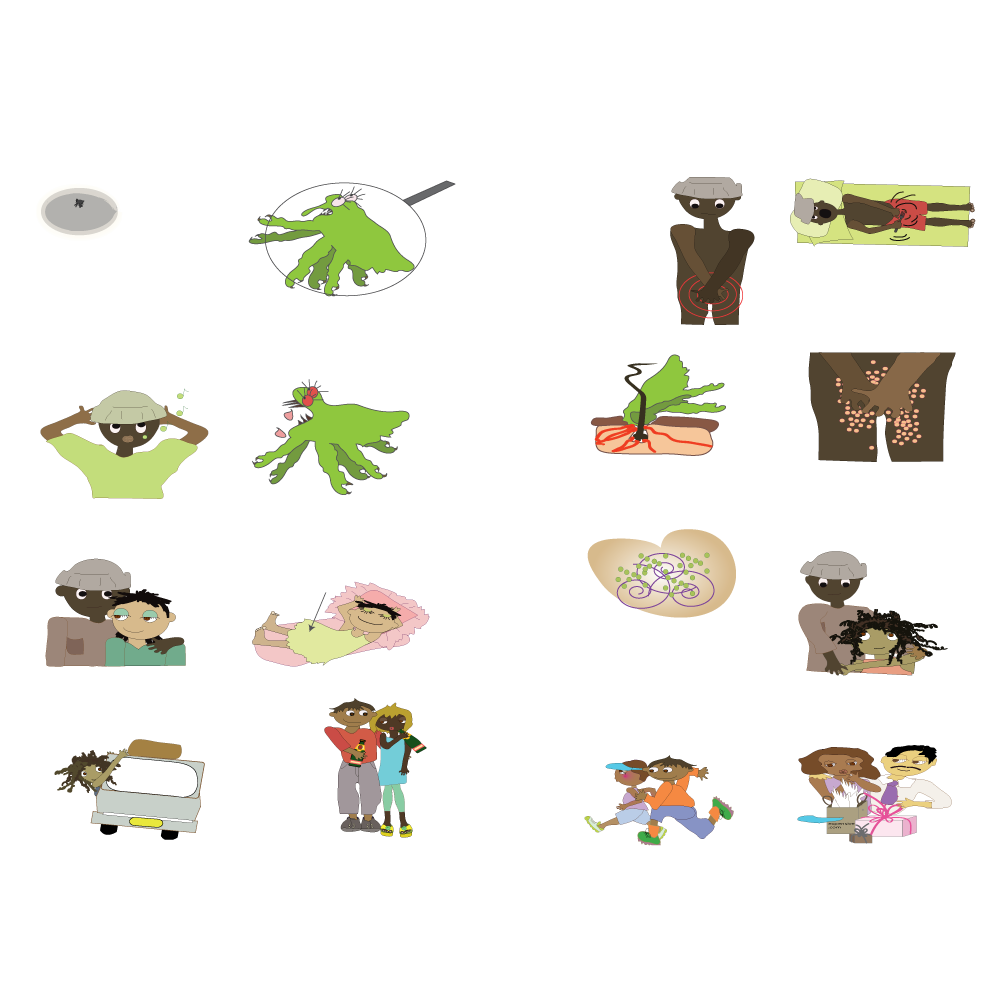
Ena ke Pthirus, nta ya sethong sa botona/botshehadi. E sesanyane haholo - boholo bo ka bang ba letheba la phensele.

Ena ke yona ka tlasa maekroskoupu.
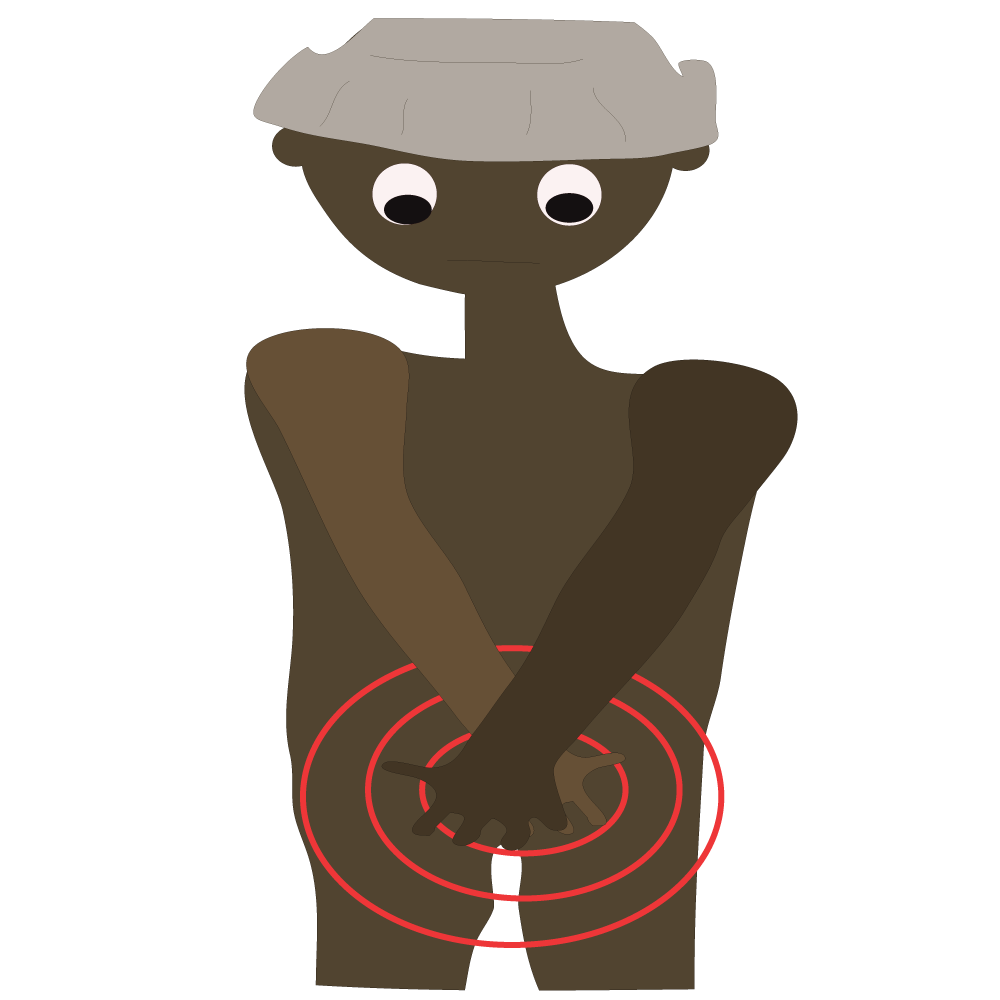
Ha jwale Pthirus e dula le lelapa la yona sebakeng se kantle ho ditho tsa botona/botshehadi sa Porofete. Di behela mahe letsatsi le leng le le leng.
Profete e hlohlona haholo bosiu.

Profete ha e tsebe hore Pthirus e etsa bana le ho ikatisa sebakeng sa yona se kantle ho ditho tsa botona/botshehadi.

Dinta di tshwarwa ke tlala bosiu.
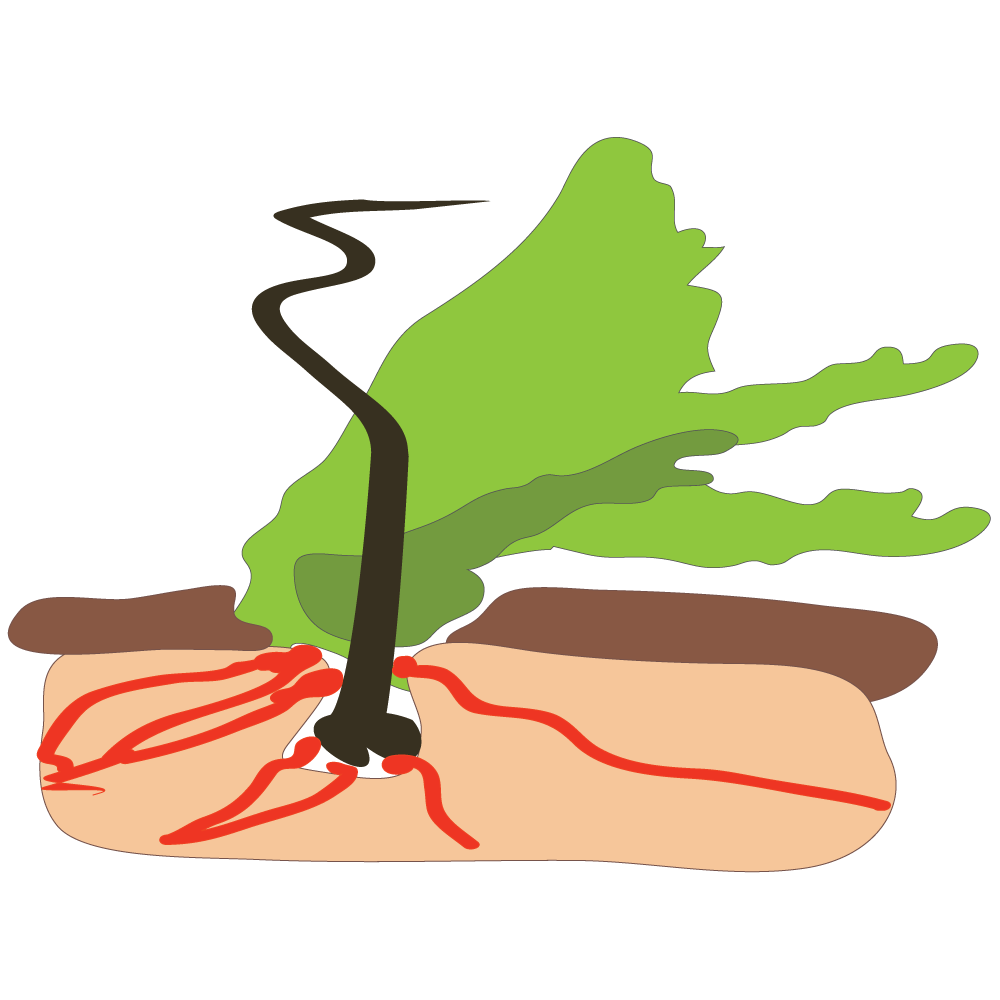
Pthirus e ja mading a ka hara lesobana la boya ba ditho tsa botona/botshehadi.
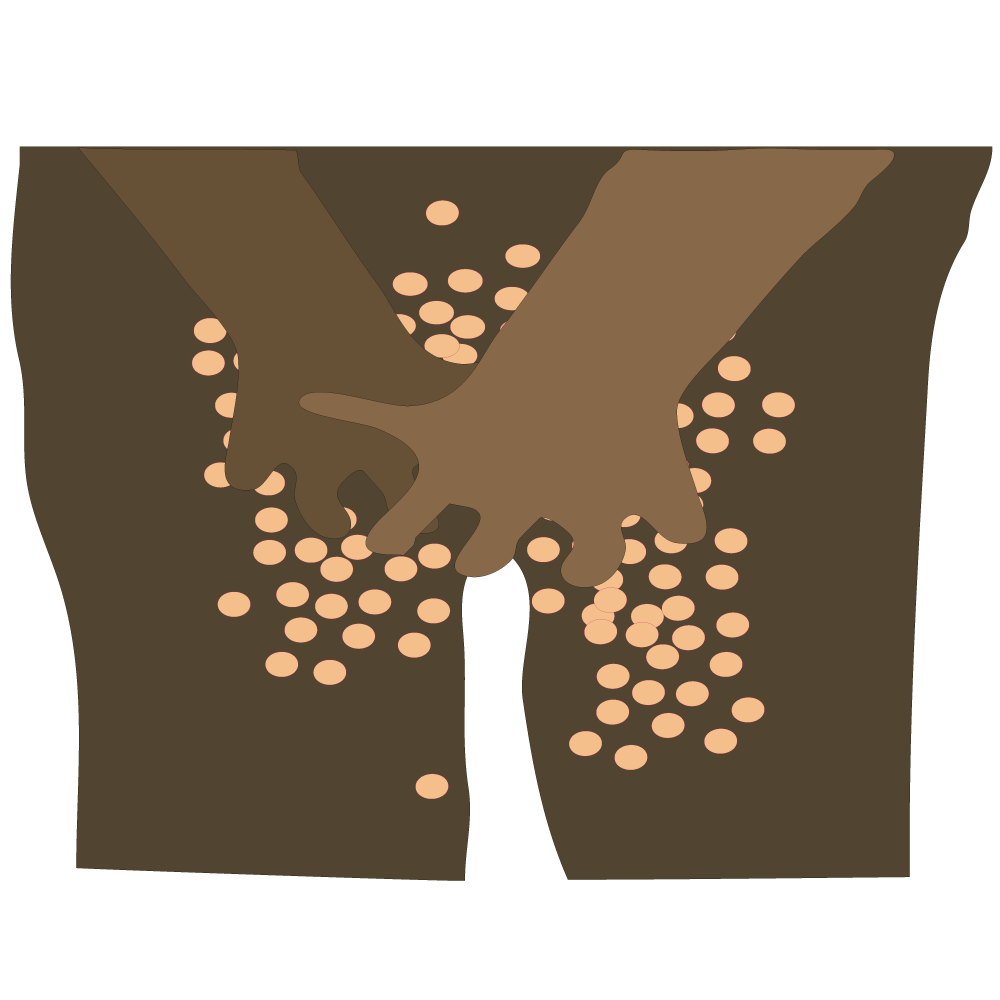
Hona ho ka baka lekgopo.

Jane le Profete ba ne ba ntse ba etsa thobalano dikgwedi tse tsheletseng.

Bana ba seng bakae ba Pthirus ba tlohile ho Profete mme ba behetse mahe sebakeng se ka ntle ho ditho tsa Jane tsa botona/botshehadi.
Mahe ana a tla qhotsa ho ba dinta tsa sebaka se ka ntle ho ditho tsa botona/botshehadi dibekeng tse ka bang tse pedi ho isa ho tse nne.

Ka lehlakoreng le leng - Rose o tla toropong mme o sesa bosiu le Profete. Ke metswalle ya kgale.
Rose o leba lapeng ho mohlankana wa hae Peter (le bapalami ba tlatsetso).

Peter ka dinako tse ding o etsa thobalano le Sibongile, eo e leng mohwebakammele.

Peter o qeta mafelo a beke a na le Zola. Ba ikwetlisa mmoho le ho etsa thobalano ha Rose a tsamaile.

Mohlankana wa Zola ke Kenny. O moholwanyana haholo (mme o na le mosadi le bana).
Pthirus le bana ba Pthirus ba eba le bana le ho nama, ba etsa hore motho a hlohlonelwe kae kapa kae moo a yang!
Ho na le mefuta e fapaneng ya diSTI e arolwang ka dihlopha tse tharo tsa motheo:
- Tse amanang le baktheria - tse bakwang ke baktheria (kokwanahloko)
- Tse amanang le vaesase - tse bakwang ke vaerase
- Tse amanang le fangase (fungus) le tse ding - tse bakwang ke fangase kapa senwamadi kapa protozoa
Maqhanyatsa/dipudula sethong sa botona kapa sa botshehadi, HIV le HPV di bakwa ke vaerase.
DiSTIs tse jwalo ka chlamydia , trichomoniasis (tshwaetso e bakwang ke senwamadi se bitswang trichomonas vaginalis), morotwana (gonorrhoea), mokaola le chancroid (tshwaetso ya diso dithong tsa botona/botshehadi e bakwang ke baktheria e bitswang Haemophilus ducreyi) di ka alafshwa ka katleho ka dianthibayothiki
Ditshwaetso tsa diSTI di ka etsa hore motho a hloke pelehi, e be moimana ya bang le mathata le kankere ya molomo wa popelo, mmoho le ho hlokahallwa ke bana ba sa le banyane haholo le batho ba baholo.
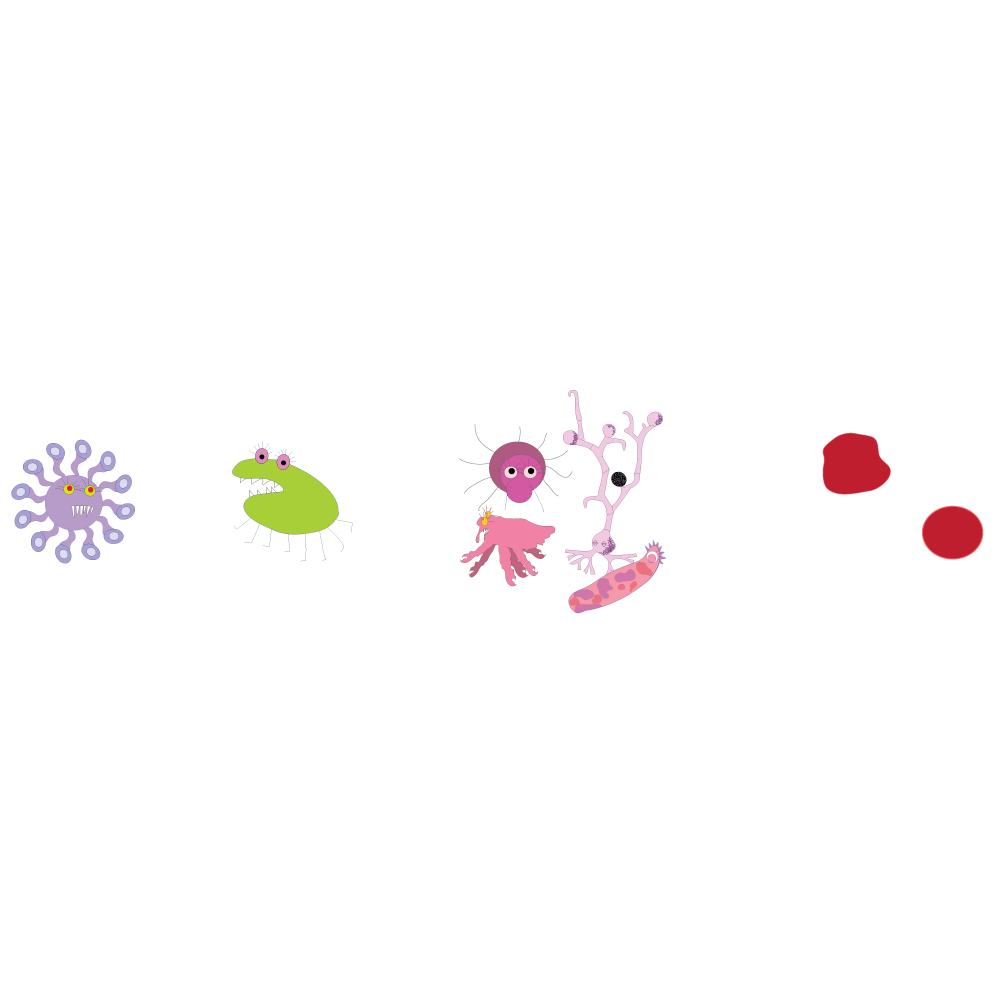
A mang a mabitso a fapaneng a diSTIs: The drop, the itch, morotwana (gonorea), madi a ditshila, mokaola (syphilis), dikokonyana tsa senwamadi karolong ya botona/botshehadi (crabs), HIV, lerothodi la lero le tswang tjhupung ya moroto, maqhanyatsa/dipudula sethong sa botona/botshehadi (herpes), feberu e fetiswang ka ho sunana, the clap (morotwana), VD, cystitis (tshwaetso ya senya).
- Dinta tsa sebaka sa botona/botshehadi (dikokonyana tsa senwamadi karolong ya botona/botshehadi)
- Baktheria e ngata kukung
- Tshwaetso ya baktheria e bitswang Chlamydia trachomatis
- Maqhanyatsa/dipudulana sethong sa botona/botshehadi
- Morotwana.
- Hepathaethis B le C
- HPV - Tshwaetso ya vaerase e bakang dihloba letlalong kapa lereng (Human papillomavirus)
- Tshwaetso ya sebakeng sa ditho tsa botona/botshehadi e bakwang ke baktheria ya Chlamydia
- Lekgopo le hlohlonang le bakwang ke diphehlane tse nyane tse bitswang Sarcoptes scabiei
- Mokaola
- Tshwaetso ya diso dithong tsa botona/botshehadi e bakwang ke baktheria e bitswang Haemophilus ducrei
- PID - Lefu la boruruisi lesapong la noka sebakeng sa setho sa botona/botshehadi
- Tshwaetso e bakwang ke senwamadi se bitswang Trichomonas
- Ditshwaetso tsa Yeast (ha kuku e ruruhile, e le bohloko mme ho na le kgonahalo ya hore e na le tshwaetso)
Ho na le diSTI tsa mefuta e mengata, mme di wela tlasa mekgahlelo e fapaneng.
Boholo ba Ditshwaetso tse Fetiswang ka Thobalano bo tla o ama feela haeba o na le motho eo o etsang thobalano le yena ya nang le STI. Le ha ho le jwalo ho na le ditshwaetso tse itseng, tse kang scabies (lefu la letlalo le tshwaetsanang le bonahalang ka ho hlohlona le ho ba le dibaka tse kgubedu tse ruruhileng) tse bitswang diSTI hobane di fetiswa ka thobalano empa di ka fetiswa le ka ditsela tse ding.
O tla bona hore ke ditshwaetso tse ngata hakae tse se nang matshwao a bonahalang le hore a ka fetisetswa ho wena kapa wena o ka a fetisetsa mothong e mong habobebe hakae.
Ditshwaetso di arotswe ka dihlooho tse tharo tse kgolo:
- Dinwamadi le tse ding
- Baktheria
- Vaerase
Mokgwa o le mong feela o bolokehileng o thibelang 100% ke ho se etse thobalano kahohlehohle, kapa ho ba kamanong ya nako e telele le molekane a le mong, (ho tshepahala 100%) ya tshepahalang.
Lebitso: Dinta tsa sebaka sa botona/botshehadi (dikokonyana tsa senwamadi karolong ya botona/botshehadi)
Mofuta: Senwamadi
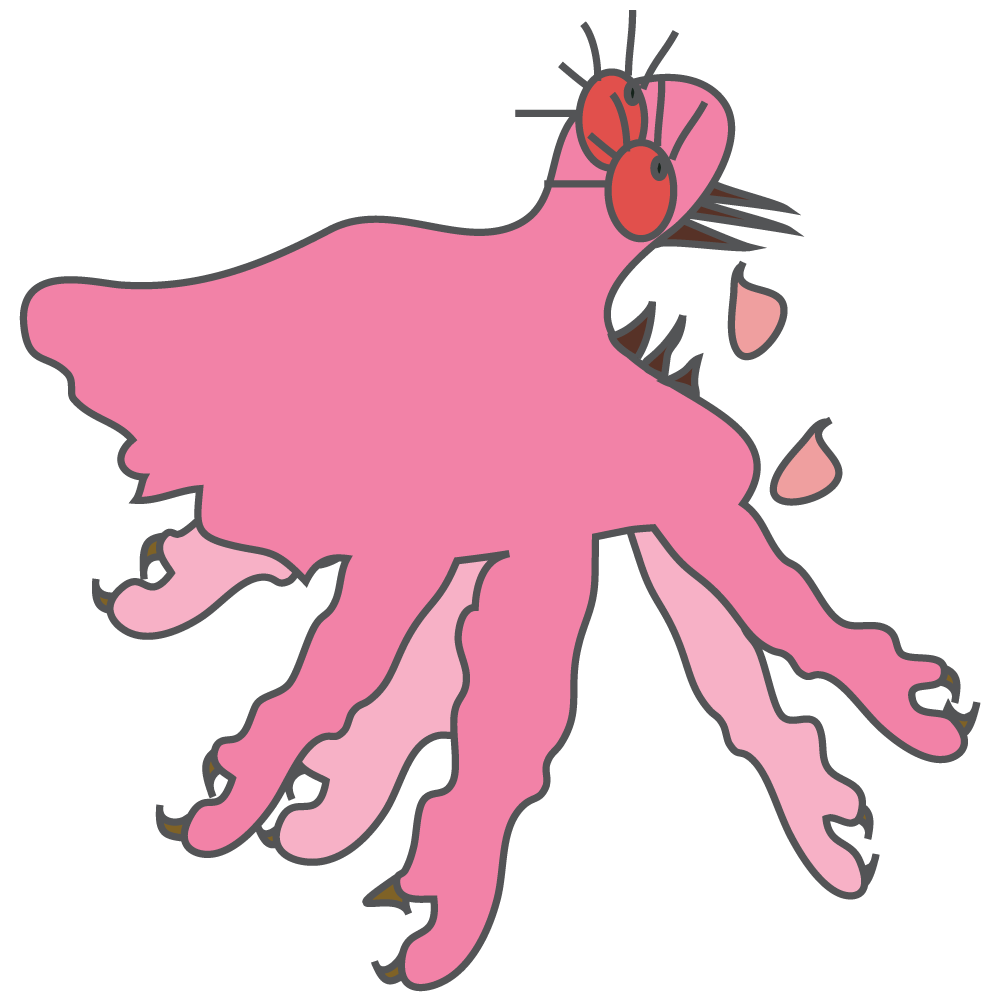
Tlhaloso: Dinwamadi tse nyane tsa sebopeho sa dinta tsa sebaka sa botona/botshehadi tse epang letlalo ho nwa madi. Di phela boyeng bo mahwashe bammele (boo hangata e leng boya ba sebaka sa setho sa botona/botshehadi, empa bo ka fumanwa le boyeng ba mahwafi, sefahleho le dintshi). Di sebedisa dinala tsa tsona tse kang lekgala ho itshwarella moriring.
Sesosa: Di fetiswa ka thobalano, empa di ka fetiswa le ka ho aparelana diaparo, dithaole kapa ho robala le motho ya nang le tsona.
Matshwao: Di phela dikarolong tse nang le moriri tsa mmele. Hangata di bonahala matsatsi a 5 ho isa ho a 7 dibeke ka mora tshwaetso. Ka dinako tse ding mahe a ka bonwa, le dinta di ka bonahala di tsamaya letlalong. Ho hlohlona haholo bosiu. Matheba a makgubedu a hlohlonang kapa lekgopo maqaqailaneng a matsoho, maqaqailaneng, matsohong, dithong tsa botona/botshehadi, sefubeng le mokokotlong.
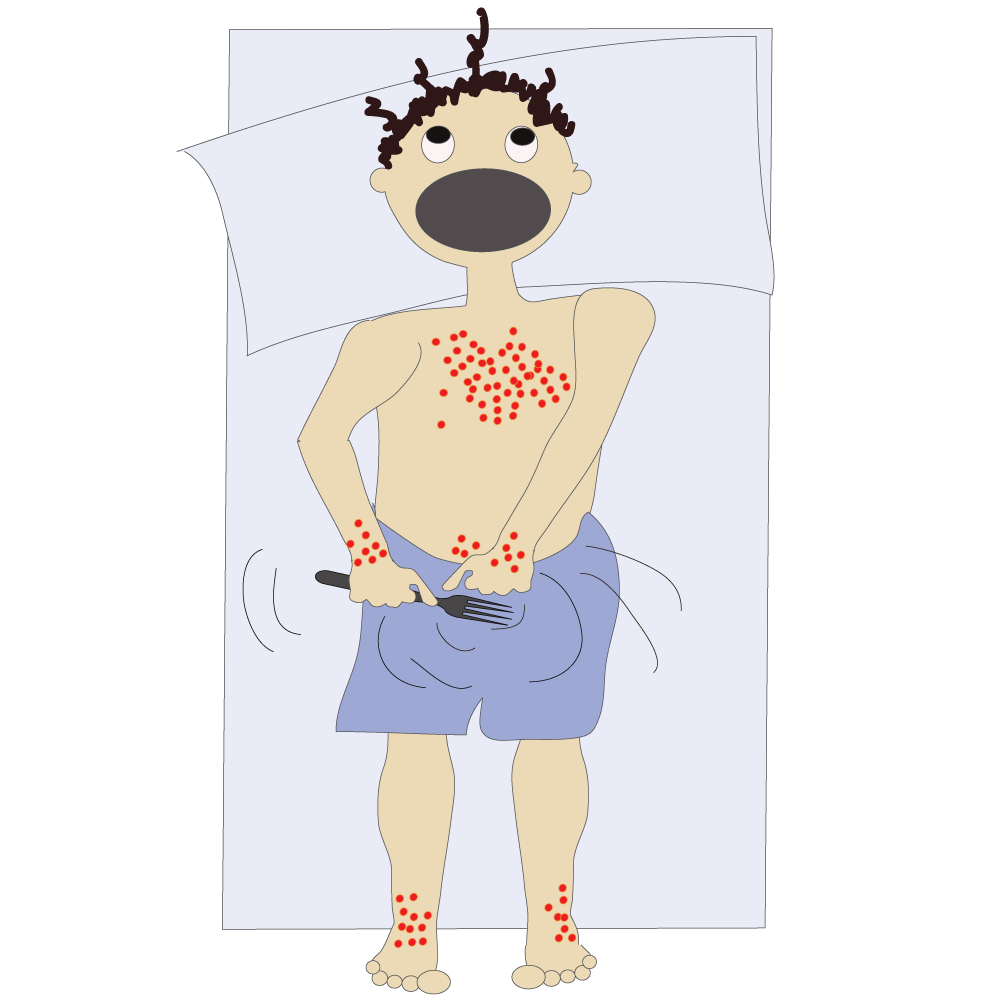
Di a alafeha: E
TThibelo: Ha ho na tsela e sebetsang hantle ka ho hlahisa diphetho tse lebelletsweng ho thibela ho tshwaetswa nakong ya thobalano. Motho ya nang le dikokonyana tsa senwamadi karolong ya botona/botshehadi a ka fokoletsa ba bang kotsi ka ho hlatswa mealo ya bethe, dithaole le diaparo (ka metsi a tjhesang haholo) ho bolaya dinwamadi.
Kalafo: Dishamphu le ditlolo tse ikgethang tse bolayang dinta le mahe a tsona. Ha ho hlokehe hore o kute boya ba sebaka sa ditho tsa botona/botshehadi ka ha hona ho ke ke ha tlosa dinta kaofela. Kalafo e ka hloka ho phetwa haeba mahe kaofela ha a shwa.
LLebitso: Lekgopo le hlohlonang le bakwang ke diphehlane (mites) tse nyane tse bitswang Sarcoptes scabiei (scabies)
Mofuta: Senwamadi
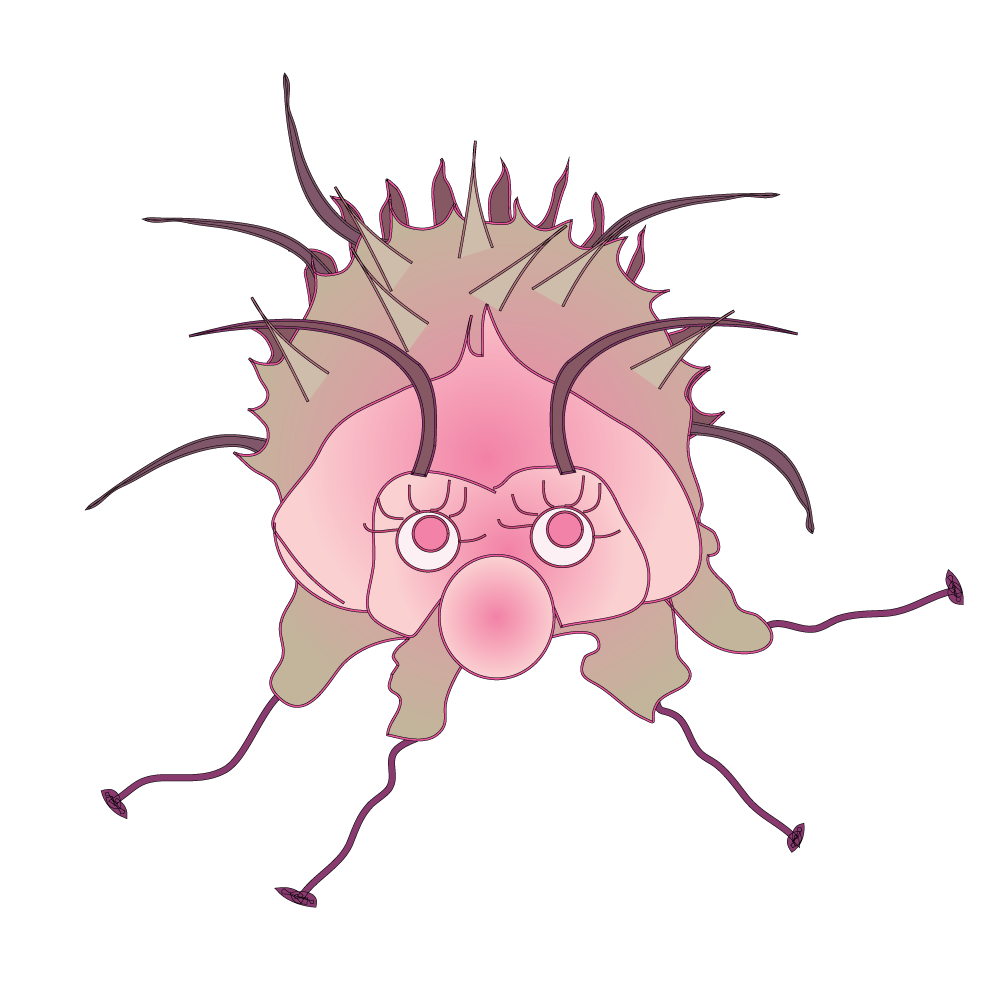
Tlhaloso: Ho kena letlalong ha phehlane ho etsang hore letlalo le hlohlone haholo le ho tshwaetsa . Phehlane e kgolo e tshehadi ha e bonahale ka leihlo la motho, e tona yona e le halofo ya boholo ba e tshehadi. Diphehlane tse tshehadi di epa molalella o ka ntle wa letlalo ho behela mahe.
Sesosa: Le fetiswa ka thobalano empa le ka fetiswa le ka ho kopana ha nako e telele ha matlalo a batho. Le ka nama ka potlako moo batho ba bokellaneng.
Matshwao: Matshwao a qala dibeke tse 2-ho isa ho tse-6 ka mora tshwaetso. Mekoti e bonahala e le mela e sa tsepamang ya bolelele ba (±15mm). Hangata e hlaha pakeng tsa menwana le menwana e metona, dithong tsa botona/botshehadi, ho potoloha mokoteng kapa maraong, setsung kapa maqaqailaneng a letsoho.
Lekgopo le hlohlonang haholo la dipudula tse ruruhileng tse kang dihloba – aleji ya diphehlane, mahe a tsona le mantle a tsona. Ho hlohlona, haholoholo bosiu kapa ka mora ho hlapa ha mmele o futhumetse, e le ho bontsha hore ho na le diphehlane.

LLe a alafeha: E
Thibelo: Ha ho na tsela e sebetsang hantle ka ho hlahisa diphetho tse lebelletsweng ho thibela ho tshwaetswa, ntle le ho tshwarana le motho ya tshwaeditsweng. Motho ya tshwaeditsweng a ka thibela ho nama ka ho hlatswa diaparo le mealo ka metsi a tjhesang haholo ho bolaya diphehlane.

Kalafo: Batho kaofela ba dulang lelapeng le le leng ba lokela ho alafshwa ka ditlolo tse tswang khemising kapa tleleniking.
Lebitso: Trichomoniasis (‘trich’)
Mofuta: Senwamadi
Tlhaloso: STI e tlwaelehileng haholo e bakwang ke senwamadi (Trichomonas Vaginalis). Matshwao a lefu a a fapana empa boholo ba batho ba nang le senwamadi ba ke ke ba tseba hore ba tshwaeditswe.
Sesosa: E Fetiswa ka Thobalano – ya ka kukung, mokoteng, ho momonwa setho sa botona/ botshehadi.
Matshwao: Batho ba tshwaeditsweng ba ka etsang 70% ha ba na matshwao afe kapa afe. Matshwao e ka ba ho longwa hanyane kapa haholo.
Matshwao a mang a matsatsing a 5 – 28 ka mora ho tshwaetswa, empa a mang ha a hlahe ho fihlela ka mora nako. Batho ba se nang matshwao ba ka nna ba fetisa tshwaetso. Matshwao a ka ba teng mme a feela.
Banana ba ka hlohlonelwa, ba utlwa ditho tsa bona tsa bosadi di tjhesa, di na le bokgubedu kapa di le bohloko ha ba rota, ba tswa lero le lesweu, bosehla bo hlakileng, talanyana le nang le monko o sa tlwaelehang.
Teko: tlhahlobo ya mofani wa tlhokomelo ya bophelo le teko ya laboratri.
E a alafeha: E
Thibelo: Dikhondomo tse sebediswang ka nepo nako e nngwe le e nngwe ha ho etswa thobalano, empa ha di thibele ntho e nngwe le e nngwe, mme ho na le kgonahalo ya ho tshwaetswa kapa ho fetisa tshwaetso ena, le ha ho sebediswa khondomo.
E ka etsa hore motho a be le: Monyetla o moholo wa ho pepa lesea pele ho nako ya lona kapa ho beleha lesea la boima bo tlase, le boruruisi ba sebakeng sa ditho tsa botona/botshehadi e bebofatsang monyetla wa ho tshwaetswa ke vaerase ya HIV, kapa ho fetisetsa vaerase ya HIV molekaneng wa thobalano.
Kalafo: Moriana o nowang kapa o tlotswang e le jele – balekane ba thobalano ka bobedi/kaofela.
Lebitso: Tshwaetso ya Yeast (fangase e etsang hore kuku e ruruhe, e be bohloko le ho ba le tshwaetso) – Genital /Vulvovaginal Candidiasis (VVC)
Mofuta: Fangase
Tlhaloso: E le hlahala e holang/namang ho feta tlwaelo.
Sesosa: Boholo ba ditshwaetso bo bakwa ke dintho tse phelang ka hara motho tsa Khandida tse phelang ka molomong, tjhupung e kenyang dijo le ho ntsha tse ditshila le ka kukung ho se na matshwao. Ha ho na le kgaello ya ntho e itseng, e jwalo ka esiti e tlwaelehileng ya diphetoho tsa ka kukung/diphetoho tsa dihomone, Khandida e ka ikatisa le ho eketseha.
E ka fetiswa ho tloha mothong e mong ho ya ho e mong ka thobalano e sa sireletsehang.
Sesosa se seng e ka ba:
- Boimana
- Tswekere
- Anthibayothiksi
- Meriana e thibelang ho ruruha kapa ho tlerefala letlalo
- Mmele o moholo ho feta tekano
Matshwao: Banana hangata ba a hlohlonelwa le ho tjha sethong sa bosadi mme ka dinako tse ding ho ba le lero le tswang kukung le kang tjhisi.
Bashemane ba ka ba le lekgopo le hlohlonang kwaeng/ntotong.
Matshwao a tshwana le a ditshwaetso tse ding tse ngata tsa dithong tsa botona le botshehadi. Hlola le mofani wa hao wa tlhokomelo ya bophelo haeba o na le letshwao lefe kapa lefe la matshwao ana.

E a alafeha: E
Thibelo: Dikhondomo tse sebediswang ka nepo lekgetlo le leng le le leng ha o etsa thobalano. Ho apara diaparo tsa ka hare tse thetsanang le letlalo tsa mofuta wa khothene ho ka thusa ho fokotsa kotsi. Haeba o na le ditshwaetso tse ngata, mofani wa hao wa tlhokomelo ya bophelo a ka laela hore o fumane meriana e meng.
Kalafo: Setlolo le/kapa pidisi balekane ka bobedi/kaofela. Etsa hore sebaka sa ditho tsa botona/botshehadi se dula se omme mme se hlwekile.
Lebitso: Bacterial Vaginosis (BV)
Mofuta: Baktheria
Tlhaloso: Ha tekano e tlwaelehileng ya baktheria e ka hara kuku e sitiseha mme ho ba le baktheria e itseng e kgolohadi sebakeng sa yona.
Sesosa:
- Ho se lekalekane ha baktheria e tlwaelehileng ya ka kukung
- Molekane e motjha /balekane ba bangata ba thobalano
- Ho sebedisa sethibelapelehi se kengwang ka hara popelo (IUD)
Matshwao:
- Banana ba bang ha ba na matshwao
- Banana ba eso etse thobalano ba ka ba le BV
- E tlwaelehile nakong ya boimana
- Lero le tswang kukung, monko, lehlaba, ho hlohlona kapa ho tjha

Thibelo: Ditsebi tsa saense ha di utlwisise BV hantle mme ditsela tse loketseng ka ho fetisisa tsa ho e thibela ha di tsejwe. Le ha ho le jwalo, ho a tsebahala hore BV e amana le ho ba le molekane e motjha kapa ba bangata ba thobalano.
Dikgato tse latelang tsa thibelo ya motheo di ka thusa ho fokotsa kotsi ya ho sitisa tekano ya tlhaho ya baktheria ya ka hara kuku:
- Se etse thobalano
- Beha moedi palong ya balekane ba thobalano
- O se hlatswe kuku ka hare ka metsi kapa metswako ya mekedikedi e fedisang monkgo
Kalafo: BV e alafeha ka anthibayothiksi eo mofani wa tlhokomelo ya bophelo a fanang ka yona. Sebedisa meriana kaofela eo o e filweng le ha matshwao a feela.
E a alafeha: E
HPV e ka etsa hore:
- diSTI tse ding tse kenyeletsang HIV, Maqhanyatsa/dipudula sethong sa botona/botshehadi, Morotwana
- PID - Lefu la boruruisi lesapong la noka le sebakeng sa setho sa botona/botshehadi ka mora ho ntsha popelo kapa mpa
- mathata a mangata a boimana le lesea le hlahang le na le boima bo tlase
- kotsi ditjhupung tsa fallopian, ho eketsang kotsi ya ho hloka pelehi kapa ho ima lesea le holelang ka ntle ho popelo (boemo bo ka nkang bophelo ba motho moo lehe le nontshitsweng le holelang kantle ho popelo)
Lebitso: Chlamydia
Mofuta: wa Baktheria
Tlhaloso: Chlamydia ke STI e tlwaelehileng e bakwang ke dibaktheria tsa Chlamydia Trachomatis, tse ka bakang kotsi dithong tsa ngwanana tsa ho etsa bana.
Sesosa: Thobalano ya ka kukung, mokoteng kapa ho momonwa setho sa botona kapa sa botshehadi.

Matshwao: Hangata ha se a mabe haholo kapa ha a be teng ho hang empa ha a ka ba teng – a ba teng beke e le 1 ho isa ho tse 3 ka mora ho bonahala.
Banana:
- Lero la kuku
- Ho tjheswa ke moroto
- Ho ba le lehlaba tlase mpeng
- Ho ba le lehlaba tlase mokokotlong
- Ho feroha dibete le feberu
- Ho utlwa bohloko nakong ya thobalano
- Ho tswa madi a mangata pakeng tsa dinako tsa ho ya matsatsing/kgweding
- Tshwaetso ya Chlamydia ya molomo wa popelo e ka namela mokoteng
Bashemane:
- Lero le tswang kwaeng/ntotong
- Ho utlwa bohloko ha ba rota
Thibelo: Dikhondomo tsa banna, tse sebediswang ka tsela e tshwanang kamehla le ka nepo, di ka fokotsa kotsi ya ho fetisa Chlamydia.
Kalafo le ho etsa diteko: Anthibayothiksi. Bashemane le banana ka bobedi ba lokela ho etswa diteko hape dikgwedi tse ka bang tse tharo ka mora kalafo ya tshwaetso ya pele, le ha ba dumela hore balekane ba bona ba thobalano ba alafilwe. Ho etsa diteko ka moroto kapa swapo.
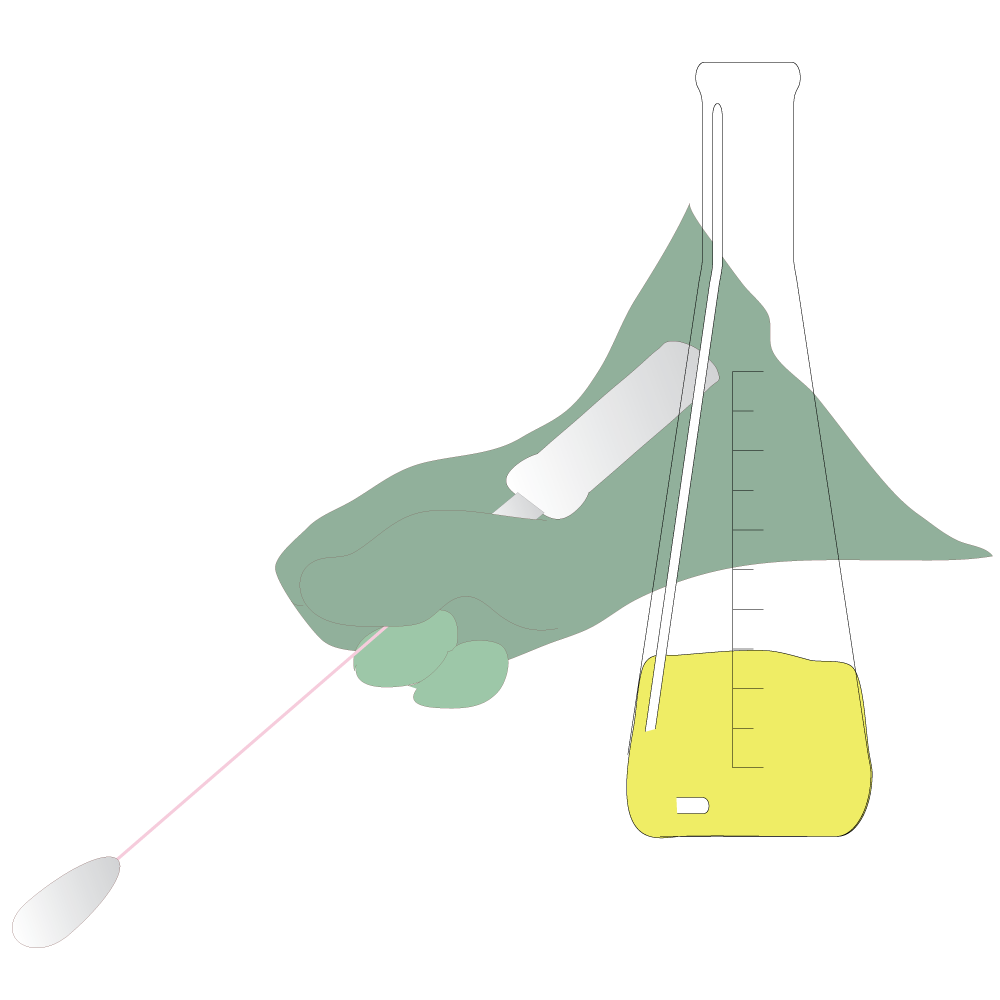
E a alafeha: E
HPV e ka etsa hore:
- Ho be le mathata a kotsi haholo le a moshwelella a bophelo
- Lefu la Boruruisi Lesapong la noka le sebakeng sa setho sa botona/botshehadi Bananeng (PID)
- Mathata a ka baka kotsi e ke keng ya hlola e phekoleha, e kenyeletsang ho hloka pelehi ho ka etsahalang ‘ho sa bontshe’ pele ngwanana a lemoha bothata
- Nyumonia le conjunthivaethisi (Ho tlerefala le ho ruruha karolo e tshweu ya leihlo) maseeng a sa tswa belehwa ho tlwaelehile
Lebitso: Morotwana (Gonorea)
Mofuta: wa Baktheria
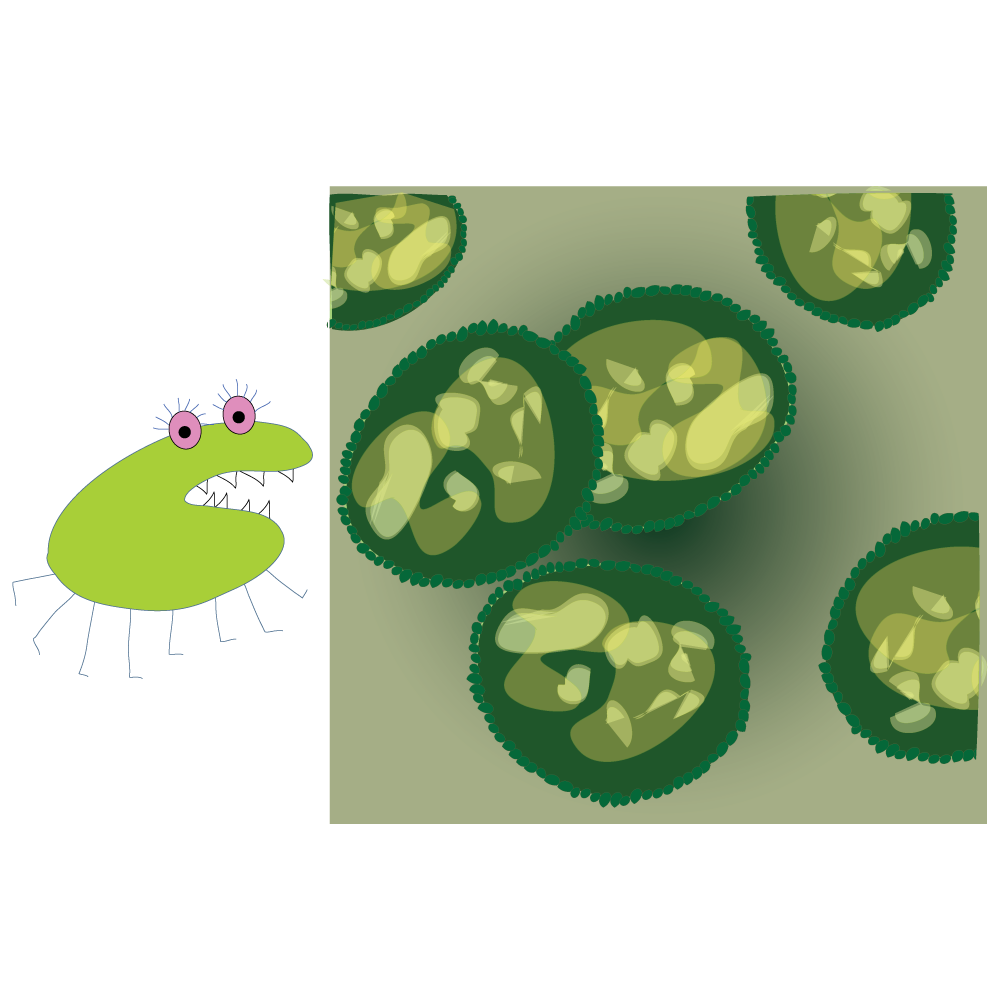
Tlhaloso: Morotwana o bakwa ke Neisseria Gonorrhoeae, baktheria e kgonang ho hola le ho ikatisa ha bobebe dibakeng tse futhumetseng, tse mongobo tsa motjha wa dikarolo tsa ho etsa bana, tse kenyeletsang:
- molomo wa popelo, popelo le ditjhupu tsa fallopian bananeng,
- urethra (tjhupu ya moroto) bananeng le bashemaneng.
Baktheria ena e ka hlaha le ka molomong, mmetsong, mahlong le ka maraong.
Sesosa: Thobalano ya ka kukung, ka maraong kapa ho momonwa ha setho sa botona kapa sa botshehadi
Matshwao:
Bong ka bobedi:
- Ho ka nna ha se be le matshwao, kapa a ka se be mabe haholo
- Lero le letenya le lesehla le tswang kwaeng/kukung, ho utlwa bohloko ha moroto o tswa le/kapa nakong ya thobalano
- Ho hlohlonelwa ka maraong
- Ho ba bohloko
- Mantle a tswang habohloko
- Mmetso o bohloko
Bananeng:
- Ho tswa madi a mangata pakeng tsa dinako tsa ho ya matsatsing/kgweding
Bashemaneng:
- Makwalata/ditapole tse ruruhileng kapa tse bohloko
Thibelo:
- Ho se etse thobalano
- Dikhondomo tse sebediswang ka tsela e tshwanang kamehla le ka nepo di ka fokotsa kotsi ya ho fetisa tshwaetso

Ho etsa diteko le Kalafo: Teko ya moroto e ka sebedisetswa ho etsa diteko ntle le ha motho a entse thobalano ya ka maraong/ho momonwa setho sa botona/ botshehadi, e leng moo ho tla nkwa diswapo.
Alafeha: E, empa kalafo e ke ke ya lokisa tshenyo e seng e entswe.
HPV e ka etsa hore:
- Ho be le mathata a kotsi haholo a ka bakang tshenyo e ke keng ya kgutlisetswa morao e kenyeletsang ho hloka pelehi ho ka etsahalang 'ho sa bontshe' pele ho lemohwa bothata.
- Kotsi e eketsehileng ya ho ima lesea le holelang ka ntle ho popelo.
- Ho tshwaetsa lesea haeba ngwanana a imile.
- Nyumonia le conjunthivaethisi (Ho tlerefala le ho ruruha karolo e tshweu ya leihlo) maseeng a sa tswa belehwa ho tlwaelehile.
- E ka namela popelong kapa ditjhupung tsa fallopian mme ya baka Lefu la boruruisi lesapong la noka sebakeng sa setho sa botona/botshehadi (PID).
- E ka namela mading le manonyeletsong haeba e sa phekolwe – hona ho ka ba le kgonahalo ya ho nka bophelo ba motho.
- Kotsi e eketsehileng ya ho ba le HIV kapa ho e fetisetsa mothong e mong.
- Bashemaneng – ho ka ba le bohloko bo bitswang Epididymitis ditjhupung tse ka mora makwalata/ditapole. E ka etsa hore moshemane a hloke pelehi (a se kgone ho ba ntate ya nang le bana).
Lebitso: Mokaola (Syphilis)
Mofuta: wa Baktheria
Tlhaloso: Mokaola ke baktheria ya STI e ka bakang mathata a nako e telele le/kapa ho hlokahala haeba e sa phekolwe ka tshwanelo.
Sesosa: Thobalano ya ka kukung, maraong kapa ho momonwa setho sa botona kapa sa botshehadi ka ho tobana le diso tsa mokaola. Banana ba imileng ba ka e fetisetsa baneng ba bona ba eso belehwe.
Matshwao: Diso (tseo hangata di leng thata, tse tjhitja le tse seng bohloko) tse hlahang haholo kantle ho ditho tsa botona/botshehadi, kukung, ka maraong, mokoteng, dipounameng le ka molomong. Nako e mahareng a ho tshwaetswa ke mokaola le ho bonahala ha letshwao la pele ke matsatsi a 21 empa e ka ba ho tloha matsatsing a 10 ho isa ho a 90.
Mokaola o na le mehato e 4:
- Mohato wa Mantlha: di/seso sa pele se hlaha moo mokaola o keneng mmeleng. Seso ha se bohloko kahoo se ka nna sa se bonahale. Se ba teng dibeke tse 3 ho isa ho tse 6 mme se fola ka kalafo kapa kantle le kalafo. Ngwanana wa moimana ya nang le mokaola a ka ba le mathata a mangata a bophelo, a ka ba le boima bo tlase ha a hlaha, a ka hlaha pele ho nako kapa a hlaha a hlokahetse.
- Mohato wa Bobedi: makgopo a letlalo karolong e le nngwe kapa tse ngata tsa mmele le/kapa diso ka molomong, kukung kapa ka maraong. Lekgopo ha le hlohlone mme le ka nna la se bonahale. Maqeba a maholo, a ruruhileng, a maputswa kapa a masweu a ka hlaha ka molomong, ka mahwafing kapa nokeng.
Matshwao a mang a kenyeletsa:
- Feberu
- Ditho tse ruruhileng tsa mmele tse ntshang mokedikedi o mongata haholo dithishung le diseleng
- Mmetso o bohloko
- Ho ba le dibaka tse se nang moriri
- Ho opelwa ke hlooho
- Ho theoha mmeleng
- Ho opelwa ke mesifa
- Mokgathala
- Condylomas (maqeba a kang dihloba)
Matshwao a tla feela ka kalafo kapa ntle le kalafo. Ha a sa alafshwe, tshwaetso e tla qetella e se na matla mme a ke ke a kgona ho ba mohatong wa ho qetela.
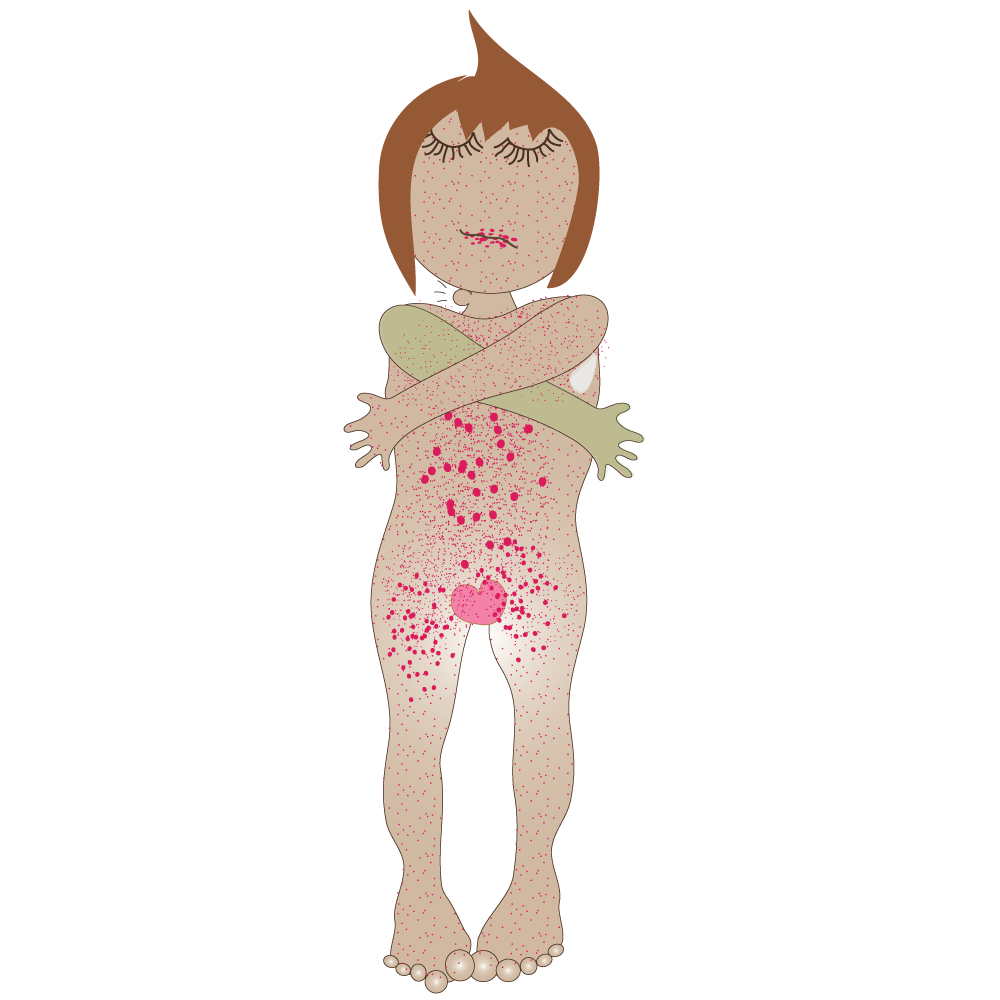
Mohato o se nang Matla (o patehileng): matshwao a mohato wa mantlha le wa bobedi a a feela. Kantle le kalafo ha ho na matshwao, empa Mokaola o dula o le mmeleng. Mohato ona o se nang matla o ka ba mmeleng dilemo.
Mohato wa moraorao: Matshwao a ka hlaha dilemo tse 10 – 30 ka mora tshwaetso mme a kenyeletsa:
- Bothata ba ho tsamaisa mesifa
- Kgolofalo
- Ho shwa bohatsu
- Ho foufala hanyane-hanyane
- Bolebadi
- Lefu le kowafatsa ditho tsa ka hare tse kenyeletsang booko, methapokutlo, mahlo, pelo, methapo ya madi, sebete, masapo le manonyeletso. Bokowa bona bo ka etsa hore motho a hlokahale.
Thibelo: Mokgwa o le mong feela o bolokehileng o thibelang 100% ke ho qoba ho etsa thobalano, kapa ho dumellana le molekane wa kamano ya nako e telele ya tshepahalang ya entsweng diteko le ho tsebahala hore ha a tshwaetswa, hore le be kamanong ya lerato le le bang feela. Dikhondomo ha di sireletse kamehla - ho tshwara seso ka ntle ho karolo e kwahetsweng ke khondomo ho ntse ho ka baka tshwaetso.
Diso tsa mokaola wa ka hanong, maraong, kukung kapa kwaeng/ntotong di bebofatsa ho fetiswa le ho fumana tshwaetso ya HIV. O na le kgonahalo ya makgetlo a 2 ho isa ho a 5 ya ho fumana HIV haeba o bile le motho ya nang le diso tsa mokaola.
Hopola: diso di ka ipata le ka kukung, ka maraong, tlasa letlalo le ka pele kwaeng/ntotong kapa molomong.
Diteko: Hangata ke teko ya madi.
Ngwanana e mong le e mong ya imileng o lokela ho etswa teko ya mokaola nakong ya boimana le ha a beleha, hobane mokaola o sa alafshwang o ka tshwaetsa le ho bolaya lesea le holang.
Kalafo: Hangata mokaola o alafeha ha bobebe ka dianthibayothiksi. Kalafo e tla bolaya mokaola le ho thibela tshenyo e fetang e seng e le teng, empa e ke ke ya e lokisa.
E ka etsa hore ho be le: Sheba mehato ya mokaola.
Lebitso: Tshwaetso ya sebakeng sa ditho tsa botona/botshehadi e bakwang ke baktheria ya Chlamydia (Lymphogranuloma (LGV)
Mofuta: Baktheria
Tlhaloso: LGV ke tshwaetso e bakwang ke mefuta ya dibaktheria tsa Chlamydia Trachomatis (tse sa tshwaneng le chlamydia)
Sesosa: Thobalano e tobileng ditho tsa botona/botshehadi, mokoteng kapa molomong. E tlwaelehile haholo BTB (banna ba etsang thobalano le banna).
Matshwao: E ka qala matsatsi a seng makae ho isa ho kgwedi ka mora ho tshwaetswa ke baktheria.
Matshwao a ka kenyeletsa:
- Dihloba/matswabadi dithong tsa botona /motjheng wa setho sa botshehadi a folang kapele a sa siye mabadi.
- Madi kapa boladu bo tswang ka mokoteng (madi mantleng).
- Mantle a tswang habohloko.
- Diso tse nyane tse seng bohloko.
- Ho ruruha le ho tlerefala letlalo sebakeng sa noka.
- Ho ruruha malebe.
- Leqhutsu la noka le ruruhileng ho potoloha karolo ya mokoteng bathong ba etsang thobalano ya ka maraong.
- Letshollo le lehlaba tlase mpeng.
Thibelo: Qoba ho ba haufi le ditho tsa botona/botshehadi, mokoteng kapa molomo wa motho ya tshwaeditsweng. Hopola, Ha ho na matshwao a bonahalang.
Kalafo: E alafeha ka dianthibayothiksi. Ho ntshwa ha boladu ka ho hlajwa ka nalete.
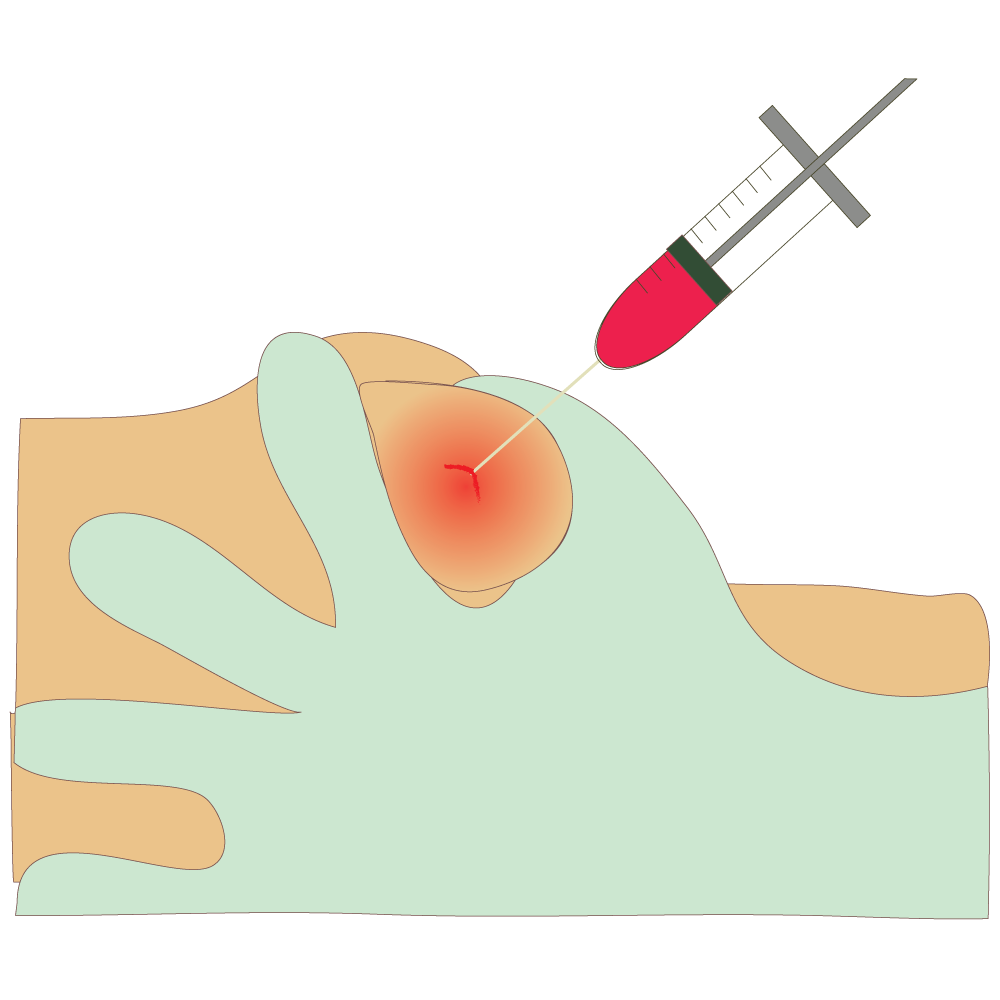
Haeba e sa alafshwe e ka etsa hore:
- Masea a hlahang a be le lefu leo a le fumanang ho mme ya tshwaeditsweng ha a beleha.
- Ho kopana ho sa tlwaelehang ho pakeng tsa karolo ya mokoteng le kuku.
- Ho ruruha booko (ha ho a tlwaeleha haholo).
- Ditshwaetso manonyeletsong, mahlong, pelong kapa sebeteng.
- Ho ruruha ha ditho tsa botona/botshehadi nako e telele.
- Ho taboha le ho ba ho sesanyane karolong ya mokoteng.
- Mathata a ka hlaha dilemo tse ngata ka mora hoba o qale ho tshwaetswa.
Lebitso: Tshwaetso ya diso dithong tsa botona/botshehadi e bakwang ke baktheria e bitswang Haemophilus ducreyi (Chancroid)
Mofuta: Baktheria
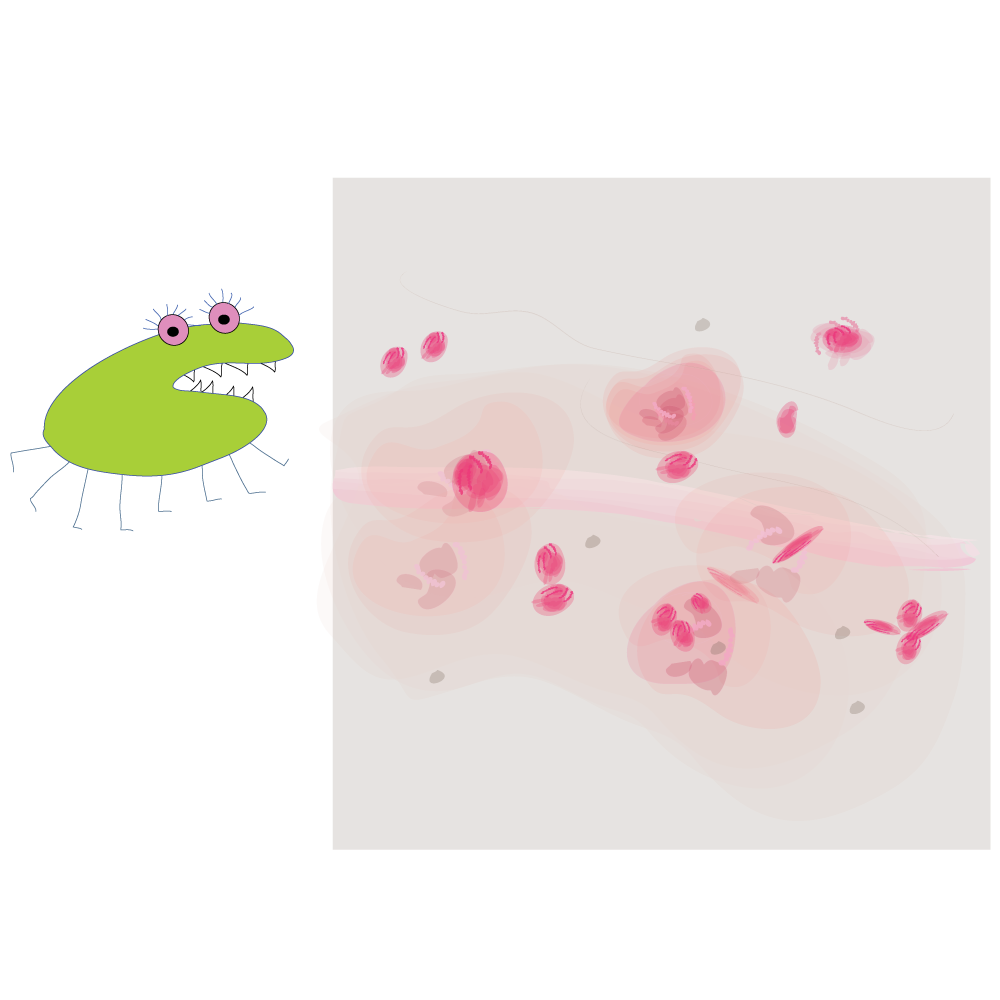
Tlhaloso: Chancroid ke STI e bakwang ke dibaktheria. E tlwaelehile dinaheng tse futhumetseng le tse mongobo empa e seng haholo dikarolong tse ding tsa lefatshe.
Sesosa: Ho etsa thobalano le motho ya tshwaeditsweng. Haholo ha motho a sa tlwaela bophelo bo hlwekileng, le ha motho e motona a sa bolotsa.
Matshwao: Hangata ke seso se le seng kapa tse ngata kapa marao a nang le dikuru a potapotilweng ke bokgubedu karolong ya botona/botshehadi, matsatsi a 4 ho isa ho a 7 ka mora ho tshwaetswa.
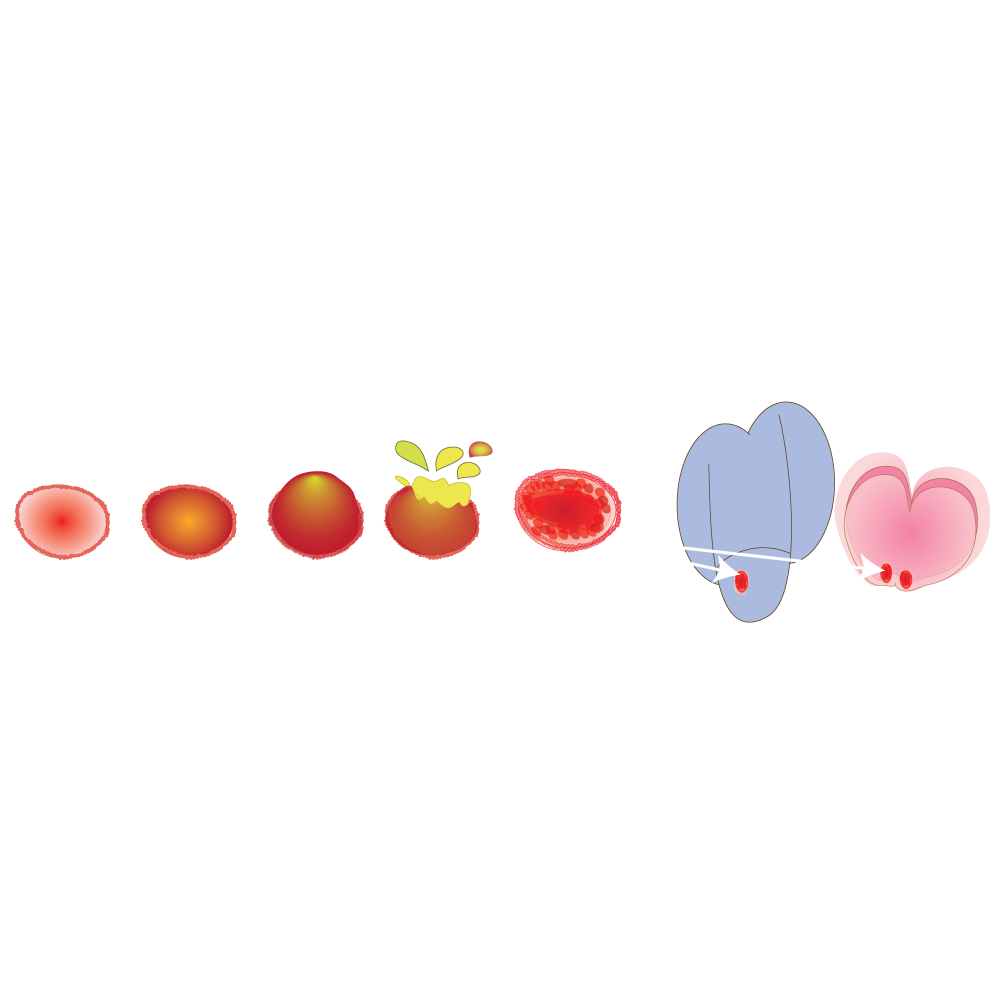
SHaufinyana diso di ba le boladu mme di a phunyeha, di siya diso tse bulehileng tse bohloko. Palong e ka etsang halofo ya diketsahalo ditshwelesa tsa noka di ba kgolwanyana, di ba thata, le ho ba bohloko, di ba bonojana, dikuru tse ka qetellang di phunyehile.
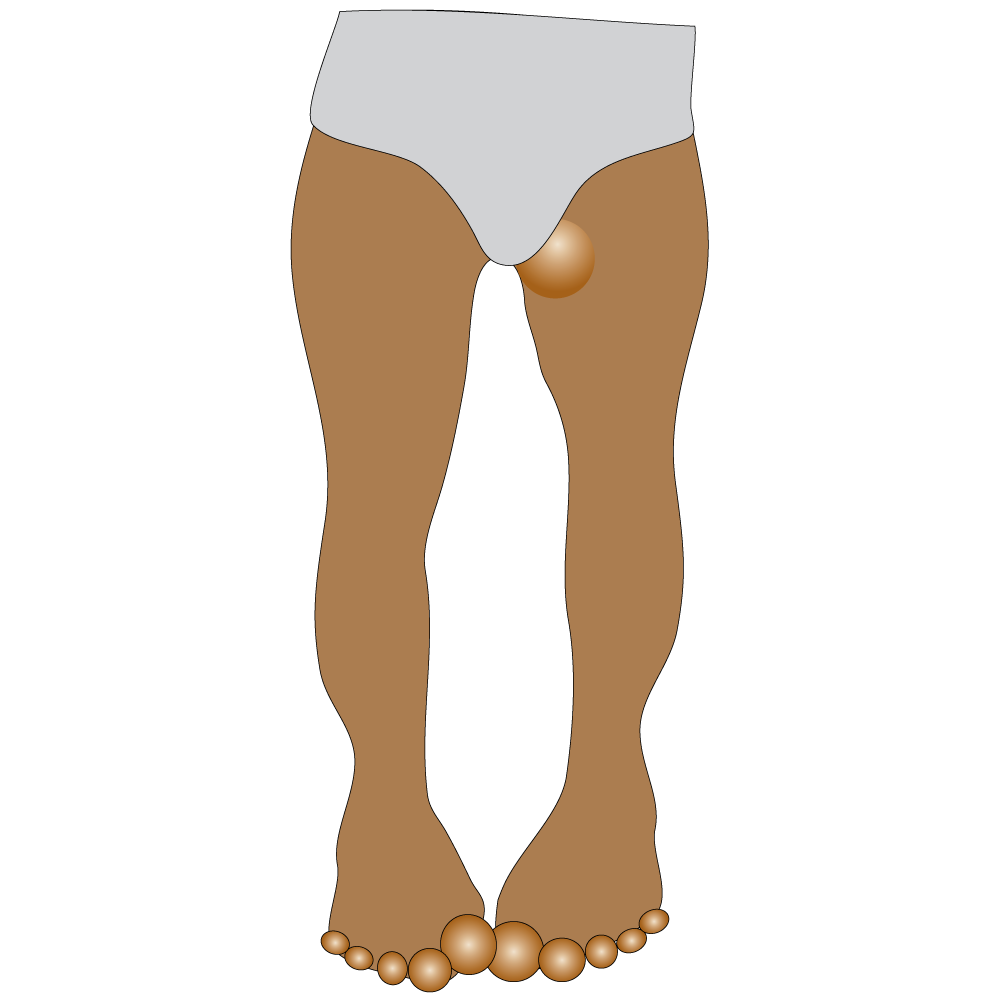
Thibelo: Mokgwa o le mong feela o bolokehileng o thibelang 100% ke ho qoba ho etsa thobalano, kapa ho dumellana le molekane ya tshepahalang ya entsweng diteko le ho tsebahala hore ha a tshwaetswa, hore le be kamanong ya lerato le le bang feela.
Dikhondomo ha di sireletse kamehla. Ho thetsa seso ka ntle ho karolo e kwahetsweng ke khondomo ho ntse ho ka baka tshwaetso.
Haeba o nahana hore o tshwaeditswe, qoba ho etsa thobalano efe kapa efe mme o hlahlojwe. Tsebisa balekane kaofela hore ba hlahlojwe.
Kalafo: Dianthibayothiksi di tla fodisa Chancroid (maqeba le mathopa a fola dibekeng tse pedi).
E ka etsa hore motho a be le: mathopa dithong tsa botona/botshehadi a ka bang teng dibeke kapa dikgwedi haeba a sa alafshwe. Kotsi ya ho fumana HIV.
Lebitso: Hepathaethis B
Mofuta: E bakwa ke vaerase
Tlhaloso: Hephathaethis B ke lefu le tshwaetsang la sebete le bakwang ke vaerase ya Hephathaethis B. E ka fetiswa le ka ho ba haufi le motho ya nang le yona le sa etse thobalano.
Sesosa:
- Ho tshwara lero la mmele o tshwaeditsweng ke hephathaethis (lero la thobalano, madi, mathe).
- Ka leqeba kapa sebaka se nang le mamina (leihlo).
- Ho etsa thobalano.
- Ho itlhaba ka dinalete tsa dithethefatsi le ho di sebedisa le batho ba bang.
- Ho fetisa ho tloha ho mme ho ya ngwaneng nakong ya peleho.
- Ho sebedisa mahare kapa maborashe a meno le motho ya tshwaeditsweng.
Matshwao: Matshwao a ka feela a sa bonahale.
Ha a le teng, a ka kenyeletsa:
- Feberu
- Mokgathala
- ho se be le takatso ya dijo
- ho feroha dibete
- ho hlatsa
- ho ba le lehlaba mpeng
- moroto o fifetseng
- mantle a mmala wa letsopa
- ho ba le lehlaba manonyeletsong
- jondisi – letlalo le sehlefetseng le mahlo a masweu.
Thibelo: Qoba ho tshwara lero la mmele (madi, lero la thobalano, mathe) a motho ya tshwaeditsweng.
Vaerase e ka phela kantle ho mmele matsatsi a fetang a 7 mme ya nna ya tshwaetsa.
Kalafo: Bakeng sa tshwaetso e mpe haholo, moriana ha o fumanehe, kalafo e a tshehetsa. Bakeng sa tshwaetso e dulang nako e telele, meriana e thibelang divaerase. Batho ba nang le tshwaetso e nkang nako e telele ya HBV ba hloka tlhahlobo ya bongaka le ho behwa leihlo kamehla.
HPV e ka etsa hore:
- Hephathaethis e nkang nako e telele e sa fole.
- Cirrhosisi (ho siya mabadi) sebeteng kapa kankere ya sebete.
Lebitso: Human Papillomavirus (HPV)
Mofuta: Vaerase
Tlhaloso: HPV ke STI e tlwaelehileng haholo e tshwaetsanang, e nang le mefuta e fetang e 40 e ka tshwaetsang molomo/mmetso le dibaka tsa ditho tsa botona le tsa botshehadi.
Sesosa:
- Thobalano ya ka kukung, mokoteng kapa ho momonwa setho sa botona kapa sa botshehadi.
- HPV e ka hlaha dilemo tse ngata ka mora hoba e o tshwaetse.
- O ka tshwaetswa ke mofuta o fetang o le mong wa HPV.
- Masea a ka tshwaetswa ha a belehwa.
Matshwao: Boholo ba batho ba nang le HPV ha bo be le matshwao kapa mathata a bophelo empa bo ntse bo kgona ho fetisa vaerase ntle le matshwao.
Masole a mmele kamehla a ntsha HPV nakong ya dilemo tse pedi. Haeba ho se jwalo, dihloba tse karolong ya botona/botshehadi di hlaha e le kuru e nyane kapa sehlopha sa dikuru karolong ya botona/botshehadi. Di ka ba nyane kapa tsa ba kgolo, tsa ruruha, tsa rapama kapa tsa bopeha jwalo ka kholifolawa.
Thibelo:
- Tsela e le nngwe eo ho nang le bonnete ba ho thibela HPV ka yona ke ho se etse thobalano.
- Dikhondomo di ka nna tsa se fane ka tshireletso e felletseng ka ha HPV e ka kgona ho tshwaetsa dikarolo tse sa kwahelwang.
- Diente di ka sireletsa batho ba batona le ba batshehadi hore ba se tshwaetswe ke e meng ya mefuta e tlwaelehileng ya HPV e ka etsang hore ba be le lefu le itseng kapa kankere. Ho bohlokwa hore o fumane ditekanyetso tse tharo hore o sireletsehe ka ho phethahala.
- Ho hlahlobela kankere ya molomo wa popelo kamehla ho fumana matshwao a qalang a lefu le kalafo ho thibela kankere hore e be teng. Dikankere tse ding tse amanang le HPV di ka nna tsa se be le matshwao ho fihlela di le boemong boo ho leng boima ho di alafa.
Kalafo: Motho a ka itlosa dihloba tse bonahalang karolong ya setho sa botona/botshehadi ka meriana e laetsweng ke ngaka kapa a ka alafshwa ke mofani wa tlhokomelo ya bophelo.
HPV e ka etsa hore: Disele tse tlwaelehileng di fetohe ho ba tse sa tlwaelehang ka sebopeho sa dihloba tse bonahalang karolong ya setho sa botona/botshehadi kapa kankere. Tsena di ka kenyeletsa dikankere tsa molomo wa popelo, valva, kwae/ntoto, mokoteng le mmetso.
Haeba di tlohelwa di sa alafshwe, dihloba tse bonahalang karolong ya setho sa botona/botshehadi di ka feela, tsa dula di sa fetohe kapa boholo kapa palo ya tsona ya eketseha.
Lebitso: Maqhanyatsa/dipudula sethong sa botona kapa sa botshehadi
Mofuta: Vaerase
Tlhaloso: Maqhanyatsa/dipudula Sethong sa botona/botshehadi ke STI e bakwang ke divaerase tse tshwaetsang letlalo. Ha e alafehe hore e fole empa e a alafeha.
Sesosa: Thobalano ya ka kukung, ka maraong kapa ho momonwa setho sa botona/botshehadi
Matshwao: A ka nna a se hlohlone haholo hoo a ke keng a bonahala empa hangata a hlaha e le letswabadi le le leng kapa a mangata karolong ya setho sa botona/botshehadi kapa sebakeng se potapotileng, mokoteng kapa molomong. Matswabadi a thubeha ebe a siya diso tse bohloko tse ka nkang dibeke tse 2 ho isa ho tse 4 ho fola. Lekgetlo la pele ha motho a qala ho futuhelwa ke lefu a ka ba le matshwao a kang a mofikela a jwalo ka feberu, ho ba le mahlaba mmeleng le ditshwelesa tse ruruhileng. Ho futuhelwa ho iphetapetang ha maqhanyatsa a hlahang sethong sa botona/botshehadi ho tlwaelehile.
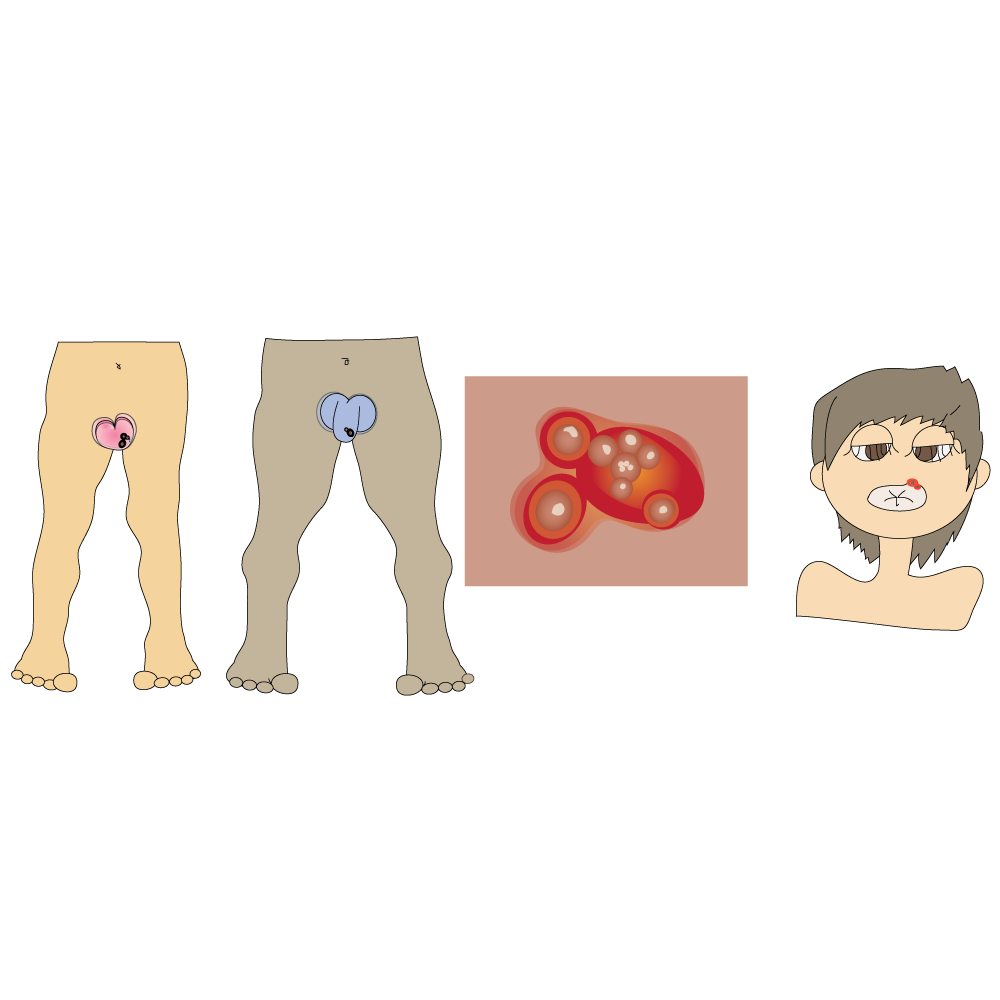
Thibelo: Tshebediso e nepahetseng le ho etswa ka mokgwa o tshwanang ya dikhondomo tsa rekere ya tlhaho e ka fokotsa kotsi ya maqhanyatsa a hlahang sethong sa botona/botshehadi, empa lefu le ka futuhela dibaka tse sa kwahelwang ke khondomo. Haeba ho na le diso, o se etse thobalano. Le ha motho a se na matshwao afe kapa afe, balekane bao a etsang thobalano le bona ba ka nna ba tshwaetswa.
Kalafo: Maqhanyatsa ha a na pheko. Meriana e thibelang vaerase e ka thibela kapa ya kgutsufatsa diphutuhelo nakong eo motho a nwang meriana.
HPV e ka etsa hore:
- Kotsi ya ho fetisa HIV e eketsehe haeba molekane ofe kapa ofe a tshwaeditswe ke HIV.
- Ho senyehelwa kapa lesea le hlahang pele ho nako.
- Tshwaetso e fetiswang ho tloha ho mme ho ya leseeng e etsang hore ho be le tshwaetso e ka etsang hore lesea le hlokahale (tshwaetso ya maqhanyatsa maseeng).
- Ho kotsi hore lesea le tshwaetswe ke vaerase ya maqhanyatsa nakong ya boimana.
Lebitso: Vaerase e Hlaselang Masole a Mmele (Human Immunodeficiency Virus (HIV)
Mofuta: Vaerase
Tlhaloso: HIV ke Vaerase e Hlaselang Masole a Mmele. Ke vaerase e ka etsang hore tshwaetso e qetelle e le Phamokate (AIDS).
Sesosa: Ka ho etsa thobalano e sa sireletsehang (ntle le khondomo) le motho ya nang le HIV. Vaerase e fetela mmeleng habobebe haeba ho na le diso (letlalo le sehilweng) tse bakilweng ke diSTI.

Ka ho tshwara madi a tshwaeditsweng ke HIV, ho etsa mohlala:
- ho sebedisa dinalete tse nang le tshwaetso le batho ba bang
- mahare
- dinalete tsa metako ya dithathu
- sesebediswa sa ho seha mabadi
- phano e sa bolokehang ya madi.

Ka ho fetisa ho tloha ho mme ho ya leseeng. Ngwanana wa moimana ya tshwaeditsweng ke HIV a ka fetisetsa HIV leseeng ha a ntse a imile, nakong ya peleho kapa ha a le nyantsha letswele.
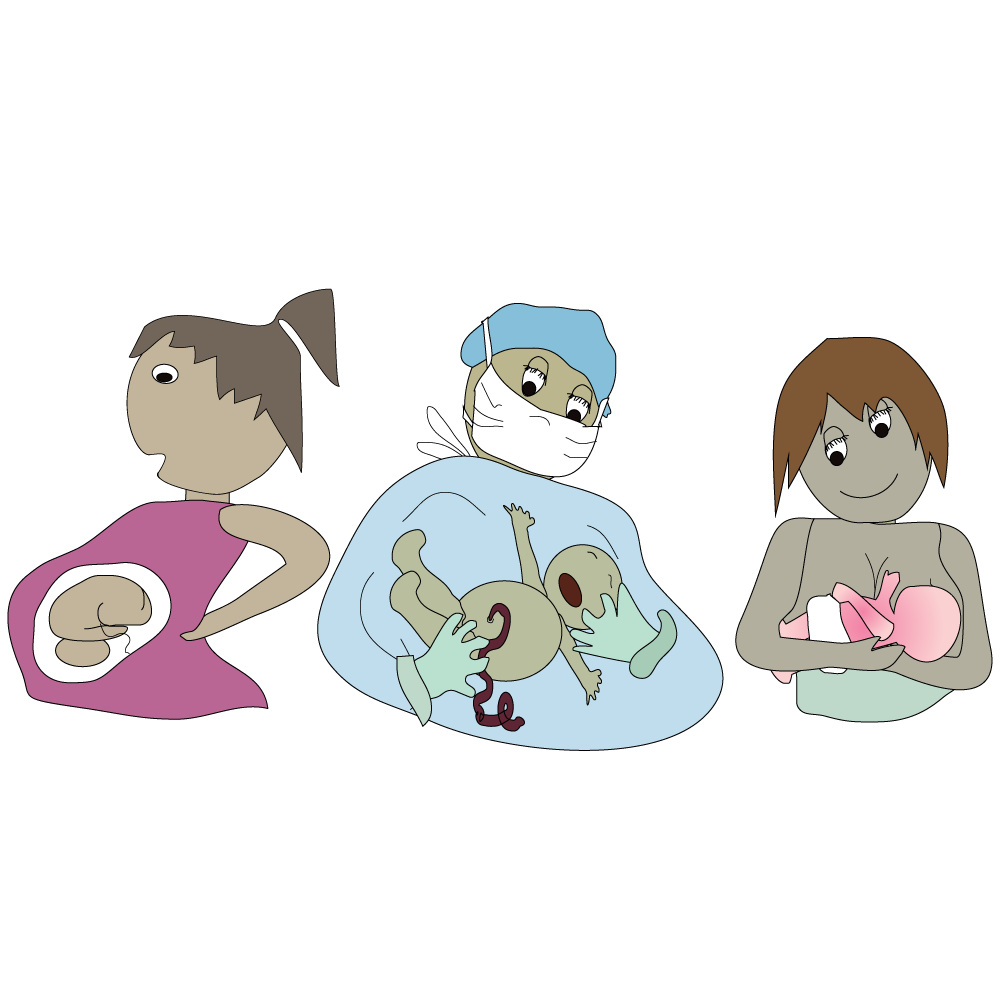
Matshwao: Dibekeng tse seng kae motho a tshwaeditswe, batho ba bang ba ba le matshwao a kang a mofikela, empa ba bang ha ba na matshwao ho hang.
Batho ba phelang le HIV ba ka bonahala le ho ikutlwa ba phetse hantle ka dilemo tse ngata. Ntle le kalafo, le ha masole a mmele a ntse a fokola, mefuta e mengata e fapaneng ya mafu e qala ho hlaha.
Thibelo:
- Qoba ho tshwara madi/lero la ditho tsa botona/botshehadi tsa motho ya tshwaeditsweng.
- Tshebediso e nepahetseng le ho etswa ka mokgwa o tshwanang ya dikhondomo e ka fokotsa kotsi ya ho fetisa tshwaetso.
- Polotso ya banna e fokotsa kotsi ya hore basadi ba tshwaetse banna nakong ya thobalano ya ka kukung.
- Ho thibela ho fetiswa ha tshwaetso ho tloha ho mme ho ya ngwaneng haeba o imile.
Kalafo: Kalafo e thibelang vaerase efe kapa efe ya sehlopha sa divaerase e ka lelefatsa bophelo ba motho ya tshwaeditsweng ke HIV ho ela haufi le dilemo tse tlwaelehileng haeba e nowa ka nepo. Hore diARV di laole HIV le ho e thibela ho ikatisa, o lokela ho nwa bonyane ditekanyetso tse 19 ho tse 20. Ketso ena e bitswa ho phethahatsa ho ya ka taelo.
Ntle le kalafo: E ka etsa hore, HIV e be AIDS, boemo ba moraorao ba tshwaetso ya HIV, ha masole a mmele a imetswe haholo mme a sa kgone ho lwantsha mafu le dikankere tse ding. Kajeno, batho ba ka phela le HIV nako e ka bang e tlwaelehileng ha ba nwa diARV ka nepo.
Lebitso: Molluscum Contagiosum (MC)
Mofuta: O amanang le vaerase
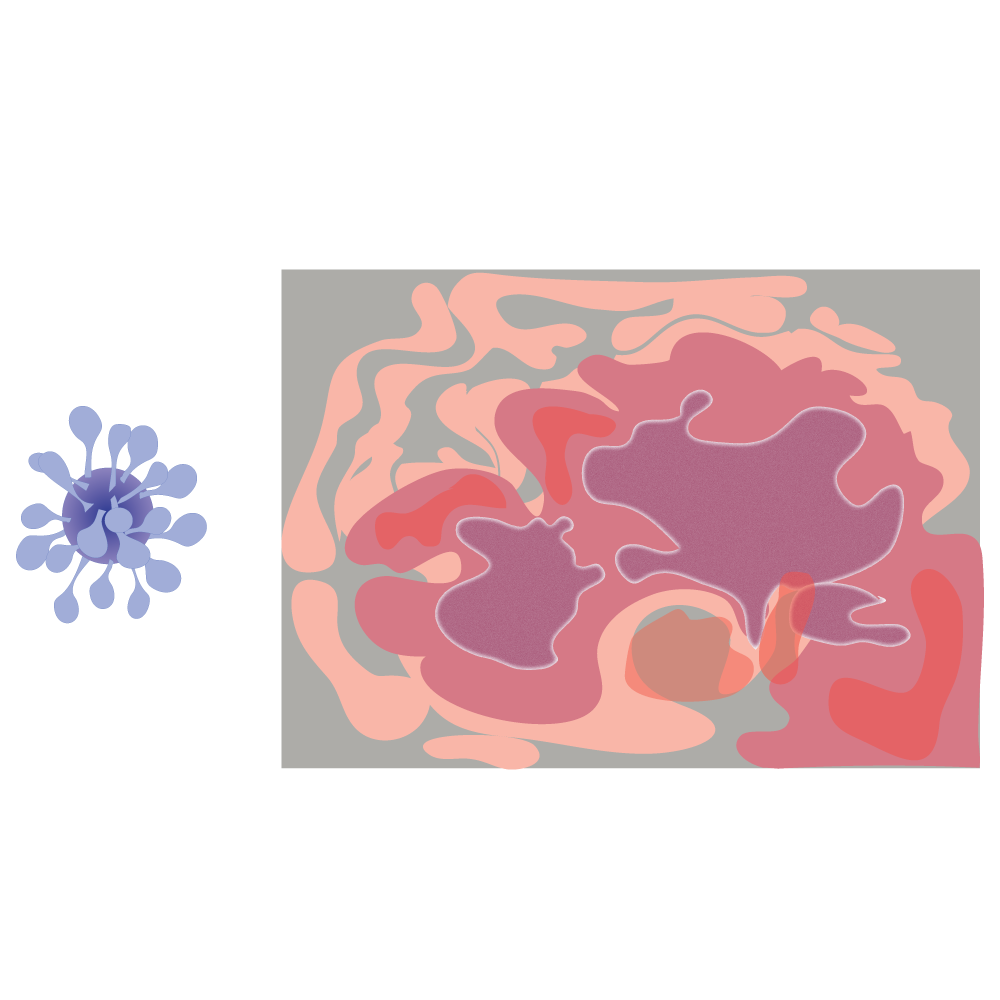
Tlhaloso: Molluscum Contagiosum e bakwa ke vaerase eo e leng setho sa leloko la divaerase tse bakang mafu a pox. O ka fumana tshwaetso ka ditsela tse ngata tse fapaneng.
Sesosa: Thobalano le ho tshwara dintho tse tshwaeditsweng, tse jwalo ka dithaole, diaparo kapa dibapadiswa.
Matshwao:
Di/kuru kapa sehloba se senyane se seng bohloko se ka beng se ruruhile, seo hangata karolo ya sona e hare e nang le sekoti se senyane sa mmala o bosweu bo sa kgahliseng.
Ho ingwaya ho etsa hore di namele dibakeng tse ding di ikentse mola ka dihlotshwana, tse bitswang dicrops, tse etsang hore letlalo le tlerefale.
E tlwaetse ho bonwa dithong tsa botona/botshehadi, mpeng le karolong e ka hare ya serope.
Maqeba (dikuru) a hlahang pele dithong tsa botona/botshehadi a ka nkwa e le maqhanyatsa kapa dihloba ka phoso, empa maqeba ana ha a bohloko jwalo ka maqhanyatsa. MC e tlwaelehile baneng ba tshwaetswang ka ho tshwara kuru ka kotloloho.
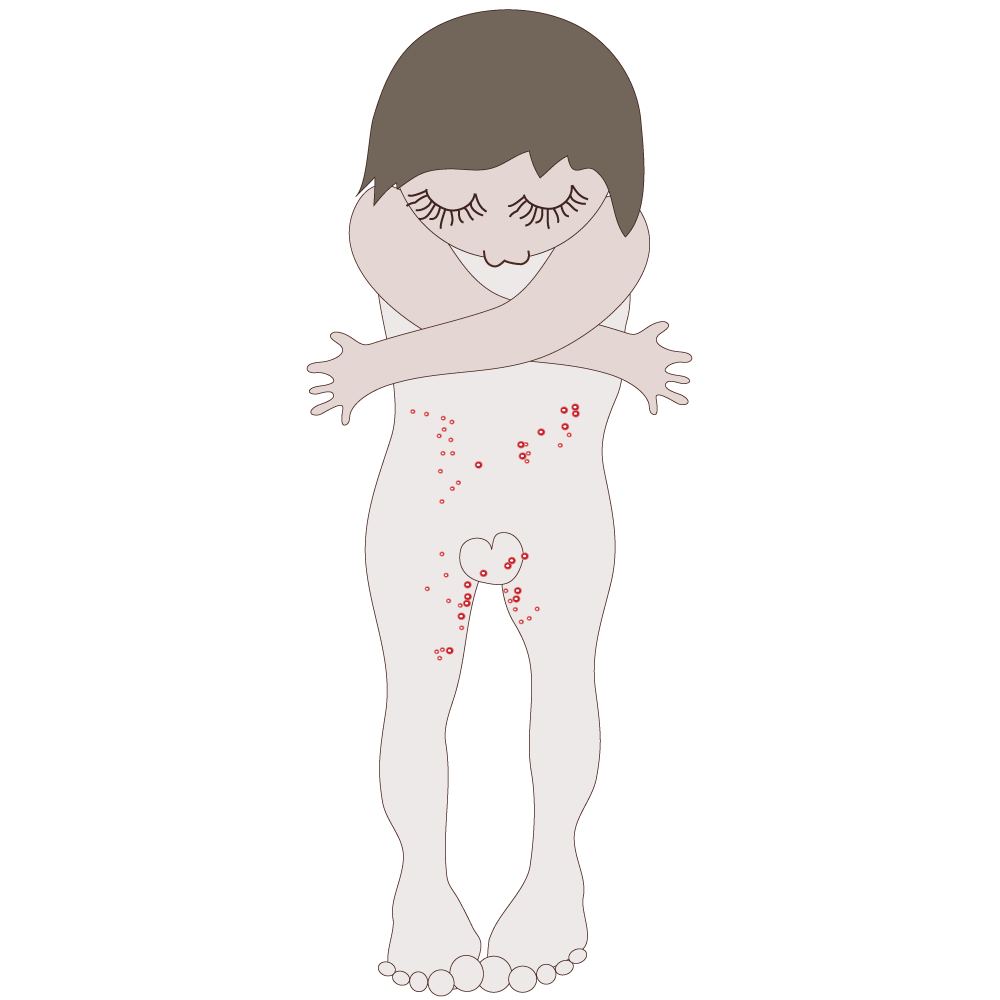
Thibelo:
- Qoba ho tshwara maqeba a letlalong.
- O se sebedise dithaole, mealo ya betheng kapa diaparo le batho ba bang.
- Ho qoba ho etsa thobalano ho ka thibela vaerase ya molluscum. Le ha ho sebediswa khondomo, tshwaetso e ntse e ka etsahala ka ho tshwara dibaka tse sa kwahelwang ke khondomo.

Kalafo: Hangata tshwaetso e tla iphella ka boyona ka mora dikgwedi tse seng kae (kapa diketsahalong tse ding e ka nka selemo kapa tse pedi) empa moo masole a mmele a fokolang, e ka mpefala.
Ho na le meriana eo mosebetsi wa tlhokomelo ya bophelo a ka fanang ka yona ho fedisa dikuru, kapa di ka tloswa ka ho sehwa, empa hona ho ka etsa mabadi.
HPV e ka etsa hore: Maqeba/dikuru le ditshwaetso tse ding tsa letlalo di ka nama le ho hlaha hape.
Lebitso: Lefu la boruruisi lesapong la noka le sebakeng sa setho sa botona/botshehadi (Pelvic Inflammatory Disease (PID)
Mofuta: Bothata bo sa lebellwang bo bang teng ka mora ho ba le diSTI
Tlhaloso: Lefu la PID ke bothata bo kotsi haholo bo sa lebellwang bo bang teng ka mora ho ba le ditshwaetso tse itseng tse fetiswang ka thobalano (diSTI). Lefu la PID le ka ntsha ditjhupu tsa fallopian le dithishu tse ka hare kapa haufi le popelo le diouvari kotsi. Lefu la PID le ka etsa hore ho be le ditlamorao tse mpe haholo, tse kenyeletsang ho hloka pelehi (ho se kgone ho ba le bana), ho ima lesea le holelang ka ntle ho popelo (boimana bo etsahalang ka hara tjhupu ya fallopian kapa kaekae kantle ho popelo) le ho ba le boladu.
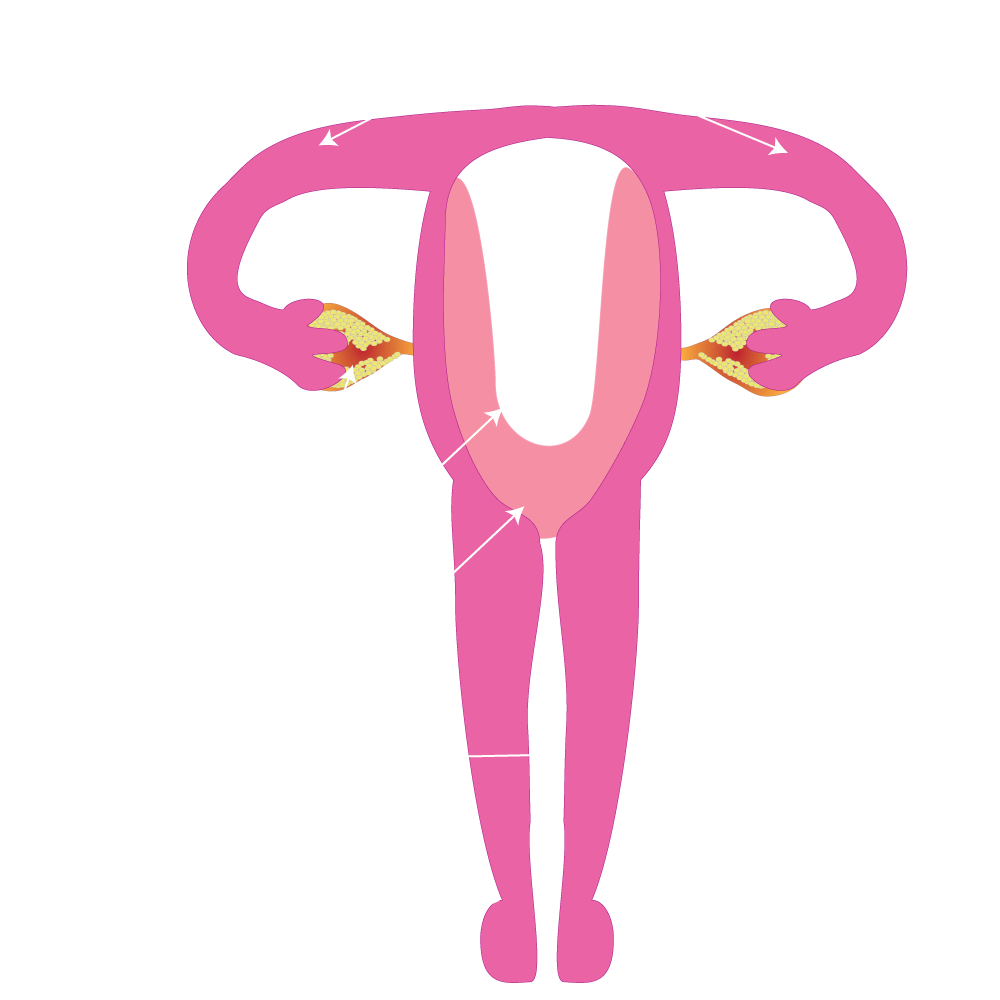
Sesosa:
- DiSTI tse sa alafshweng tse nyolohelang dithong tsa ho etsa bana.
- DiSTI tse sa alafshweng, haholoholo chlamydia le morotwana.
- Lefu la PID le ba teng ha baktheria (dikokwanahloko) di tsamaela hodimo kukung kapa molomong wa popelo (lesobeng la popelo) ho kena ka hara ditho tsa ho etsa bana.
- Banana ba sa leng dilemong tse tlase ba na le monyetla wa ho ba le PID hobane molomo wa popelo ya bona ha o e so tiye, e leng bothata bo eketsang menyetla ya bona ya ho tshwaetswa ke diSTI tse tsamaellanang le PID.
- Ha ngwanana a ba le balekane ba bangata ba thobalano, kotsi ya ho ba le PID e kgolo ka lebaka la kgonahalo ya ho kenwa ke mafu a tshwaetsang.
- Banana ba hlapang kuku ka hare ka metsi kapa metswako e meng (Lereo la Sefora le bolelang ho 'inela’ hoo e leng mokgwa wa hlapa kuku ka hare) ba ka ba le kotsi e hodingwana ya ho ba le PID.
Thibelo:
- Thobalano e bolokehileng.
- Tlhahlobo le kalafo ya diSTI.
- Qoba ho hlatswa setho sa bosadi/kuku ka hare.
Matshwao:
- Matshwao a lefu la PID a ka fapana ho tloha ho a seng kotsi ho ya ho a leng kotsi haholo.
- Lefu la PID le bakwang ke Chlamydia le ka hlahisa matshwao a seng kotsi haholo, le ha ditjhupu tsa fallopian le ditho tsa ho etsa bana di se di tswile kotsi.
- Hangata banana le bafani ba tlhokomelo ya bophelo ha ba bone ha lefu la PID le le teng.
- Letshwao le tlwaelehileng haholo ke ho ba le lehlaba tlase mpeng.
- Matshwao a mang a kenyeletsa feberu, lero la kuku le sa tlwaelehang le ho ka ba le monkgo o mobe, ho utlwa bohloko ha ho etswa thobalano, ho utlwa bohloko ha motho a ntsha metsi, ho ya kgweding/matsatsing ho sa tlwalehang, le lehlaba hodimo lehlakoreng le letona la mpa
Kalafo: Lefu la PID le ka alafshwa ka mefuta e mengata ya dianthibayothiksi, empa ha di kgutlisetse kotsi e seng e etsahetse morao.